eISSN: 2377-4304


Research Article Volume 13 Issue 5
1Department of Obstetrics and Gynecology, Justus Liebig University Giessen, Germany
2Department of Obstetrics and Gynecology, Maastricht University Medical Centre+, Netherlands
Correspondence: Dr. Gerold Link, Department of Obstetrics and Gynecology, Justus-Liebig-University Giessen Muehlenweg 16, 52349 Dueren, Germany, Tel +49-2421-51488, +49-170- 4949238
Received: October 15, 2022 | Published: October 27, 2022
Citation: DOI: 10.15406/ogij.2022.13.00673
Objective: Ureteral injury is a typical complication in pelvic surgery even though occurring not frequently. The goal of this study was to classify the importance of perioperative assessment of serum creatinine with clinical symptoms concerning the early detection of ureteral lesions after surgery.
Patients and methods: The postoperative course of 7 gynecological and 2 obstetric patients raising doubt on ureteral integrity was analyzed, retrospectively, using medical records. Clinical symptoms (urinary production, flank pain), and the temporary changes of serum creatinine (µmol/L) as well as interdisciplinary diagnostic and interventional procedures were recorded. Glomerular filtration rate (GRF) was calculated using CKD-EPI formula (mL/min/1.73m2). Data analysis was done using descriptive statistics, Fisher’s exact test, non-parametric tests, and regression analysis (SPSS).
Results: 6/9 patients presented with ureteral impairment. In 5/6 patients unilateral (n=2) and bilateral (n=3) obstructions were detected all deriving from anterior colporrhaphy. 1 patient exhibited ureteral kinking healing spontaneously. In patients affected by ureteral obstruction diminishing of urinary outflow occurred significantly earlier than flank pain (2.8±1.0 vs. 28.8±9.2 hours, p=0.03). Mean increase in serum creatinine and decrease of GFR was from 72±16 before surgery up to 160±34 and from 79±18 down to 30±6 (p=0.07), respectively, within 8–48 hours after surgery being significantly different from respective values in patients without obstruction (p=0.03). The increase in creatinine in patients with unilateral obstruction followed a logarithmic graph indicating interference between deteriorated ipsilateral and functionally compensating contralateral kidney after 24 hours.
Conclusion: Perioperative measurement of serum creatinine is useful in testing ureteral integrity. However, the negative predictive value is superior to the positive predictive value. According to decreasing GFR highly important is a contemporary registration of the urine outflow in the first hours after surgery.
Keywords: pelvic floor surgery, ureteral injury, creatinine, urinary outflow, anterior colporrhaphy, glomerular filtration rate, chronic kidney disease, urogynecology
Ureteral injury is a characteristic complication in pelvic surgery. However, it doesn’t occur frequently. Due to the close neighborhood of the ureter to the female pelvic organs, many gynecologic and obstetric surgical procedures include the risk of ureteral damage, especially in operations involving invasive cancer and urogynecological procedures.1 The incidence of ureteral injury in gynecologic interventions is reported to range between 0.1% to 1.5% in benign cases and up to 5% in patients undergoing surgery because of malignancy.2 Moreover, 75% of all iatrogenic ureteral injuries derive from gynecological surgeries.3 Frequently, the ureteral trauma is not recognized during the surgical event but several days later. Only a third of these injuries are detected at the time of surgery.4
Currently, with few exceptions (uterosacral ligament suspension [USLS], tension free vaginal tape [TVT]), there is no generally accepted requirement to perform cystoscopy during common gynecological procedures. Intraoperative cystoscopy with visualization of ureter ostia by intravenous administration of indigo carmine, although sensitive in 97% of cases, does not capture the detection of ureteral obstruction that develops in the early postoperative period due to tissue changes such as edema around the ureter or the formation of a hematoma.5 Furthermore, cystoscopic evaluation of the ureters at the end of the procedure is technically demanding and sometimes requires relevant additional time. In consideration of the already very low incidence of ureteral damage, many gynecologists therefore refrain from intraoperative testing of ureteral patency.
