eISSN: 2377-4304


Case Report Volume 14 Issue 5
Clinical Doctor in Uruguay, Diploma in Bone and Metabolic Diseases, Autonomous University of Baja California: UABC, Mexico
Correspondence: Dr. Edgardo Romero Galván, Clinical Doctor in Uruguay, Diploma in Bone and Metabolic Diseases, Autonomous University of Baja California: UABC, Mexico, Certificate in Bone Densitometry, AMMOM, Mexico
Received: October 03, 2023 | Published: October 13, 2023
Citation: Galván ER. Osteoporosis and vertebral fractures in postmenopausal women. Obstet Gynecol Int J. 2023;14(5):145-150. DOI: 10.15406/ogij.2023.14.00713
Osteoporosis is a chronic bone disease, with a high incidence in post-menopause, up to 50% in women over 70 years of age, with an enormous impact on public health and great morbidity and mortality. There have been notable advances in diagnosis and especially in treatments, but fragility fractures continue to increase, both vertebral and hip fractures. The former are still underdiagnosed and undertreated; the objective is to prevent them in all postmenopausal women and improve quality of life.
Keywords: osteoporosis, vertebral fractures, bisphosphonates, denosumab, romosozumab
Osteoporosis is a systemic skeletal disease characterized by low bone mass and deterioration of the microarchitecture of bone tissue, causing an increase in bone fragility with a consequent increase in the risk of fractures. In this definition we have a qualitative concept of architectural alteration and a quantitative one related to bone mineral density (BMD). There are several factors that are related to the decrease in bone resistance, in addition to BMD, they include the rates of bone formation and resorption, the geometry of the bone, that is, its size and shape, which guides towards microarchitecture. Most postmenopausal women with osteoporosis have bone loss related to estrogen deficiency and advancing age.
The concept of low bone density refers to a decrease in bone tissue with respect to the total volume of the bone and low BMD is that which is quantified by densitometry (dual X-ray absorptiometry - DXA) of the spine and/or hip, reported as an absolute value in gs./cm2, when it is below – 2.5 standard deviations with respect to the average of the normal population, young adults, called T score (in postmenopausal women) and the Z score describes the bone mass of the patient compared to averages of people of the same age and sex (in premenopausal women) Figure 1.
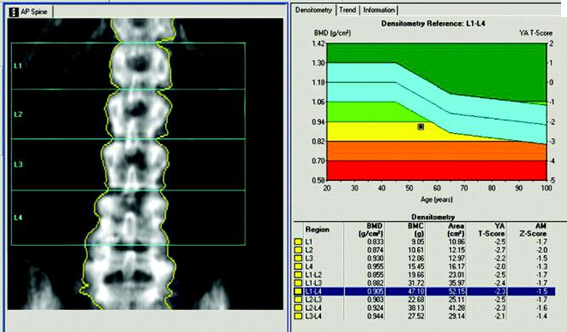
Figure 1 Densitometry of a 71-year-old patient. 0.905 grs/cm2 with a T score L1-L4: -2.3 Osteopenia. Study carried out at Centroseo by Diana Wilizanski MD, CCD/ISCD in 2019. Fracture risk calculated by FRAX: 11% for major fractures and 5.3% for hip fracture due to risk factors
The deterioration of the bone microarchitecture refers to the number and thickness of the trabeculae as well as the concentric lamellae that form both the trabecular and cortical bone, which can be evaluated by histomorphometric methods, calculating static and dynamic indices, the percentage occupied by the osteoid, the mineralized bone, its thickness and width.
The change in life expectancy, older people, has led to an increase in the incidence of pathologies of old age such as osteoporosis. In the USA alone, this pathology affects more than 10 million people, it is estimated that by 2030 it will increase to 14 million and worldwide it is estimated that about 200 million people suffer from it, calculating that the costs of care for patients with osteoporotic fractures in the USA by the year 2040 would be 50 billion dollars, knowing that the risk of fractures due to osteoporosis during life in women is 40 to 50% and in men it is up to 22 to 25%.
In the USA, 700 to 750 thousand vertebral fractures occur per year due to osteoporotic causes, compared to 250 thousand hip fractures and in Europe more than 810 thousand vertebral fractures and 400 thousand hip fractures. There is an erroneous perception that, despite being more common, spinal injuries have fewer consequences than hip injuries, but they have the same devastating effects in terms of decreased quality of life, decreased independence, and increased morbidity and mortality. 20% of patients who present a vertebral fracture die within one to five years.
