eISSN: 2377-4304


Research Article Volume 6 Issue 6
1Department of Gynecology and Obstetrics, So Paulo State University, Brazil
2Department of Obstetrics and Gynecology, Federal University of Minas Gerais, Brazil
3Department of Radiotherapy, Hospital Luxemburgo, Brazil
4Hospital Luxemburgo, Brazil
5Internal Medicine Department, Federal University of Minas Gerais, Brazil
Correspondence: Agnaldo L Silva Filho, Departamento de Ginecologia e Obstetrcia da Faculdade de Medicina da Universidade Federal de Minas Gerais, Avenida Professor Alfredo Balena 190. Santa Efigênia. Belo Horizonte. Minas Gerais. Brasil. CEP: 30130100, Tel 55-31-34099764, Fax 55-31- 34099765
Received: October 28, 2016 | Published: April 24, 2017
Citation: Ferreira APM, Paiva SPC, Lima SSS, et al. The Impact of Mindfulness-based Interventions onthe Wellbeing of Cervical Cancer Patients on Chemoradiotherapy. Obstet Gynecol Int J. 2017;6(6):144-148. DOI: 10.15406/ogij.2017.06.00224
Introduction: Cervical cancer (CC) is the fourth most common cancer in women worldwide, and a major cause of morbidity and mortality. Mind-body skills represent an experiential approach to teach relaxing techniques that can enable patients to achieve mindfulness and self-awareness to engage in self-care. This study has examined whether a shot-term mindfulness-based skills (MBS) program can improve the wellbeing of women with cervical cancer being treated with chemoradiation.
Methods: A cohort of 60 women was enrolled at a public academic cancer center, while on treatment for cervical cancer. The MBS intervention consisted of 7 weekly sessions of mindfulness meditation, relaxation, autogenic training, bio feedback and guided imagery. All participants from control group (n=30) and study group (n=30) were paired for age and prospectively evaluated between January and June 2013. Quality of life was assessed by the European Organization for Research and Treatment of Cancer Quality-of-Life Questionnaire (EORTC QLQ-C30). The distress was evaluated by Distress Thermometer, and salivary cortisol was evaluated by Salivette®. The differences between groups were assessed by Student's t and Chi-square tests. Significance level was set at 5%.
Results: The groups were similar in relation to marital status, education, menopause, height and weight. The analysis revealed significant better quality of life in women with cervical cancer submitted to chemoradiation who practiced the MBS techniques compared to control group (p=0.0001). There was also a significant association between participation in the MBS program and decrease of Distress Thermometer parameters (p<0.0001) and salivary cortisol (p<0.0001).
Conclusion: Both qualitative and quantitative assessment suggests that a 7-week MBS program may decrease salivary cortisol, as well as improve the general wellbeing and quality of life of women with cervical cancer undergoing chemoradiation.
Keywords: cervical cancer, chemoradiation, quality of life, salivary cortisol, stress/distress, mindfulness
LMIC, low and middle income countries; QOL, quality of life; MBS, mindfulness-based skills
Cervical cancer is the fourth most common cancer in women worldwide and a major health concern in low and middle income countries (LMIC). Surgery is the main treatment for patients with initial disease, stages I to IIA, and chemoradiotherapy is the current standard for those patients with locally advanced disease (stages IIB to IIIB).1 In LMIC, most patients present at diagnosis with locally advanced disease and need chemotherapy combined to radiotherapy as their first treatment.