Typical clinical symptoms of ureteral injury include renal colic in terms of flank or groin pain, fever, abdominal mass (urinoma), prolonged ileus and finally, irreversible renal damage within 1 to 6 weeks.6 Apart from the fact that only 50% of patients develop symptoms at all, they usually appear only in a broad time slot of one week postoperatively.7 Therefore, although early detection is desirable in any case, the dramatic clinical phenomena do not lend themselves to a prompt diagnosis of ureteral damage after surgery.
To get out of the diagnostic difficulty, an attempt was made to provide a simple method to confirm the integrity of the ureters in the early postoperative period, especially if cystoscopy has not been used during the surgical procedure. Some reports in the literature recommend an evaluation of postoperative serum creatinine levels as an early reliable criterion of normal bilateral renal function.5,8–10
The objective of the present study was to adjust the role of postoperative determination of creatinine in serum with other clinical clues and imaging techniques concerning the earliest possible detection of ureteral damage after gynecologic and obstetric surgery. This may provide a guide as to whether routine creatinine determination should be included in postoperative monitoring.5
This is a retrospective study of nine patients giving doubt about the integrity of the ureter after gynecologic or obstetric surgery. Urogynecological surgery had occurred in 6 cases, tumor debulking in 1 case, and cesarean section in 2 cases. Using the medical documentation in the medical record, the postoperative course was retrospectively analyzed. A positive vote (AZ 169/22) was given by the Ethics Committee of the Department of Human Medicine, Justus Liebig University, Giessen, Germany.
The study design concerning the attribution of ureteral injuries with surgical procedures and interventions is shown in Figure 1. A potential postoperative lesion of the ureter, which was an item in 9 patients after surgery, was confirmed in 6 patients, all of whom were treated with anterior colporrhaphy, usually in addition to other surgical measures.
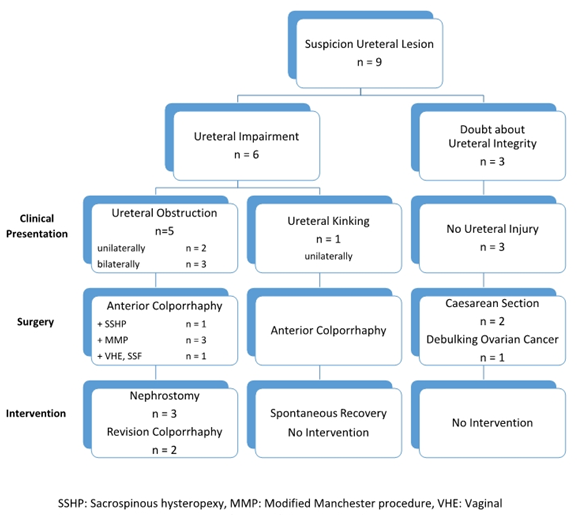
Figure 1 The split of the analyzed patients with doubt about the integrity of the ureter. Out of 9 patients, impairment of the urinary tract pathways was present in 6 patients. Common to all these cases was a preceded colporrhaphy. In 1 patient, there was only harmless ureteral kinking, which normalized spontaneously. In the 5 other cases ureteral obstruction was detected (2x unilateral, 3x bilateral). Necessary revision was performed 3x by nephrostomy and 2x by surgical revision of the colporrhaphy. In the remaining 3 patients, the initial suspicion was not confirmed.
In 5/6 cases, imaging and cystoscopy demonstrated obstruction of one or both ureters (2x unilateral, 3x bilateral), which forced intervention: in 3 patients, transcutaneous unilateral or bilateral nephrostomy was performed; in 2 cases, the sutures of the anterior colporrhaphy were released, subsequently creating a new plication of the pubocervical fascia under protection by a retrogradely inserted DJ catheter.
In 1/6 case with ureteral lesion, unilateral kinking was the cause of congestion of the left renal pelvis with flank pain. However, the planned placement of a double J catheter was not necessarily due to a rapid spontaneous healing.
In the remaining 3/9 patients, ureteral injury could be excluded (Figure 1). The primary suspicion was based on unilateral and bilateral lateral avulsion of the uterotomy in the case of the two cesarean operations, and the oncologic patient reported postoperative back and flank pain.
