eISSN: 2377-4304


Short Communication Volume 7 Issue 3
AIMST University, Malaysia
Correspondence: Yu Chye Wah, Faculty of Allied Health Professions, AIMST University, Malaysia, Tel 604-4296104, Fax 604-4298009
Received: October 31, 2016 | Published: June 21, 2017
Citation: Hai CH, Wah YC. The therapeutic logic behind various forms of pelvic floor support. Obstet Gynecol Int J. 2017;7(3):254-256. DOI: 10.15406/ogij.2017.07.00248
Pelvic floor muscle can be weakened by many causes and this contributes to sagging of pelvic floor, and lead to pelvic floor disorder (PFD). There are various forms of pelvic floor support available in modern medicine; each has its own therapeutic logic behind its use. The non-invasive mechanical device bowel aid with Hai’s Perinatal Support (HPS) offers supplementary support to pelvic floor muscle, facilitate defecation and prevent descend of pelvic floor. This mechanical support is promising to provide a better prognosis for patients on reconstructive pelvic mesh and sling surgery to alleviate their complications.
Keywords: Pelvic floor, Pelvic floor support, Pelvic floor disorder, Constipation, Mesh and sling surgery
HPS, Hai’s Perianal Support; PFD, Pelvic Floor Disorder; PFME, Pelvic Floor Muscle Exercise; POP, Pelvic Organ Prolapse; UI, Urinary Incontinence
A healthy pelvic floor support is essential for normal functioning of urinary and reproductive system as well as normal defecation function. Pelvic floor can be weakened by many causes; the common causes include childbirth, obesity, old age and the associated straining of chronic constipation. The weakened and sagged pelvic floor will lead to pelvic floor disorder (PFD). Manifestations of PFD are wide, they include urinary and anal incontinence,1 pelvic organ prolapse (POP),2 obstructed defecation, frequent UTI, constipation, sexual dysfunction, chronic pain syndromes and associated problems like hemorrhoid.3-5 PFD symptoms are strongly associated with female gender.6 It was estimated that 1 in every 3 women who have delivered a baby will experience PFD and 50% over 50 years old will suffer POP.7 46.2% of women would have some major PFD in their life.6
How pelvic floor is weakened and lead to wide variety of clinical conditions? For instance, overstretching of pelvic floor by baby head as in second stage of delivery may cause perineal tear. Stretching of pudendal nerve as in descended perineal syndrome causes pain in perineum. Majority of constipation is obstructive type secondary to sagged pelvic floor especially the posterior portion or the anococcygeal region.7,8 As a result of chronic repeated straining, venous dilatations of the haemorrhoidal plexus occur due to abnormal downward displacement of vascular anal cushions can lead to symptoms of hemorrhoid.9 Overstretching of anal mucosa and tearing cause anal fissure and chronic repeated process of overstretching prevent normal healing, and contribute to chronic anal fissure which is mainly located at 6 o’clock position.10 Urinary incontinence is due to weakened pelvic floor support at bladder neck area. A study found pelvic floor of healthy, nulliparous women descends by 3 cm during normal defecation.11 The descent logically deteriorates in those with weak pelvic floor support and straining because of constipation. With aging the situation would gradually worsen. In short, weakened pelvic floor support and sagging pelvic musculature play an important role in pathogenesis of various diseases in pelvic floor area. Hence, the solution of the problem is to strengthen or supplement and protect the pelvic floor support. There are various forms of pelvic floor supports available in modern medicine which is not well noticed by many.
Exercise
Kegel exercise or Pelvic Floor Muscle Exercise (PFME) aims to improve strength of pelvic floor musculature and provide support to prevent further visceral descent. It has been used to treat and prevent urinary and fecal incontinence since 1920s within the British physical therapy profession.12 Several studies have confirmed that PFME is effective in the treatment of female stress (SUI) and mixed urinary incontinence and therefore is recommended as a first-line therapy.13-15 Studies also found patients who have participated in a series of pelvic floor muscle exercise experienced improvement in sexual desires.16,17
Manual support
Mechanical support
Bowel aid, a special toilet seat with additional protrusion (Hai’s Perianal Support -HPS) (Figure 1) provides pelvic floor support and acts as mechanical laxative to facilitate smoother defecation and successfully prevent anal tearing20 and heal chronic anal fissure and significantly benefited hemorrhoid patients.21,22
Surgically reconstructed support
Autologous pelvic floor: Reconstructive surgery by just repairing weaken pelvic floor without implant. Lavatory plasty is a reconstructive surgery to strengthen lavatory plate (main component of pelvic floor support system) is found to benefit wide range of pelvic floor related problem including constipation.23
Reconstructive pelvic floor with sling or synthetic mesh: Sling surgery and mesh implantation is indicated for urinary incontinence (UI) and pelvic organ prolapse (POP) respectively to strengthen part of pelvic floor support system.
