eISSN: 2377-4304


Case Report Volume 4 Issue 2
1Department of Obstetrics and Gynecology, University of Florida College of Medicine, USA
2Department of Internal Medicine, University of Florida College of Medicine, USA
3Department of Pathology, University of Florida College of Medicine, USA
Correspondence: Erich T Wyckoff, Assistant Professor, Division of Gynecology, Department of Obstetrics and Gynecology, University of Florida College of Medicine, 1600 SW Archer Road, Gainesville FL, 32608, USA, Tel (352)213-5903
Received: December 08, 2015 | Published: February 9, 2016
Citation: Wyckoff ET, Cua GM, Alizadeh L, et al. The bartholin cyst that wasn’t: a case report of metastatic cancer. Obstet Gynecol Int J. 2016;4(2):60-62. DOI: 10.15406/ogij.2016.04.00102
Bartholin gland cysts and abscesses are common disorders of the Bartholin glands, with carcinomas and benign tumors being rare.1 Nevertheless, it may be suggested that patients over 40 years of age with a suspected Bartholin gland cyst or abscess should undergo both drainage and biopsy of the lesion in order to exclude potential carcinoma. While metastatic disease is common in primary cancers of the Bartholin gland secondary to its rich vascular and lymphatic network, we present a case report of a poorly differentiated endometrial carcinoma metastasis to the Bartholin gland that initially presented as a Bartholin gland abscess. This case also serves as a useful reminder that each presentation, no matter how seemingly common or innocuous, deserves critical inspection and must be managed in the context of the patient as a whole.
Keywords: Bartholin, Gland, Cyst, Abscess, Endometrial, Uterine, Cancer, Carcinoma, Malignancy, Metastasis
EMB, Endometrial Biopsy; PET, Positron Emission Tomography; FDG, Fleurodeoxyglucose
Endometrial cancer is the most common gynecologic cancer in economically developed countries, and the second most common gynecologic cancer in economically developing countries.2 Women in the United States have a 2.6% lifetime risk of developing uterine cancer, with the average age of diagnosis being 61 years old.2 Eighty to ninety percent of the time, abnormal vaginal bleeding or discharge is the primary chief complaint.3 At the time of diagnosis, the risk of the patient having distant metastases is approximately 8%.4 Common sites of metastases from uterine cancer are the lungs, liver, inguinal and supraclavicular nodes, bones, brain, and vagina.5 With regards to alternate sites of metastasis, the Bartholin glands are a rare target, with few case reports published of their existence. Primary cancers of the Bartholin gland, however, have been described, with many case reports detailing them and their potential for metastases to the liver, lungs, and even the brain. We present a case of a perimenopausal woman who initially presented with a left vaginal lesion and irregular menses that was later found to have a poorly differentiated carcinoma in both the Bartholin gland and endometrium. Histology and imaging later determined the endometrium to be the primary source of the malignancy.
A 52 year old G1P1001 female with a history of hypertension, hyperlipidema, depression, and schizoaffective disorder presented with the primary complaint of a painful left sided vaginal mass. She also complained of irregular heavy menses for the past three months. On pelvic exam, the vaginal mass was diagnosed as a left Bartholin gland abscess that measured 2x3cm and was noted to be indurated. The remainder of the pelvic exam was unremarkable. The patient was offered incision and drainage for which she declined. She was started on Augmentin. Perimenopause was thought to be a contributing factor of the patient’s irregular menstrual pattern. As part of screening guidelines, Papanicolaou smear was performed and was found to be remarkable for atypical glandular cells of undetermined significance. Endometrial biopsy (EMB) was recommended. The patient was lost to follow up for two months. She eventually returned to clinic and reported improvement in the abscess after antibiotics, but recurrence after discontinuation. During her follow up visit, EMB and incision & drainage of the Bartholin abscess with placement of Word catheter was performed. However, due to the exuberant amount of indurated tissue expressed from the Bartholin abscess, a tissue specimen of the Bartholin abscess were sent to pathology for evaluation. The pathology report returned a poorly differentiated malignant neoplasm favoring carcinoma for the Bartholin gland sample as well as the endometrial biopsy sample. The tumor was described as poorly differentiated and consisting of enlarged nuclei with vesicular chromatin, perinuclear clearing, occasional prominent nucleoli, moderate amounts of amphophilic delicate cytoplasm, and increased mitoses (Figures 1 & 2). There was also extensive tumor necrosis seen in the specimens (Figure 3). The patient underwent CT of her chest, abdomen, and pelvis, as well as a PET CT of the skull to thigh. Her CT revealed a 10.8 cm poorly defined endometrial and myometrial neoplasm, with metastatic disease to the right iliac node, right parametrial nodes, periaortic lymph nodes, and bilateral adrenal glands. There were no other significant findings on CT. Her PET scan showed prominent Fluorodeoxyglucose (FDG) activity in the uterine mass and left adrenal mass, with a smaller amount of FDG activity in a large right pelvic lymph node adjacent to the uterine mass, with no other contributory findings (Figure 4). She was referred to the care of medical oncology, and during the patient’s Gynecology Tumor Board case presentation the pathologists concluded that her poorly differentiated cancer was uterine in origin. Due to the extent of metastatic disease she was recommended medical management. She was started on a Paclitaxel and Carboplatin chemotherapy therapy.