In addition to biometric data, clinical symptoms (decreased urine output, flank pain) and interdisciplinary diagnostic measures (renal ultrasonography, CT-assisted intravenous pyelogram [IVP], cystoscopy) and therapeutic interventions (percutaneous nephrostomy, surgical revision) were recorded.
Serum creatinine concentration was measured in the routine laboratory in µmol/L. Approximate determination of glomerular filtration rate (GFR) was performed using the Chronic Kidney Disease Epidemiology Collaboration creatinine-based formula (CKD-EPI formula) in mL/min/1.73m2.
For clinical symptoms, diagnostic and therapeutic measures, and renal parameters, the respective event times after the end of the surgical procedure and the intervention were determined.
Processing of data was performed by descriptive statistics (mean and standard deviation for characterization of samples) and nonparametric tests comparing independent and related samples (Mann-Whitney U test, Wilcoxon test) using Statistical Package for Social Sciences (IBM SPSS Statistics, software version 27). Fisher's exact test was used to analyze contingency tables because of small case numbers <5. Linear and logarithmic regression analyses were performed by the least squares method (Excel, software version 2209) to prove associations between individual parameters. A statistically significant difference or relationship was assumed at p or 2α value of <0.05, respectively.
The demographic data and diagnoses of the patients are given in Table 1. The age of the patients ranged from 28 to 80 years (53±17) with a BMI between 19 and 40kg/m2 (25.7±6.3). Significant differences between patients with and without ureteral obstruction were not existent (age: p=0.41, BMI: p=0.39). The indications for vaginal surgery were uterine procidentia (n=1) and predominant cystocele (n=5) according to POP Q stage 2 and 3. The two cesarean sections were performed because of pathology during birth, and the cytoreductive debulking in one case was due to ovarian carcinoma.
Patient no. |
Age (years) |
BMI (kg/m2) |
Preoperative diagnosis |
POP Q stage |
1 |
65 |
40 |
Cystocele |
3 |
2 |
48 |
23 |
Cystocele, Uterine Prolapse |
2 |
3 |
54 |
27 |
Cystocele, Uterine Prolapse |
3 |
4 |
28 |
19 |
Preterm Birth with BP |
- |
5 |
30 |
22 |
Term Birth with FP |
- |
6 |
68 |
28 |
Ovarian Cancer |
- |
7 |
80 |
24 |
Uterine Procidentia |
3 |
8 |
54 |
- |
Cystocele |
2 |
9 |
52 |
23 |
Cystocele, Uterine Prolapse |
3 |
Table 1 Demographic features and diagnoses of the patients
BMI, body mass index; POP Q, pelvic organ prolapse quantification; BP, breech presentation; FP, failure to progress
Postoperatively, the leading clinical symptom "oliguria and anuria" occurred significantly earlier than the symptom "flank pain" (2.8±1.0 vs. 28.8±9.2 hours, p=0.03). In all cases with decreased urine output (4/4), ureteral obstruction was subsequently confirmed, whereas ureteral obstruction could be excluded in 4/5 cases with undiminished urine production. However, in the fifth case, bilateral obstruction was demonstrated later (p = 0.04). In patients exhibiting flank pain, obstruction was observed twice (2/4) and kinking once. Conversely, despite the absence of pain, ureteral obstruction was present in 3/5 patients (p=1.00).
The time slot of additional diagnostics covered 5 to 53 (32±17) hours after surgery. A significant difference between cases with and without obstruction of the ureter (p=0.19) did not exist. Renal ultrasonography was performed in 5 patients. Congestion of the renal pelvis was detected in the case with kinking and in three cases with obstruction of the ureter. Another sonography after cesarean was correctly negative and showed no abnormality (p=0.40). The findings of CT-IVP (1x) and cystoscopy (2x) proved to be correctly positive.
Interventions in the 5 cases with proven ureteral obstruction occurred 18 to 73 (46±25) hours after primary surgery. However, the nephrostomy procedure was performed an arithmetic mean of 42 hours later than the surgical revision (63±14 vs. 21±4, p=0.20).