In relation to surgically reconstructed support, sling surgery and mesh implantation are recommended as gold standard surgery to be effective in treating urinary incontinence and POP symptoms. But these surgeries are now facing largest medical complications in medical world. There are hundreds of thousands of such procedures performed in USA so far and thousands of them end up in complications and lawsuits.24,25 This has raised the concern for public about the safety of surgical procedures in treating POP.
Why for sling surgery, an evidence based intervention can end up in such a big catastrophic complication? Mesh or sling is a synthetic non-stretchable material that holds up the urethra or pelvic organ to correct the UI or POP symptoms. During defecation while the rest of pelvic floor is descended during defecation, the surgical site is loaded more then what it can hold. In early post-operative period, prognosis is usually good, but as time passed with aging and straining due to constipation, the rest of pelvic floor descend to overload the surgical site. The synthetic material does not fail to support but only the supported site gradually erode and migrate and cause excruciating pain when the synthetic material touch the nerve plexus. This has led to world largest medical complications, involving billion dollar lawsuit. The worse is yet to come, as urogyn ecologists are yet to find a reliable solution. Reconstructive surgery with sling and mesh for UI and POP are based on similar concept to strengthen anterior and middle segment of pelvic floor support that responsible for pathogenesis of UI and POP. The associated chronic constipation which is due to weakness and sagged posterior part of pelvic floor remains uncorrected. The prognosis of the pelvic floor reconstructive surgery should be better if straining during defecation and the loading of surgical site can be prevented. This is based on well accepted old concept of supplementary support to prevent overloading of reconstructed support: Orthopedic surgery for lower limb would face the similar scenario as sling surgery for UI if there are no crutches or walking aid to provide supplementary support to allow optimal healing of surgical site (Figure 1).
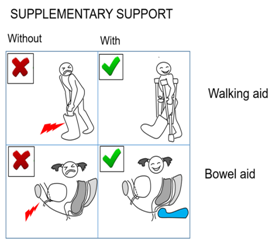
Figure 1 Supplementary support of post orthopedic reconstructed surgery of lower limb with walking aid and Hai’s perianal support (HPS) of bowel aid for obstructed constipation.
Priority is not to prove which modality is better, combination of the entire different pelvic floor supports should be explored for optimal result. Conservative measures should be well instituted before consider invasive surgery. Orthopedic surgeon has been doing reconstructive surgeries with great success. After the fracture of lower limb, typically, the reconstructed site heals so well and finally the lower limb could support the whole body weight without residual problem. Crutches or walking aid are used after orthopedic reconstructed surgery of lower limb (e.g.: tibia plating), to provide supplementary support for optimal healing of surgical site. However, compare to sling or mesh surgery for UI and POP, the surgical site is challenged repeatedly during defecation immediately after surgery.
We strongly believe it is not accurate to draw conclusion that the sling or mesh surgery fails or to totally blame implant for the complications. Evidences found so far only show support with the pelvic floor reconstructive surgery alone is insufficient to bring about recovery without complications. With supplementary pelvic floor support during defecation to prevent overloading of surgical site, pelvic floor reconstructive surgery with sling and mesh will give better prognosis and therefore very promising to be an important component in successful management for the world largest complication in history of modern medicine. As the role of a supplementary support with walking aid in post-surgical management is proven without doubt in orthopedic surgery, hence bowel aid deserves serious attention and thorough exploration, hopefully to end the patient suffering from complications, save the surgery from risk of being sanctioned and restore the dignity of surgical intervention in modern medicine.
None.
None.

©2017 Hai, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.