Chemoradiotherapy is associated with acute and long term side effects that significantly impacts quality of life (QOL) in cervical cancer survivors. Moreover, cancer diagnosis and treatment are associated with significant emotional load and physical changes, as well as a broad symptomatology including pain, fatigue, changes in functionality, low acceptance of body image, marital relationship difficulties, stress and distress.2-4
Stress is a popular term worldwide associated with psychiatric disorders. The term distress, more commonly used in the field of Oncology, means extreme anxiety, sorrow or pain and is common in patients receiving cancer diagnosis. The term distress is justified by the National Comprehensive Cancer Network (2007) as a specific way of depicting a well-defined psychosocial aspect of cancer patients.3 Chronic stress can affect the body growth and metabolism, causing malfunction of the thyroid gland and affecting the menstrual cycle and the reproductive function. It can also influence the cognitive and motivational aspects of learning.5
Mindfulness-based techniques are widely known to reduce psychological symptoms of distress and enhance quality of life.6-8 The use of mindfulness-based techniques, such as meditation, relaxation exercises, biofeedback, guided imagery and journal writing, aim at the cultivation of a nonjudgmental awareness of whatever is happening at each successive moment of perception.6 Mindfulness meditation, the core of the Mindfulness-based Skills (MBS) program, exerts beneficial effects on physical and mental health, including symptoms of general distress such as worry, rumination, anxiety, depressive symptoms, sleep quality, pain and quality of life.9-19
Most of the techniques and activities of the MBS have as a main task the promotion of neuro-endocrine response and muscle relaxation. This state of relaxation is effective against the physical and emotional responses to stress, causing the body to return to a state of homeostasis and important balance.20 The anti-stress response has a fundamental effect on the decreased levels of hormones related to stress mechanism, as norepinephrine and cortisol, promoting physiological changes such as decreased heart rate, decreased blood pressure, slowing down breathing, decreased muscle tension, peripheral vasodilatation and elevation of body temperature in the extremities.21 Therefore, the aim of this study was to investigate whether a short-term MBS program would improve the wellbeing of women with cervical cancer on chemoradiation.
Study design and ethical approval
A cohort of 60 women was enrolled at a public academic center of cancer therapy in Belo Horizonte, Brazil, took part in this study and was prospectively evaluated between January and June 2013. The project was reviewed and approved by the Institution’s Research Ethics Committee Board and all the participants signed then informed consent. Participants included women with cervical cancer, confirmed by histopathology, and submitted to chemorratiation and with no difficulty to understand the questions in the questionnaires. Demographic and clinical data of participants were obtained from medical records, interview, and examination. Participants from control group (n=30) and study group (n=30) were paired for age and completed the European Organization for Research and Treatment of Cancer Quality-of-Life Questionnaire (EORTC QLQ-C30) to evaluate the quality of life before and after intervention. Distress was evaluated in salivary cortisol with Salivette®. The study intervention was participation in the MBS program.
Intervention
The MBS program followed the Georgetown University School of Medicine (GUSOM) protocol, as described elsewhere.8 Participants met with the MBS program facilitator individually for 1 hour every week, over 7 consecutive weeks. Each session included relaxation techniques, controlled breathing, autogenic training, biofeedback, guided imagery and participants were encouraged to engage in physical activities as well as journal writing.
Each session began with a brief medication and a “check-in” that provided the opportunity for participants to receive individual attention and instruction, as well as share their feelings about their personal experiences and learning about the MBS techniques. Facilitator also asked questions regarding regular physical activity, eating habits, journal writing, as well as to mention one positive event that occurred in the last 7 days. After check-in, a new MBS technique was demonstrated, practiced and then processed. Every session ended with a brief meditation.
Outcome assessment
Before and immediately after the MBS program, participants were surveyed about the impact of the techniques on self-awareness, self-reflection, stress management and quality of life. Saliva samples were also collected before and immediately after the MBS program, for cortisol levels measurements.
Quality of life was evaluated by the European Organization for Research and Treatment of Cancer Quality-of-Life Questionnaire (EORTC QLQ-C30), a generic instrument which evaluates the quality of life of individuals with cancer. QLQ-C30 is composed of five functional domains (physical, functional development, cognitive, emotional and social), three symptom domains (fatigue, pain, nausea and vomiting), one domain of overall health status, and another on general quality of life, as well as items which evaluate dyspnea, loss of appetite, insomnia, constipation, diarrhea, and disease financial impact. Questionnaire internal consistency was measured by the Cronbach alpha coefficient with a value of 0.70.21
Salivary cortisol was evaluated by Salivette®. Saliva samples were collected in plastic tubes with cotton. This device allows an easy and clean catch. The salivary cortisol shows good correlation with serum total cortisol and free serum cortisol. It has the advantage of being a non-invasive, painless and safe method. Cortisol values between 2.1 to 15.7 nmol/L were considered normal.