The FIT study showed that both hip and vertebral fractures were associated with an increase in mortality and authors such as Cyrus Cooper1 demonstrated that the survival rate (SV) was lower than that of healthy people and similar to that of healthy people. SV after hip fracture. Another point to highlight is that only 1/3 of vertebral fractures (VF) receive medical attention (2/3 are not treated), they are underdiagnosed;2 It is important that a timely diagnosis be made because the presence of a vertebral fracture increases the risk of subsequent fractures; A VF predisposes 4.5 to a new VF and 2.3 to a hip fracture.
VFs occur spontaneously or from minimal trauma during daily activities such as lifting objects, bending forward, climbing stairs, creating a compressive-type load that exceeds the decreased load capacity of the osteoporotic vertebra.
Back pain or dorsalgia is the most common symptom in a vertebral fracture, it was found in only 38% in the SOF study, the absence of signs and symptoms is very common, up to 75% of VF in X-rays They can remain undetected. The pain can be severe and chronic but also mild, subsiding 6 to 8 weeks later. At the time of the fracture the pain is acute, sometimes patients report only “tiredness in the back” which must be interpreted.
Due to the etiological complexity of back pain, it is common that an Osteoporotic fracture is not suspected and that it is often interpreted as muscle pain, such as a contracture. Another finding is the loss of height, which is usually gradual. The most frequent location of VF is in the middle region of the dorsal column T7 and T8 as well as in the dorsolumbar junction T12 - L1 as we see in Figure 2, Figure 3 and Figure 9 Many of these symptoms can become disabling. physically and psychologically due to its persistence, producing depression, social isolation and interpersonal relationship problems as well as difficulty falling asleep due to pain and depression, leading in severe cases to the loss of social identity.
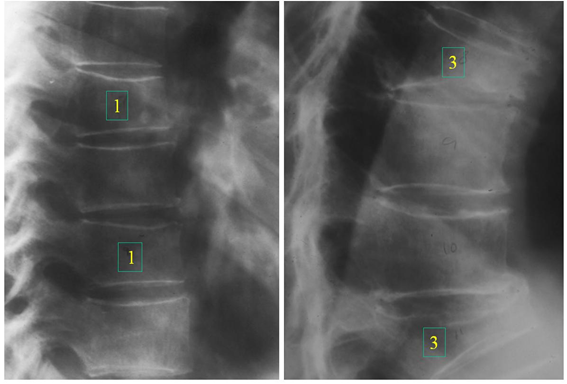
Figure 2 Vertebral fractures at level T8 and T11, numbers 1 and 3 on the radiographs show the Genant classification: 1 mild and 3 severe.
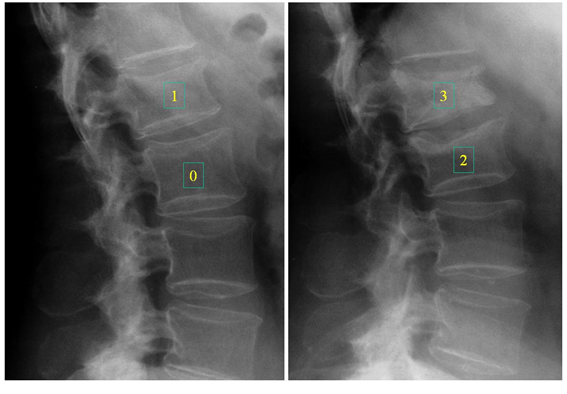
Figure 3 Lumbar vertebral fractures, the number 0 is normal, 1,2 and 3 show different VF (Genant Classification).
Any patient with a VF, regardless of the result of the Densitometry (osteopenia), should be treated and considered osteoporotic.
Other compromises have been detected in VF such as a decrease in lung capacity (restrictive insufficiencies) as well as a decrease in respiratory function of up to 10% and even greater if it coexists with previous defects such as Chronic Obstructive Pulmonary Disease, Asthma.
The diagnosis of osteoporosis causes a feeling of old age in women and when presenting a xiphosis accentuated by VF it causes ugliness, anxiety, low self-esteem, induces fear of falls with hip fractures and fear of losing independence, hence the importance early diagnosis and avoid reaching these clinical stages.