Perioperative serum creatinine and glomerular filtration rate (GFR) data are summarized in Table 2 according to the severity of ureteral lesion (bilateral obstruction, unilateral obstruction, kinking, no impairment).
Patient no. |
Baseline Value |
Ureteral injury |
1st Value |
Intervention |
1st Value After Intervention/2nd Value After Surgery |
|||
|
Creatinine |
GFR |
Creatinine |
GFR |
Creatinine |
GFR |
||
9 |
57 |
103 |
Bilateral obstruction |
204 |
22 |
Bilateral nephrostomy |
131 |
37 |
7 |
63 |
80 |
Bilateral obstruction |
123 |
35 |
Bilateral nephrostomy |
96 |
48 |
3 |
77 |
76 |
Bilateral obstruction |
- |
- |
Revision AC, bilateral DJ |
60 |
100 |
1 |
64 |
85 |
Unilateral obstruction |
164 |
29 |
Revision AC, unilateral DJ |
90 |
58 |
2 |
97 |
53 |
Unilateral obstruction |
148 |
33 |
Unilateral nephrostomy |
102 |
50 |
M±SD |
72±16 |
79±18 |
160±34 |
30±6 |
96±26 |
59±24 |
||
8 |
73 |
80 |
Unilateral kinking |
82 |
70 |
No intervention |
73 |
80 |
4 |
- |
- |
No ureteral impairment |
38 |
139 |
No intervention |
44 |
132 |
5 |
65 |
110 |
No ureteral impairment |
54 |
122 |
No intervention |
- |
- |
6 |
59 |
91 |
No ureteral impairment |
49 |
96 |
No intervention |
48 |
97 |
M±SD |
66±7 |
94±15 |
56±19 |
107±30 |
55±16 |
103±27 |
||
P* |
1,00 |
0,25 |
|
0,03 |
0,03 |
|
0,07 |
0,14 |
Table 2 Perioperative levels of serum creatinine (µmol/L) and glomerular filtration rate (GFR [mL/min/1,73m2]) with clinical events
AC, anterior colporrhaphy; DJ, double J catheter; M, mean; SD, standard deviation; p*, Mann-Whitney-U-Test
In the collective of ureteral obstruction, a substantial but nonsignificant increase in mean serum creatinine concentration from 72±16 to 160±34µmol/L (p=0.07) was measured in an interval of 8 to 48 (25±17) hours after the primary procedure but before the intervention. The minimum postoperative creatinine increase was 51µmol/L=0.6mg/dL (patient no. 2). Mean GFR decreased in parallel from 79±18 to 30±6mL/min/1.73m2 (p=0.07).
The analogous values in patients without intervention were measured in a comparable time frame after surgery (29±25 hours, p=1.00) and showed no significant changes. In 2/3 cases, postoperative serum creatinine concentration decreased slightly. In the one case with unilateral kinking of the ureter (patient no. 8), a small increase in creatinine was detectable (9µmol/L=0.1mg/dL) with a corresponding decrease in GFR.
However, when comparing the groups with and without intervention, a significant difference was present for both parameters at the first measurement after surgery (p=0.03).
After the intervention (15±9 hours), again a marked but also nonsignificant decrease in creatinine with a corresponding increase in GFR was again observed (p=0.07). Statistically, no significant difference between the time intervals from surgery to increase and intervention to decrease in serum creatinine existed (p=0.07).
In Figure 2, the timeline of serum creatinine and GFR was reconstructed in 2 patients with bilateral obstruction and 2 cases with unilateral obstruction as well as in the case with unilateral ureteral kinking using all available measurement data.