Distress Thermometer was used to evaluate the distress. It is a tool created by the National Comprehensive Cancer Network in 2003 in order to assess the degree of anxiety/stress (distress) that the person experiences. It is a self-registration, composed of two instruments, one that examines the level of distress and other identifying possible causes (list of issues). The first is presented as a thermometer and allows for signaling the level of distress, starting from 0 to 10 (0=no distress and 10=extreme distress). Levels higher than 5 indicate a significant level of distress.22 The distress thermometer has been adapted and validated for the use in Brazilian cancer patients. The list of problems consists of 36 items, which identifies possible causes of distress on the past week. Items can be grouped in 5 dimensions: problems of day-to-day, family problems, emotional problems, religious issues and physical problems.23
Statistical analysis
Data was analyzed using Statistical Package for the Social Sciences - SPSS (version 17.0). Data normality distribution was evaluated by the Kolmogorov-Smirnov test. The statistical differences between the groups were tested using Chi-square, Student’s t-test or Mann-Whitney U test as required. Significance level was set at 5%. The sample size of 30 participants per group was derived on the assumption that it is sufficient to resolve, with a statistical power of 80% and a confidence level of 95%, a difference of at least 30% between the proportions for the groups and a difference of at least a standard deviation in the difference between the means of the groups.
Demographic data
Participants’ age in the intervention group ranged from 29 to 79 years (mean ± standard derivation: 55.5 ± 14.8 years) and in the control group ranged from 37 to 79 years (mean ± standard derivation: 56.8 ± 13.1 years). The groups were similar in relation to marital status, education, menopause, height and weight (Table 1).
|
Variables |
Categories |
Groups |
P |
|
|
control |
Cases |
|||
|
Age (years) |
|
56,8 ± 13,1 |
55,5 ± 14,8 |
0.721 |
|
Marital Status |
Single |
3,3% |
6,7% |
0.979 |
|
Married |
33,3% |
33,3% |
||
|
Stable Relationship |
16,7% |
16,7% |
||
|
Widowed |
30% |
30% |
||
|
Separated |
16,7% |
13,3% |
||
|
Schooling |
None |
10% |
6.7% |
0.657 |
|
Primary Incomplete |
36,7% |
56,7% |
||
|
Primary Complete |
13,3% |
10% |
||
|
Secondary Incomplete |
20% |
13,3% |
||
|
Secondary Complete |
32% |
18% |
||
|
Tertiary |
0% |
0% |
||
|
Menopause |
No |
30% |
33,3% |
1.00 |
|
Yes |
70% |
66,7% |
||
|
Height (m) |
|
1,6 ± 0,07 |
1,6 ± 0,06 |
0.955 |
|
Weight (kg) |
|
63 ± 12 |
63,4 ± 10,6 |
0.892 |
Table 1 General Characteristics of the Sample
Note: data expressed as means ± standard deviations and proportions. Comparisons between groups by the Student t and Chi-squared tests.
European Organization for Research and Treatment of Cancer Quality-of-Life Questionnaire (EORTC QLQ-C30)
There was a significant improvement in quality of life in cervical cancer patients submitted to chemoradiation who participated in the MBS program compared to pre-intervention values (p=0.0004). On the other hand, there was a significant quality of life decrease in the control group compared with pre-intervention values (p=0.0002) (Figure 1). The intervention cohort, compared to the control arm, presented a worse baseline QLQ-C30 score (p=0.0273). However, QLQ-C30 score after chemorratiation presented a significant decrease in the control group, and, compared to the intervention group, there was a statistic significant difference in quality of life between patients, favoring the intervention cohort (p<0.0001) (Figure 1).
