eISSN: 2377-4304


Research Article Volume 6 Issue 1
1University Hospital, France
2Auxerre Hospital, France
Correspondence: Julie Sellier, CHU Service de Gyn?cologie Obst?trique, 14 Rue Paul Gaffarel, 21000 Dijon France, Tel 33 380293702
Received: November 30, 2016 | Published: January 17, 2017
Citation: Sellier J, Lafont M, Choux C, et al. Screening for macrosomia at term: performances of ultrasonographic estimation of the fetal weight and the use of the uterine height. Obstet Gynecol Int J. 2017;6(1):16-21. DOI: 10.15406/ogij.2017.06.00194
Objective: The aim of our study was to assess the performance for the detection of macrosomia at term of estimating fetal weight corrected by the growth effect (EFWc) measured by ultrasound, EFWC via measuring uterine height (UH), the waist circumference and higher uterine height threshold or equal to 37.
Methods: It is a retrospective study of 233 patients whose newborn macrosomes were sampled. The estimated fetal weight (EFW) ultrasound was performed during the 41th week of amenorrhea, as the EFW by measuring waist circumference with the Warsof’s formula and EFW by measuring the uterine height according to the kayem’s formula. These 3 estimates were corrected taking into account the growth effect.
Results: The proportion of estimates with a margin of error of less than 10% was 61.3%, 50% and 68.4% respectively for the EFWc EFWUHc and EFWACc. ROC curves of the EFWc EFWUHc and EFWACc find the Aires under the curve (AUC) to 0.859, 0.783 and 0.856. The EFWc and EFWACc are significantly higher than for term screening for macrosomia compared to EFWUHc (p <0.001 and p <0.001 respectively).
Conclusion: Measuring the EFWc and EFWACc are reliable and simple means for screening for macrosomia term, but will be improved.
Keywords: macrosomia, screening, term, evaluation, accuracy
One of the main tools in the management of pregnancies to term is the estimated fetal weight. This allows the detection of small fetuses for gestational age (SGA), and macrosomic children, defined by a birth weight of over 4000 grams. Indeed, this screening has important clinical implications. Furthermore, the obstetric and neonatal prognosis of macrosomic fetus is marked with a higher morbidity and mortality,1 particularly because of the risk of shoulder dystocia. Concerning these risks, the French College of Obstetricians Gynecologists recommends an elective caesarean section for an estimated fetal weight greater than 4500 grams in case of gestational diabetes or scarred uterus, and 5000 grams in other cases. Thus the estimation of fetal weight (EFW) by ultrasound must be effective because the prenatal diagnosis of macrosomia by estimation on the EFW can lead to an unjustified elective caesarean section a posteriori.2 The underestimation of a macrosomic may pose an obstetrical risk of severe perineal lesions, obstructed labor or dystocia.1
Screening for macrosomia is difficult.3 For this purpose, several methods have been studied such as fetal weight estimation with various formulas, measurement of waist circumference on ultrasound measurement of uterine height with the formula of Johnson, clinical and sonographic estimations whose performances are contradictory in studies.4–6 Several recent studies have demonstrated the performance of an ultrasound to estimate fetal weight in the delivery room7 at term.8–10
Lafont et al.9 showed in his study that the estimated fetal weight using the formula Hadlock with 3 parameters,11 performed by licensed practitioners and taking into account the growth effect, was a reliable and efficient way to estimate the term fetal weight.9
To our knowledge, just few studies have evaluated the performance of screening for macrosomia at term, although the importance of time between the estimated fetal weight and birth which has already been demonstrated.12
The aim of our study was to evaluate the performance of different techniques for screening the macrosomia at term: the estimated fetal weight corrected by the growth effect (EFWc) measured on ultrasound by experienced practitioners, the EFW via measurement of uterine height, the EFW using the measure of waist circumference and threshold uterine height (UH) greater than or equal to 37.
For our study we used the cohort of Lafont et al.9 study of 233 patients, i.e. a retrospective study to estimate fetal weight singleton pregnancies, conducted during the consultation of 41 weeks for patients who gave birth in 2014 to an IIB level maternity at Auxerre Hospital.