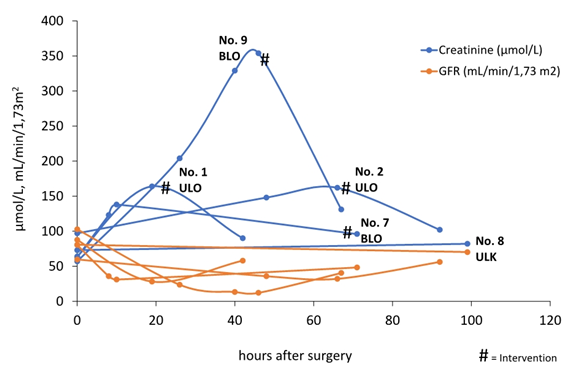
Figure 2 The changes of serum creatinine concentration and glomerular filtration rate (GFR) after primary surgery up to 1st measurement after intervention in 2 patients with unilateral (ULO) and 2 patients with bilateral obstruction of the ureter (BLO) and one patient with unilateral ureteral kinking (ULK). In the first 20 hours postoperatively, there is a steep increase in serum creatinine, which is paralleled by a decrease in GFR. The highest creatinine value is observed in bilateral obstruction (no. 9), which is followed by a steep decrease after intervention. In the patient with unilateral kinking of the ureter, only a minimal increase in serum creatinine (9 µmol/L) is present.
Within the first 20 postoperative hours, two cases with bilateral (no. 7, 9) and one case with unilateral obstruction (no. 1) experienced a steep rise in serum creatinine. In the other patient with unilateral obstruction, the rise was much flatter. The maximum creatinine value (354µmol/L) was measured after bilateral obstruction (no. 9). The postinterventional fall in creatinine was steeper in this patient than in the two cases after unilateral obstruction. Compared with the large movements in creatinine levels, the parallel inverse changes in GFR had a narrower profile. However, within the first 20 postoperative hours, a marked decrease in GFR is evident in 3/5 patients (no. 1, 7, 9).
The increase in creatinine and the consecutive decrease in GFR in unilateral kinking (no. 8) were minimal and are localized in a graph sector clearly outside the curve of cases with unilateral or bilateral obstruction of the ureter. The second postoperative creatinine value was not included in the figure because it was measured 576 hours after the procedure.
Case no. 3 with bilateral obstruction could not be shown in the diagram, too, due to lack of postoperative creatinine determination. The clinical suspicion of a ureteral lesion in this patient was due to postoperative anuria and was subsequently confirmed by cystoscopy. In the same session, 18 hours after the primary procedure, intervention was performed by revision of the anterior colporrhaphy protected by bilateral double J catheters.
For analyzing Figure 2 more in detail, the creatinine values describing the increase in serum concentration were plotted against time for the cases with unilateral (blue) and bilateral obstruction of the ureter (orange), separately (Figure 3). For unilateral obstruction, the best mathematical approximation to the values was obtained by a logarithmic function reflecting an initial steep increase in serum creatinine in the first postoperative hours with subsequent marked flattening of the curve. In bilateral obstruction, adjusting a linear regression line generated the highest correlation coefficient, indicating a steep steady increase in creatinine concentration.
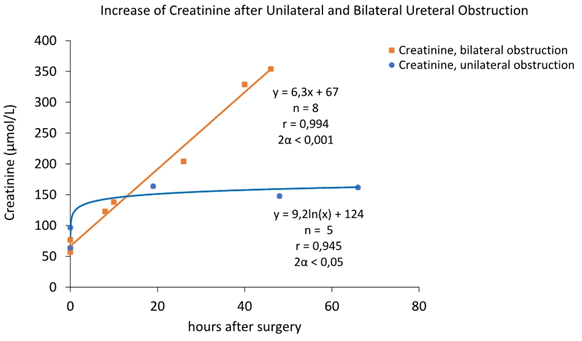
Figure 3 The increase of serum creatinine concentration after primary intervention up to the maximum value before intervention in 2 patients with unilateral and 2 patients with bilateral obstruction of the ureter. The relationship between the measured values and time after unilateral obstruction is best reflected by a logarithmic function that exhibits a steep rise in the first postoperative hours subsequently flattening out markedly. The series of measurements after bilateral obstruction are most confidently described by a linear regression line showing a steady increase in serum creatinine with time.