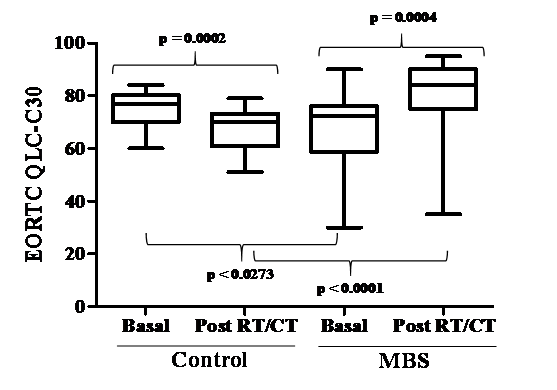
Figure 1 Association between participants to MBS program and quality of life.
Note: data are expressed as median and interquartile ranges. Comparisons between groups were performed using the Mann-Whitney U test.
Distress thermometer
The Distress Thermometer registered decreased levels of distress in women with cervical cancer submitted to chemoradiation that participated in the MBS program compared with preintervention values (p<0.0001), and on the other hand, control group had increased distress after chemoradiation (p=0.0036) (Figure 2). Prior to chemoradiation, the distress scores were higher in the study group compared with the control one (p=0.0034). However, after chemoradiation, the control group had a significant increase in distress scores, compared with intervention group indicating worsening of distress (p<0.0001) (Figure 2).
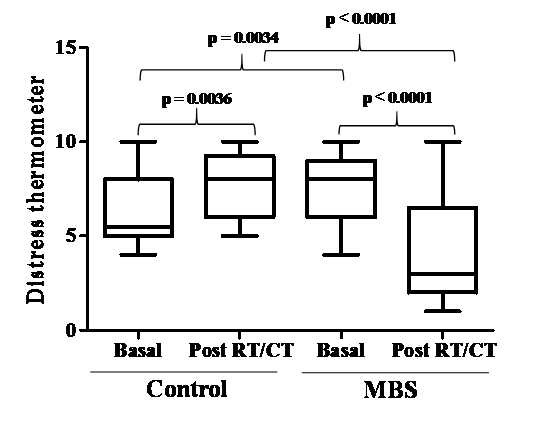
Figure 2 Association between participants to MBS and Distress Thermometer.
Note: data are expressed as median and interquartile ranges. Comparisons between groups were performed using the Mann-Whitney U test.
Salivary cortisol levels
There was a significant decrease in salivary cortisol levels in women with cervical cancer submitted to chemoradiation that participated in the MBS program (p<0.0001) compared with preintervention values. On the other hand, there was a significant increase in salivary cortisol levels after chemoradiation in the control group compared with pretreatment values (p<0.0001) (Figure 3). Both intervention and control groups presented similar salivary cortisol levels before chemoradiation (p=0.0128). However, salivary cortisol levels after chemoradiation decreased in the intervention group, compared with increased levels in control group (p<0.0001) (Figure 3).
Our findings suggest that a 7 weekly sessions of MBS program is effective in improving the general wellbeing and quality of life and decreasing distress and salivary cortisol in cervical cancer patients on chemoradiotherapy. Distress in the context of a cancer diagnosis is an anticipated response. However, the intensity and duration of distress varies according to cancer type, social circumstances of the patient, prognosis and morbidity associated with treatment. Focusing on cervical cancer chemoradiation, it impacts on bladder, bowel and sexual function, as well as overall quality of life. A multi-specialty team and a patient-centered approach is essential to overcome those challenges.
The majority of research regarding meditation as a supportive care in cancer patients report positive results, including improvements in mood and sleep quality, as well as reduction in stress and distress.24 In the present study, researchers investigated whether a short-tem MBS program would improve the wellbeing of women with cervical cancer undergoing chemoradiation. The study objectives included making the stress of cervical cancer and radiotherapy more manageable, enhancing patients awareness and presenting opportunity for self-care.