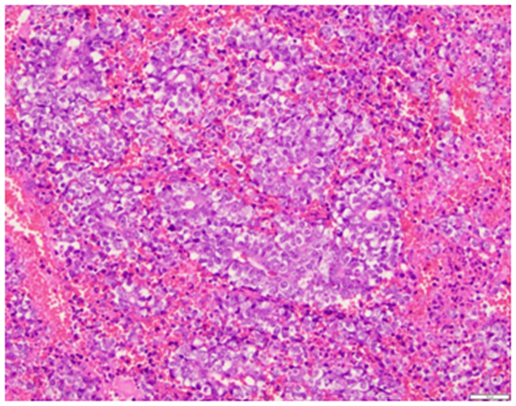
Figure 1 Medium power view of the poorly differentiated tumor, consisting of enlarged nuclei with vesicular chromatin, peri–nuclear clearing and occasional prominent nucleoli (H&E, 20x).
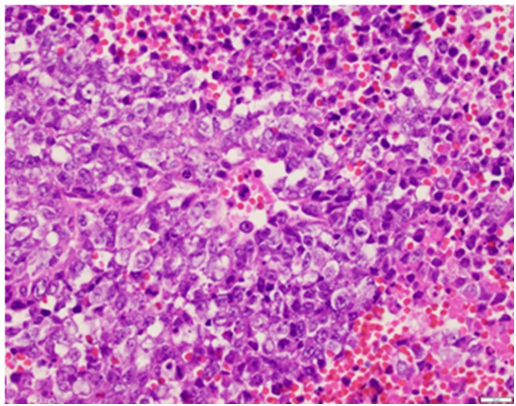
Figure 2 High power view of the poorly differentiated tumor, consisting of enlarged nuclei with vesicular chromatin, peri–nuclear clearing, occasional prominent nucleoli, moderate amounts of amphophilic delicate cytoplasm and increased mitoses (H&E, 40x).
This case is worthy of mention for several reasons. One, because of its deceptively innocuous presentation which later contributed to a major clinical finding, and two, because of the valuable teaching points which arose from these circumstances. Initially, asymptomatic Bartholin gland cysts do not require intervention, particularly if they are small or asymptomatic. However, if they are large or become symptomatic as seen with infection, they are usually incised and drained.1 This provides immediate relief of the pressure. Simultaneous Word catheter placement and/or marsupialization can be performed to help prevent reoccurrence. In our case, the treatment was not so straightforward, as the patient had several factors which made the case more complex. Among them was the clinical context in which this abscess appeared: the patient was an older woman, had an abscess that did not resolve completely with antibiotics, and also had concurrent irregular heavy menses. While her irregular bleeding could have been due to perimenopause, her advanced age raised the suspicion of endometrial cancer. This, along with her abnormal pap smear, prompted us to further investigate with an endometrial biopsy. At the same time, the incision and drainage of her Bartholin gland abscess revealed tissue that was much more exuberant than expected, compelling us to send those samples to pathology as well. Indeed, in women over age 40 who have a Bartholin gland cyst, it is generally recommended that a biopsy be taken to exclude the presence of carcinoma.1 In this manner, the treatment of the Bartholin gland abscess was not as straightforward as simple incision and drainage.
While the majority of Bartholin gland cancers are primary cancers, the results of this case report showed that the carcinoma in the Bartholin gland was actually a metastasis from the endometrium. The majority of cancer cases associated with the Bartholin gland are those of primary cancers, which are mostly adenocarcinomas or squamous cell carcinomas.1 Metastases to the Bartholin gland are rare, with only three cases reported in recent literature: the first from an endometrioid adenocarcinoma that was found to have recurred there,6 the second from a non–Hodgkin lymphoma,7 and the third from a lobular breast carcinoma.8 This finding contributed to the management of the patient because it served as the first indicator of the presence of a metastasis and advanced stage disease.
Bartholin gland cysts and abscesses occasionally warrant further evaluation beyond simple drainage and treatment. In older patients and patients with other concurrent symptoms, biopsies should be performed to exclude potential malignancy. While primary cancers of the Bartholin gland represent approximately 5% of all vulvar cancers, our case demonstrated that uterine metastases to the Bartholin gland is also possible and can present as part of the initial chief complaint. It also emphasizes the importance of further investigating common complaints that behave uncommonly, such as a Bartholin gland cyst that resists antibiotics, recurs after treatment, or appears in the setting of other abnormal gynecological findings.
None.
None.

©2016 Wyckoff, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.