eISSN: 2377-4304


Case Report Volume 12 Issue 2
1Department of Obstetrics and Gynecology, Geisinger Medical Center, USA
2Department of Interventional Radiology, Geisinger Medical Center, USA
Correspondence: Alexis Svokos MD, Geisinger Medical Center, Department of Obstetrics and Gynecology, 100 N Academy Ave, Danville PA, 17821, USA, Tel 570-271-6343
Received: February 18, 2021 | Published: March 3, 2021
Citation: Cunningham KMD, Sullivan MDO, Ahmed SMD, et al. Secondary postpartum hemorrhage due to uterine artery pseudoaneurysm. Obstet Gynecol Int J. 2021;12(2):49-51. DOI: 10.15406/ogij.2021.12.00550
We present the case of a 26-year-old female who experienced secondary postpartum hemorrhage nine days after an uncomplicated elective repeat low transverse cesarean section. She was found to have a uterine pseudoaneurysm and underwent gel foam embolization of the right uterine artery. Subsequently, patient was diagnosed with pulmonary embolism on post-embolization day 3, and was initiated on anti-coagulation regimen.
Keywords: postpartum hemorrhage, uterine artery, maternal death, pulmonary embolus
Postpartum hemorrhage remains the leading cause of maternal death worldwide.1 Primary postpartum hemorrhage occurs within 24 hours of delivery, while secondary postpartum hemorrhage occurs from 24 hours and up to 12 weeks after delivery.2 Most common etiologies of secondary postpartum hemorrhage include sub involution of placental site, retained products of conception, endometritis and inherited coagulopathies. Uterine artery pseudoaneurysm is a rare cause of secondary postpartum hemorrhage with an estimated incidence rate of 2-3/1,000 deliveries.3
We are presenting the case of a 26-year-old female who was admitted with acute onset abdominal pain and secondary postpartum hemorrhage on post-operative day (POD) 9 after an uncomplicated elective repeat low transverse cesarean section (ERLTCS). On CT scan, the patient was found to have uterine pseudoaneurysm with active extravasation. She underwent gel foam embolization of the right uterine artery. Active extravasation was noted at the time of the procedure. The procedure was uncomplicated and post embolization angiogram demonstrated cessation of hemorrhage. Patient was diagnosed with pulmonary embolus on post-embolization day 3, and initiated on anti-coagulation regimen.
The patient is a 26-year-old G2P2002 with a history of anemia who underwent a scheduled ERLTCS at 39 3/7 weeks. Her preoperative hemoglobin and hematocrit were 9.5g/dL and 30.4% respectively. The procedure was uncomplicated and estimated blood loss at the time of cesarean section was 700mL. Post operatively, the patient remained hemodynamically stable and asymptomatic with an appropriate amount of vaginal bleeding. Repeat hemoglobin and hematocrit were obtained on POD #1 and were found to be 8.3g/dL and 26.9%. Patient was discharged home on POD #2 in stable condition. On POD #9, patient experienced acute onset right lower quadrant adnominal pain, which prompted her to present to the emergency department (ED).
On initial presentation, her blood pressure was 107/88mmHg, her heart rate was 121 beats per minute, her respiratory rate was 20 breaths per minute, and her oxygen saturation was 98% on room air. Patient was afebrile with a temperature of 37.0Celsius. On physical exam, patient appeared alert, in no acute distress. Abdomen was soft and diffusely tender, however increased in right lower quadrant. Uterus was enlarged and palpable above the umbilicus, approximately 20-22 week sized. Vaginal bleeding was moderate. Laboratory workup revealed white blood cell count of 19.39K/uL, hemoglobin of 7.0g/dL and hematocrit of 22.5%. CT abdomen and pelvis was obtained and revealed a large region of active hemorrhage within the uterine fundus with a more focal rounded area measuring up to 0.8×1.4×1.4cm, suggestive of a uterine artery pseudoaneurysm (Figure 1) (Figure 2). The patient received one unit of packed red blood cells (pRBCs) while in the ED. Following the initial transfusion, patient’s hemoglobin was found to be 5.8g/dL and an additional 2 units pRBCs were transfused.
Due to patient’s acute blood loss anemia, clinical symptoms and imaging studies suggestive of uterine pseudoaneurysm, patient was transferred to a tertiary care facility with plans to undergo right uterine artery embolization. During the IR embolization, moderate ongoing hemorrhage arising from a branch of the right uterine artery was noted. Successful gel foam embolization of the right uterine artery was completed, and post embolization angiogram demonstrated cessation of hemorrhage (Figure 3) (Figure 4). There were no complications noted during the procedure and patient remained in stable condition. Post procedure, patient had minimal vaginal bleeding, and remained hemodynamically stable and asymptomatic. Her repeat hemoglobin and hematocrit were 8.0g/dL and 25.0%. On post-embolization day 1, patient’s clinical course was unremarkable, and her repeat hemoglobin was 7.6g/dL. Patient was discharged home on post-embolization day 2, at that time she has hemodynamically stable, and was not experiencing significant vaginal bleeding.