These locations correspond to the most mechanically compromised regions of the spine: mid-dorsal region where the dorsal xiphosis is most pronounced during spinal flexion and the dorso-lumbar junction, where the thoracic spine is somewhat rigid connecting with more mobile lumbar segments. An indicator for searching for VF is height loss of 3 to 5 cm. The EVOS study showed a strong relationship between vertebral deformities due to fractures and height loss of at least 5 cm. Another valuable clinical sign is the prominent dorsal xiphosis Figure 4 that manifests multiple VFs, especially with collapse of the anterior edge.
Types of fractures: to confirm the diagnosis, the radiograph must clearly identify the contours of the vertebral bodies to evaluate the decrease in any of the vertebral heights or break in the cortical edge and classify as wedge, biconcave or crushing Figure 5.
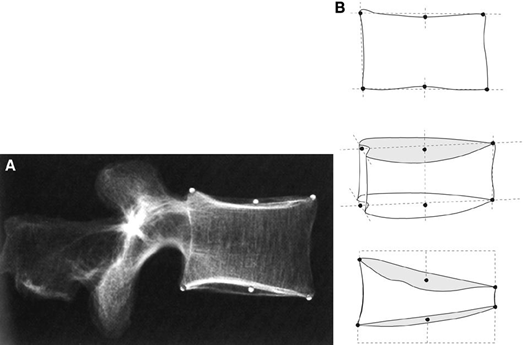
Figure 5 Placement of 6 points that delimit the vertebral borders and define anterior, middle and posterior height.
Wedge fractures are due to a collapse of the anterior or posterior edge of the vertebral body, more frequently the anterior edge as seen in number 3 in Figure 2.
Biconcave fractures are produced by collapse of the central portion of the vertebral body Figure 6, and crushing is when the entire vertebral body has collapsed Figure 7.
Different methods were described to evaluate VF, already in 1947 Fletcher proposed a “wedging index” to describe the variations of anterior vertebral heights and in 1960 Barnet and Nordin described the “biconcavity index” as the ratio of the average vertebral height and the anterior height calculated in a lumbar vertebra and its value of 0.8 was indicative of osteoporosis, but has fallen into disuse since it correlated poorly with Densitometry. Detailed descriptions of the measurements of vertebral heights are due to Hurxthal in 1968 to evaluate coinages. Other semiquantitative methods were described: Smith's method, Meunier's method classifying into grades 1,2 and 3 (normal vertebra, biconcave and collapsed) and even calculated the RVI (radiological vertebral index); the Kleerekoper method modified the IRV and introduced SDV (vertebral deformity score) based on the type of deformity and finally Henry K. Genant3 developed his method of evaluating VF by visual inspection and the degree of reduction of vertebral heights , differentiate deformities because a deformity is not always a fracture but a VF is always a vertebral deformity. Figure 8. differentiate deformities because a deformity is not always a fracture but a VF is always a vertebral deformity. Figure 8. differentiate deformities because a deformity is not always a fracture but a VF is always a vertebral deformity. Figure 8.
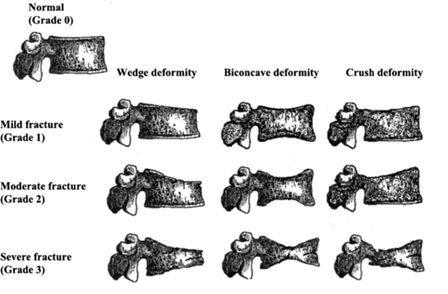
Figure 8 Genant method classifying the different wedge, biconcavity and compression VF into mild, moderate and severe (grades 1,2 and 3). (From Henry Genant).
Grade 1 has a previous height reduction of 20 to 25% and an area reduction of 10 to 20%, moderate (grade 2) of 25 to 40% and area reduction of 20 to 40%, severe (grade 2). grade 3) of more than 40% at any height and area. This method has been evaluated and tested in different epidemiological studies and clinical studies with drugs. In Figure 3 the number 0 is normal, 1 corresponds to grade 1, mild; the number 2 to a grade 2 and 3 to a severe Genant grade 3, is calculated from the “vertebral deformity index” P: length of the posterior wall, A: length of the anterior wall, therefore: PA/P x 100 = % that P is less than A. With this method, the IFC (spinal fracture index) can also be calculated by adding all the grades assigned to the vertebrae and dividing by the number of vertebrae.