The risk of ureteral lesion in anterior colporrhaphy
All 6 ureteral lesions in the present study arose during anterior colporrhaphy. 5 of these patients required postoperative interventions. However, even the 6th spontaneously healed case with unilateral kinking of the ureter demonstrates the fundamental danger associated with placing sutures in the surgical layer of the septum vesicovaginale as shown by the transiently dilated renal pelvis with flank pain and the slight increase in serum creatinine. Although ureteral injuries are rare events, they are by no means uncommon in the surgical correction of pelvic organ prolapse. The combination of uterosacral ligament suspension with anterior colporrhaphy was found to be of particular risk, with a rate of ureteral occlusions of 9%.11 Kinking of the ureter was described in 6% of cases in an analysis of 161 uterosacral ligament suspensions.12 Specifically for anterior colporrhaphy, caution should be exercised when laterally mobilizing the bladder from the underlying vagina, because too radical dissection may expose the ureter resulting in ligation or kinking as the redundant tissues are plicated.13
On the other hand, the redressing effect of anterior colporrhaphy is insufficient if the cystocele is not completely exposed. In this respect, appropriate dissection, and correct placement of the plicating sutures are a challenge to the surgeon's experience. For this reason, some gynecologists prefer reconstruction of a pronounced cystocele using a mesh interposition device, even in the primary situation. However, transvaginal mesh repair can cause significant problems in individual cases, even if not in the ureter, and is therefore not recommended as a primary method in prolapse.14
The time frame of diagnostic measures and therapeutic interventions in ureteral lesions
In accordance with widespread practice, intraoperative cystoscopy was also omitted in the patients of the present study. In hysterectomy for example, routine use of postprocedural cystoscopy is under great debate because it did not prove to reduce the rate of a 30-day delayed injury.15 The diagnostic measures used to examine the ureters occurred in a postoperative time frame of 5 to 53 hours. Unless ureteral injuries are detected intraoperatively (>60%), the diagnosis is often made several days later. After caesarean section, 24 ureteral injuries were reported in 22 patients over a period of 21±50 days.16 In 7 patients after total laparoscopic hysterectomy (TLH) for benign indications, the diagnostic period ranged from 3 to 84 (25±37) days.10
Concerning the most reliable diagnostic technique, the CT scan with contrast medium has become established providing an informative value clearly superior to renal ultrasound. Nevertheless, renal sonography is usually used as the first measure because of its permanent availability and safety. As a rule, however, no physician will decide on invasive therapy based on renal ultrasound alone.
The therapeutic interventions occurred a mean of 14 hours following the diagnosis of obstruction between 18 and 73 hours after the primary procedure. With respect to the interval to therapeutic intervention, a time slot consistent with the present data was reported from a procedure because of obstruction of a solitary kidney ureter, which was relieved 51 hours after previous caesarean section by re-laparotomy with release of the traction suture and subsequently double J placement via cystotomy.17
The increase of serum creatinine after ureteral obstruction and ureteral kinking
The increase in serum creatinine concentration after ureteral obstruction has widely been reported in the literature5,8–10,18,19 and is basically consistent with the observations of the present study. However, the first postoperative creatinine determination revealed a much higher mean increase (122%) than in a previous study5 of 7 ureteral obstructions after robotic and vaginal apex suspension procedures (60%). The explanation of the divergent observation is probably based on the different interval to the primary intervention, which was limited to the first 24 postoperative hours, in contrast to this study (8-48 hours).
On the other hand, not all ureteral lesions cause a meaningful increase of creatin on the first postoperative day. Depending on the type and impact of the lesion (peritoneal or vaginal ureteral fistula, hydronephrosis), an alarming rise may sometimes be delayed until postoperative day 2 or even later.10
In postoperative ureteral obstructions, a creatinine increase of 0.2mg/dL in the first 24 hours has repeatedly been reported to be the maximum tolerable limit not fearing an obstruction (8,9). In contrast, in the study mentioned above,5 an ROC analysis of 273 robotic and vaginal apex suspension procedures revealed a strong positive predictive value for the presence of ureteral injury at an increase of creatinine ≥0.3mg/dL exhibiting a sensitivity and specificity of 100 and 96.4%, respectively. The findings of the present study are consistent hereby: the minimum increase in creatinine in the group with obstruction of the ureter was 0.6 mg/d, clearly above the limit (patient no. 2 with unilateral obstruction). On the contrary, the maximum increase in the patient with spontaneously recovered ureteral kinking (no. 8) remained below the limit at 0.1mg/dL indicating a low-grade ureteral impairment as a result of surgery but there was no obstruction. Thus, all cases of this study would have been correctly allocated based on the creatinine increase threshold alone.