Cancer patients repeatedly endure physical and emotional events that activate stress-response mechanisms, including the hypothalamic-pituitary-adrenal (HPA) axis. Such repeated activation has been associated with HPA axis deregulations and adverse health consequences.25 One sign of deregulation in this endocrine stress response system is the alteration of the circadian cortisol rhythms.25-27 Deregulations of the cortisol response may compromise tumor resistance. Glucocorticoids have been implicated in tumor growth, both in animal and in in vitro studies.26,27 Cortisol may accelerate tumor growth via immunosuppressive actions or effects on metabolic processes.28,29 When cortisol profiles are affected, dysregulated patterns of immune activity and immune cell trafficking may also emerge.30 Some researchers demonstrated that patients with breast and ovarian cancer with altered cortisol rhythms might present disruptions in patterns of circulating leukocytes, neutrophils, platelets, and serum proteins.31 To our knowledge, there has been no other study investigating the impact of the MBS program on salivary cortisol levels of cervical cancer patients on chemoradiotherapy.
Meditation, one of the most common mind-body interventions, is a conscious mental process that induces a set of integrated physiological changes named the relaxation response. Mindfulness-based meditation, the core of the MBS program, strives to develop an objective observer role, thus creating a non-judgmental mindful state of conscious awareness. Although its mechanisms of action have not been fully characterized, recent neuroimaging studies suggest that hypnotic phenomena are associated with brain activity within brain structures involved in the regulation of consciousness. Guided imagery, another MBS technique, has potential applications in relieving cancer-related pain and symptom-related distress, as well as reduction in pain sensation.32 Guided imagery and relaxation training have been also effective in diminishing anticipatory nausea and vomiting in patients receiving chemotherapy, reducing anxiety and distress caused by invasive medical procedures and decreasing pain caused by aversive medical procedures.33 Music and art therapy, another MBS technique, are used to creative process to allow awareness and expression of an individuals’ deepest emotions. For many years, music therapists have served the needs of hospitalized patients by helping to alleviate isolation, anxiety, fear, and sometimes boredom associated with lengthy hospital stays. Some cancer researchers have identified the importance of music therapy on pain management, nausea control, and psychosocial concerns, such as depression and anxiety.34 Journaling involves writing down ones’ thoughts and feelings for therapeutic purposes. As another MBS technique, it has most frequently been used to assist patients in dealing with stress or trauma. However, journaling can also be used to address specific life problems and symptomology, as with cancer patients.35 Evidence shows that writing about stressful events can improve the wellbeing and reduce the frequency of medical visits. It has also positive implications improving the immune function, as well as psychological and behavioral effects in cancer patients.35
In the present analysis, there was a significant correlation between engaging in the MBS program prior to chemoradiation and improvement on wellbeing and quality of life, as well as reduction in stress, distress and salivary cortisol throughout the treatment. Our results in this specific subpopulation of cervical cancer patients undergoing chemoradiation suggest that the MBS program is a valuable experiential approach to promoting self-awareness, self-reflection and self-care. Increased mindfulness accounts also for changes in mood and perceived stress that explain, in part, the positive impact of the MBS interventions on stress coping. However, these positive results may have been influenced by the small sample size. The difference in quality of life and distress thermometer score at baseline between control and intervention arm may be an imbalance consequent to this small cohort, but it also may reflect a selection bias. Nonetheless, even with a worse baseline score, patients on BMS intervention arm presented better scores at the end of the treatment compared to their own baseline and compared to the control arm score. This “double comparison” strengths the current analysis - BMS and control arm patients were compared at baseline and at the end of treatment for all study parameters between each other, and, each arm was individually compared as well.
As expected, patients in the control group (no MBS intervention) presented deterioration in their quality of life, increased distress, as well as increased levels of salivary cortisol after chemoradiation. On the opposite, MBS intervention patients presented an increase in quality of life and a decrease in distress, suggesting that the intervention is an efficacious tool. The results of this study may have clinical implications as BMS intervention is easy to apply, has low cost and is safe to the patients.
MBS techniques might be effective in improving quality of life and reducing distress in cervical cancer patients. Further investigations are needed to advance the understanding of MBS mechanisms and its effects on stress and distress of patients with cervical cancer undergoing chemoradiation. If supported by rigorous research studies, the practice of mindfulness meditation – the main MBS technique – might be promising to facilitate the cultivation of a healthy mind and increased wellbeing for this subpopulation.
None.
None.

©2017 Ferreira, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.