These different methods evaluate VF by quantitative morphometry and measurements currently use digitalized procedures.4
When morphometry is performed in lateral dorsolumbar radiology, it is known as MRX (radiographic vertebral morphometry), using the 6 points to determine anterior, middle and posterior heights as we see in Figure 5 and the “wedging indices” are used. “biconcavity index” and the “compression index”; leading to the definition of VF: as a percentage of decrease between 15 to 20% in their height or decrease in their indices as mentioned by J. Melton.4 Other authors such as Eastel, Mc Closkey and Minne have proposed other definitions, slightly modifying the previous ones.5–7
Another method has been developed, MXA (vertebral morphometry by absorptiometry) performed with Densitometry equipment, in the Lunar equipment known as LVA (Lateral Vertebral Assessment) or VFA and in the Hologic, IVA (Instant Vertebral Assessment), allowing to obtain an image simple and efficient of the entire spine and with less irradiation than a conventional X-ray Figure 9.
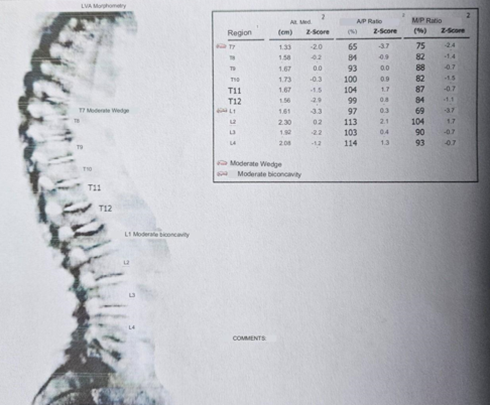
Figure 9 VFA of an 82-year-old patient where a biconcave vertebral fracture of T12 and L1 is confirmed. Study carried out by Diana Wiluzanski MD, CCD at Centróseo de Montevideo, 2023.
There are studies that correlate MXA with MRX, as carried out by JA Rea et al. demonstrating that MXA is more effective in identifying moderate to severe deformities with a sensitivity of up to 81% to identify grade 2 deformities, therefore MXA has advantages compared to MRX, it radiates less, the acquisition of the entire spine in one single image and lower cost.
As we have mentioned, there is an increase in the risk of VF with age, but up to the age of 65, VF is more common in men than in women, as demonstrated in the EVOS Study (European Vertebral Osteoporosis Study) where 15,570 men and women are evaluated. in 36 centers in 19 countries.8,9
The LAVOS Study in Latin America shows that the VF defined by MRX in a group of 400 women over 50 years of age in Mexico are similar to those found in Caucasian populations in the USA in the SOF study. Argentina, Brazil, Colombia, Mexico and Puerto Rico participated in LAVOS; It is found that only 30% of VF manifest clinically, there is an underdiagnosis and the prevalence was 14.8% for Brazil, 12.1% for Puerto Rico and 19.5% for Mexico compared to 25% in USA.10
Treatment
Osteoporosis does not present clinical manifestations until a fragility fracture occurs. This is an important fact because many patients without symptoms incorrectly assume that they must not have osteoporosis. The treatment of osteoporosis consists of lifestyle measures, such as exercise and adequate dietary calcium, as well as pharmacological therapy.
In the case of any patient who consults for back pain, of abrupt onset and without a history of significant trauma, thinking that we may be facing an osteoporotic VF, we must confirm by MRX and MXA with DXA.
The use of analgesics is mandatory, but the most important thing is the underlying treatment of Osteoporosis to avoid new fractures. The treatment is based on the use of antiresorptives such as Bisphosphonates (BPs) that have analgesic effects. The third generation ones report results especially in pain and it is confirmed in multicenter studies that these drugs reduce the risk of VF by up to 70%. % as Zolendronate in the Horizon PFT (Pivotal Fracture Trial) study Figure 10.11
65% for Risedronate in the VERT study (VERT-NA and VERT-MN)12 and 62% for Ibandronate in the BONE study.13
Bisphosphonates can accumulate in bones, in osteoclasts, so after a period of treatment, lower risk patients can be offered a period without pharmacological therapy (vacation) although with adequate calcium intake and normal levels. of vitamin D3.