However, a creatinine rise of > 0.2mg/dL is not always attributable to an injury of the ureter. This was evident from a study of 5 patients with an early creatinine rise above 0.2mg/dL, but only one case with ureteral obstruction.8 Other factors like intraoperative blood loss, volume of fluid replacement and use of nephrotoxic medication may be involved in serum concentration of creatinine as well. Therefore, the unchallenged clinical benefit of pre- and postoperative serum creatinine measurement is primarily based on its high (100%) negative predictive value.5,8
Normally, a small decrease in serum creatinine occurs at the first postoperative check-up,9,10 as was also shown in this study in 2 patients without ureteral lesion (no. 5 and 6). The reason is probably due to hemodilution resulting from postoperative infusion therapy. On this background, the early postoperative increase in creatinine is a serious biochemical warning sign requiring further diagnostic measures independent of a specific threshold.10
The underlying pathophysiologic mechanisms of increase in serum creatinine after ureteral obstruction
Ureteral injury is the result of direct and indirect damage by ligation and transection of the ureter or tissue distortion resulting in kinking and obstruction of the ureter consecutively impairing ureteral patency.20–22
Several pathophysiologic mechanisms precede the increase in serum creatinine. Obstruction of the ureter leads to a dramatic increase in pressure proximal to the obstruction, which is transmitted to the renal pelvis. The result of the elevated intrarenal pressure is a decrease of GFR with the consequence of cessation of urine production without dilatation or pain, and finishing ureteral peristalsis.23 This is followed by a transient increase in creatinine for 24 hours indicating a transient decline of global renal function. In the case of unilateral ureteral obstruction, the contralateral kidney compensates afterwards for the failure of the compromised ipsilateral kidney.8 The interference between impaired renal function and incipient compensation by the unaffected kidney is reflected in the logarithmic creatinine increase with unilateral obstruction (Figure 3).
The decrease in GFR in the first 24 hours after obstruction is reported in the literature to be 4%.5,8 This clearly contradicts the results of the present study, which showed a mean decrease in GFR of 68% at the first postoperative follow-up. However, it must be considered that the timeline was beyond 24 hours on the one hand and 2 cases showed bilateral obstruction (Table 2) on the other hand. Furthermore, the calculation of GFR involves only an estimate according to the CKD-EPI formula.
The reduced urinary outflow as a leading clinical sign of ureteral obstruction
The glomerular filtration rate (GFR) corresponds to the primary urine. This is the fluid pool forming the definitive urine volume (UV) after tubular reabsorption (TRR): UV=GFR–TRR. The global decrease in primary urine immediately after ureteral obstruction is thus equivalent to a decreased production of definitive urine. Clinically, this situation appears as oliguria or anuria, as shown in 4/5 patients in the present study.
Therefore, simple monitoring of postoperative urine output in the first few hours is a very important tool to be alert to possible ureteral damage.
The rate of TRR is 99% of the GFR, so the definitive urine volume can be estimated with GFR/100. If one accepts a GFR of 100mL/min as a rough order of magnitude in patients without comorbidity, the postoperative urine output after surgery would have to be compared with an expected volume of approximately 60 mL/hour, considering the diuretic effect of postoperative infusion therapy.
If the real urine output is falling below, significantly, without signs of obvious urinary concentration, forcing diuresis by a single intravenous application of 20mg furosemide may be attempted. If the provocation test remains unsuccessfully, the determination of serum creatinine may provide relevant information and initiate further diagnostic steps.