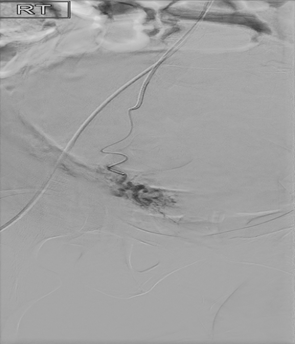
Figure 3 Super selective frontal DSA showing hemorrhage and pseudoaneurym from right uterine artery.
The patient represented the day after discharge with complaints of pleuritic chest pain and shortness of breath. She was tachycardic with a heart rate of 110 beats per minute and had oxygen saturation of 98% on room air. Her hemoglobin was 8.1g/dL and hematocrit 25.3%. Her D-Dimer was elevated at 1.67ug/ml. CT pulmonary embolus scan of the patient was performed and noted to have a sub segmental pulmonary embolus. At that time, she was initiated on heparin protocol and closely observed for worsening of vaginal bleeding. Serial monitoring of hemoglobin and hematocrit was performed, and labs remained stable. Patient was discharged home the next day on oral Apixaban anticoagulation regimen. Her repeat hemoglobin and hematocrit four weeks later were 11.8/36.9g/dL. Patient continued close follow up with anticoagulation clinic as outpatient and remained on Apixaban for 3 months.
Post-partum hemorrhage is an obstetrical emergency and remains one of the leading causes of maternal morbidity and mortality. Primary postpartum hemorrhage occurs within 24 hours of delivery, while secondary postpartum hemorrhage occurs from 24 hours and up to 12 weeks after delivery.2 Most common etiologies of secondary postpartum hemorrhage include endometritis, retained products of conception, subinvolution of placenta and coagulopathies. More infrequent causes involve uterine artery pseudoaneurysm, arteriovenous malformations, malignancies such as choriocarcinoma.
Uterine artery pseudoaneurysm is a rare cause of secondary post-partum hemorrhage with an estimated prevalence rate of 2-3/1,000 deliveries.3 Pseudoaneurysms develop when there is damage to the arterial wall, which leads to a blood-filled cavity communicating with the arterial lumen.4 Unlike a true aneurysm, which involves all three layers of the arterial wall, a pseudoaneurysm is an enlargement of any layer of blood vessel wall. Differential diagnosis of a pseudoaneurysm includes arteriovenous fistulas, arteriovenous malformations and vessel rupture. Risk factors for development of pseudoaneurysms include trauma, surgery, infection or neoplasm that lead to vascular injury. There have been documented cases after cesarean section, myomectomy and hysterectomy.4
Uterine artery embolization (UAE) is a minimally invasive procedure, performed under sedation via access through the right femoral artery. Most commonly, particulate material is used as the embolic agent and there are several that are approved by the Food and Drug Administration (FDA) in the US. Those agents include tris-acryl gelatin microspheres and nonspherical polyvinyl alcohol (PVA) particles.5 UAE is an overall safe and well tolerated procedure that can help manage postpartum hemorrhage. Overall complication rates are low and include amenorrhea (0-3% in women under the age of 45), septicemia (1-3%), pulmonary embolus (<1%).6
Development of pulmonary embolus after UAE is rare and the pathogenesis is poorly understood. According to Virchow’s theory, endothelial injury, hypercoagulable state and venous stasis are well known risk factors for development of venous thrombosis. Risk factors for development of thrombosis include immobility, inherited or acquired thrombophilia, history of prior thrombotic event, surgery, estrogen therapy, malignancies and pregnancy/post-partum period. The risk of developing pulmonary embolus remains increased up to two weeks after delivery.7
Several different theories have been proposed regarding the etiology of UAE related pulmonary emboli. First, stasis of contrast has been visualized in uterine veins following embolization procedure, suggestive of decreased blood flow through pelvic veins, creating potential for thrombosis.8 Second, passage of embolization material such as gel foam directly into venous system can lead to pulmonary embolism.9 Thirdly, during embolization procedure there can be inadvertent injury of endothelial cells, thus promoting local thrombosis and promoting coagulation.10 Lastly, currently there is no standard regarding initiating anticoagulation after UAE. The use of heparin like agents as post procedure thromboprophylaxis is controversial due to the increased risk of associated bleeding complications.11
In the particular case presented, the uterine artery pseudoaneurysm was the cause of the delayed post-partum hemorrhage, as during the patient work-up and evaluation other etiologies of delayed post-partum hemorrhage had been excluded (sub involution of placental site, retained products of conception, endometritis and inherited coagulopathies), therefore the treatment of her acute uterine bleeding with uterine artery embolization was appropriate.
The patient had multiple risk factors which could have contributed to her developing a subsequent pulmonary embolus including recent pregnancy, and recent surgery. Given these predisposing risk factors for development of a thrombotic event, it is difficult to delineate whether the pre-existing risk factors, the uterine embolization or both where the cause of the pulmonary embolus.
Uterine artery pseudoaneurysm is a rare cause of secondary post-partum hemorrhage. In hemodynamically stable patients, uterine artery embolization is a safe option for management of acute bleeding. Acute pulmonary embolus is a very rare, but life-threatening medical complication associated with UAE. Early diagnosis and treatment improve patient outcomes.
In this case it is unclear whether the development of the acute pulmonary embolus was a complication related to the UAE as the patient had multiple risk factors including recent surgery, pregnancy and post-partum period.
None.
None.
The author declares that there is no conflict of interest regarding this study.

©2021 Cunningham, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.