In recent years, with the advent of Monoclonal Antibodies, we have Denosumab, a human antibody that acts by blocking the RANK ligand of the Osteoblast, preventing its union with the RANK of the Osteoclase, an effect similar to that of Osteoprotegerin physiologically and in this way stops all osteoclastogenic activity. 60 mg subcutaneously is prescribed every 6 months. The FREEDOM Study recruited 7,868 women with postmenopausal osteoporosis between 60 and 90 years old from 214 centers. The results show an increase of more than 20% in bone density at the lumbar level, which translates into a 68% decrease in VF14 and a reduction in the incidence of new fractures at 36 months Figure 11.
The effects of Denosumab are not maintained when the treatment is suspended, the gain obtained in BMD falls rapidly, so we do not interrupt it for several years and in this way we avoid cascade vertebral fractures, aggravating the clinical situation.
The last biologic approved for Osteoporosis, Romosozumab, which It is a humanized antibody for subcutaneous administration, 210 mg once a month in 2 separate injections of 105 mg each for one year. It has a dual effect on bone remodeling, inhibiting Sclerostin and secondarily inhibiting RANKL, producing a rapid but transient increase in bone formation (osteoforming) associated with a more sustained decrease in resorption time. As a consequence, there is a marked increase in BMD and a decrease in the risk of fractures (Figure 12).
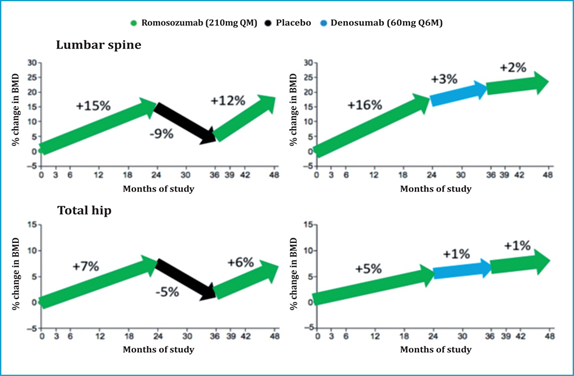
Figure 12 Sequential Romosozumab treatment after a 2-year cycle followed by Denosumab increases bone mineral density in the lumbar spine and hip.15
The effect of Romosozumab on bone remodeling is reversible, and its discontinuation is accompanied by a normalization of formation and a rebound effect of resorption, which translates into a rapid loss of BMD in both the lumbar spine and the hip.
The prior administration of Alendronate seems to mitigate this rebound effect and attenuate the loss of BMD.16
The different treatments with BPs, with Denosumab or Romosozuab, should be associated with the appropriate dose of Calcium and Vitamin D3 prior to determination and calculation of the dose according to the blood level, as well as encouraging physical mobility.
For in women, a clinical fracture risk assessment (FRAX) is appropriate in menopause and DXA should be requested in all women aged 65 years or older and in younger women if they have any risk factor that reduces BMD such as being underweight, previous fractures. (Colles fracture), use of corticosteroids and diseases that are associated with loss of bone mass (Celiac Disease, Hyperthyroidism).
TheVertebral Fractures commonly go unnoticed by the patient and the doctor. Every postmenopausal patient over 60 years of age should be evaluated for evidence of vertebral fractures. Height loss of more than 2 cm, acute back pain, and increased syphosis may be due to a vertebral fracture. A bone densitometry with a T score in Osteopenia plus a VF treat the patient as osteoporotic.
This review ends with a clinical case that came to the clinic in November/2011: a 75-year-old patient with intense back pain of 5 months' duration, without previous trauma, who had been treated with 5 tablets per day of Ibuprofen 400. mgrs. unanswered. She had no personal history of hip or Colles fracture and her physical examination highlighted her marked dorsal xiphosis Figure 13 and abdominal depression. The lateral X-ray of the dorsal spine confirms wedged and crushed vertebrae (arrows) due to osteoporosis Figure 14. Treatment with Bisphosphonate is started, 1 intravenous ampoule of Zolendronate is indicated to be administered in 15 minutes, after evaluation of renal function through a Creatinine Clearance, 1500 mg of Calcium and 1000 IU of vit are associated. D3. A week after starting the treatment, the patient experienced improvement in her pain, without the need for the high doses of Ibuprofen that she had been ingesting.
My special thanks to Diana Wiluzanski from Centróseo de Montevideo for her collaboration in DXA to my patients. I am grateful to be a Member of SIBOMM, AMMOM, SECUAMEM.
None.
Author declares that there is conflict of interest.

©2023 Galván. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.