The significance of an early therapeutic intervention in ureteral obstruction
If intervention is indicated following conclusive diagnosis, prompt treatment of the ureteral lesion is desirable because damage to the renal parenchyma begins as early as 24 hours after obstruction. After 1 to 6 weeks, irreversible renal damage is present.6 However, in animal experiments in rats recently has been shown that despite normalization of GFR, tubulointerstitial fibrosis with progressive atrophy and dilatation and renal insufficiency due to protein leakage will start after only a few weeks, even with early removal of ureteral obstruction after 72 hours.24 Therefore, the risk of subsequent chronic kidney disease is always present if the obstruction of a ureter is not corrected immediately.
Regarding the specific treatment for postoperative ureteral obstruction, recent literature predominantly favors methods using a ureteroscopic retrograde or percutaneous nephrostomy antegrade stent.25–27 Although this procedure is often successful in the case of ureteral kinking, overcoming a real obstruction with splinting of the ureter does not always succeed. In these circumstances it will be necessary to switch to an alternative direct renal urinary drain using a nephrostomy catheter, may be for longer time. For higher obstructions after sacrocolpopexy or uterosacral ligament suspension, the sequence above may be useful, potentially added by a secondary surgical procedure later.
Regarding the obstructive lesions after anterior colporrhaphy in this study, the time to intervention spanned 18 to 73 hours and already overlapped with the critical range of subsequently renal parenchymal damage. However, it was found that rapid surgical intervention by revision of anterior colporrhaphy on the day after the primary procedure resulted in significantly faster success than time-consuming retrograde or antegrade stenting methods in the patients concerned here finishing ultimately in urinary drains by nephrostomy for a longer time.
Although there is the undeniable disadvantage of renewed anesthesia in a second procedure, the operative work is low since the obstruction is usually removed by solving two easily accessible rows of sutures.
Limitations of this study
The present study is associated with several limitations. The most serious limitation of the results concerns the very small number of cases. Second, it is a retrospective study with two major disadvantages: first, despite careful manual extraction of the information in the medical record, complete data sets cannot be obtained generating a further disastrous lack in an already small number of cases. Second, there is a large variability of the timing of qualitatively comparable events because postoperative monitoring did not follow a prospective protocol. This implies the realistic risk of statistical bias of the compared measurements and creates a considerable spreading on the time axis. In this respect, the described results give a clinical indication, but must be evaluated with caution and restraint, as the data base is not very reliable.
A strength of the study is the comparison between patients with unilateral and bilateral obstruction of the ureter. Even though the number of cases per category is again smaller, it was still possible to demonstrate the pathophysiological differences due to the compensating effect of the contralateral kidney in unilateral obstruction.
Concerning gynecological and obstetric surgery, a few cases are complicated by unilateral or bilateral obstruction or kinking of the ureter. Since intraoperative cystoscopy with intravenous administration of indigo carmine is not a mandatory standard of every procedure, the question arises, if a method is available checking the integrity of the ureters in the early postoperative period when cystoscopy is not performed.
The present study shows that pre- and postoperative monitoring of serum creatinine is suitable for this purpose even after unilateral obstruction. The negative predictive value with exclusion of a ureteral lesion in the absence of a postoperative creatinine increase is reliable and exceeds the positive predictive value because an increase in creatinine after surgery is not necessarily associated with obstruction.
According to the pathophysiology of acute ureteral obstruction, a decrease in urine output is the first warning sign of an impaired drain of urine. Therefore, contemporary postoperative registration of urine flow is of high diagnostic value. Routine combination with measurement of serum creatinine within the first 24 hours is useful because it may provide reason for further diagnosis if an increase is present.
The primary goal is to remove a unilateral or bilateral ureteral outflow obstruction without delay, as the sensitive parenchyma of the kidney is rapidly compromised resulting in chronic renal damage if the obstruction is not relieved within a maximum of 3 days.
In the interest of this requirement, speedy revision surgery is preferred in obstructions after anterior colporrhaphy because, in contrast to other situations, the ureter can usually be released in these cases faster and more reliably than using retrograde or antegrade stenting methods.
Given the narrow data base of this study, it is desirable for future analyses to standardize postoperative monitoring after gynecologic and obstetric surgery including serum creatinine and to continue collecting cases with ureteral lesion.
None.
None.
There are no conflicts of interest.

©2022 , et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.