Each patient had received an ultrasound during their first quarter between 11 and 13 WG+6 days, enabling precise dating of the date of early pregnancy and the date of the term provided for 41 weeks. During the term consultation carried out systematically for all patients around 41SA, in order to verify the fetal well being, was elevated the uterine height, weight, height, body mass index (BMI) in early pregnancy, weight, height and BMI at 41 weeks, weight gain during pregnancy, the existence of gestational diabetes, the term of the consultation’s day.
The non obstetric ultrasound was performed by practitioners who are all holders of the Interuniversity ultrasound diploma. This ultrasound measures the biparietal diameter (BIP), head circumference (HC), abdominal circumference (AC), femur length (FL) and the amniotic fluid index (AFI) by measuring the four quadrants. The EFW was calculated using the formula Hadlock 3-parameters (BIP, AC and LF)11:
EPF log10 = 1.335 + 0.0316 0.0457 BIP + AC + 0. 1623 LF − LF 0.0034 PA
The Ultrasound scans were performed using a Toshiba type scanner with a 3.5 MHz abdominal probe and meets the quality criteria of the CTE (Technical Committee of the ultrasound) and CFEF (French College of Fetal ultrasound).13 The delivery term and birth weight (BW) were identified secondarily. Multiple pregnancies, morphological or chromosomal abnormalities and patients who had not received an ultrasound Q1 for accurate dating of pregnancy were excluded. In this cohort, we selected for our study as reference sample the macrosomic fetus with a birth weight superior than 4000 grams. The “term-consultations” were conducted between 40 WG + 6 days and 41 weeks + 2 days while the term of delivery was between 41 and 42 WG+1 day.
The EFW has been corrected by considering an average growth of 25g/day between the day of the term of consultation and the day of birth.14 Thus was obtained the corrected estimate fetal weight (EFWc) by the formula:
EFWc= EFW + 25 x N
Where
EFW is the fetal weight estimation on the day of the term of consultation and
N is the number of days between the term consultation and the delivery.
To calculate the fetal weight estimation corrected by measuring the AC (EFWACc) we used the AC measurement performed during the term of consultation which we deducted a fetal weight estimation with Warsof formula15
EFWACc= EPF log10 = 0.092 −1.8367 + AC − 0.000019 AC3
This was corrected using to the same principles as seen above, or:
EFWACc= EFWAC + 25 x N
To calculate the fetal weight estimation via uterine height, we used the formula of Kayem et al.16
EFWUH = ±199.93 [108.59 x UH (cm)]
Which was corrected as seen above:
EFWUHc = EFWUH +25 x N
Finally we used the UH "raw", easily used in routine practice, holding a 37cm line16 as a screening macrosomia. The measurement of uterine height is with a ribbon and to measure the height of the uterus to the pubic symphysis to the uterine fundus. Data was collected and analyzed using the Excel spreadsheet (Office, Microsoft Corporation, Redmond, WA, USA).
After delivery the various EFW were compared to birth weight by calculating the average margin of error, and the proportion estimates with a margin of error of less than 10%. The association between EFW and corrected birth weight was investigated by calculating the Pearson correlation index. For each means of screening the study macrosomia, we calculated the sensitivity and specificity with a 95% confidence interval, percentage, proportion of false positives and false negatives, in percentage, and the likelihood positive and negative ratio, and that, with the XLSTAT 2016 statistical software, Addinsoft, PARIS, FRANCE. We have also, via this software, calculated the ROC curves for the screening of fetuses of more than 4000 g of 3 EFW equations: EFWc, EFWACc, EFWUHc, and compared the areas under the curves by a Student test. Results were considered significant when p <0.05.
The cohort of Lafont et al.9 has 233 patients, and the author has already described the characteristics in his study.9 We have extracted 42 patients who gave birth to a macrosomic child. The mean age was 30.8 years, the average gravidity and parity of 2.5 and 1.1 respectively, the average BMI of 25.99 kg/m² preterm and 32.33kg/m² futures. 9.52% of the patients had gestational diabetes and the average term of the term of consultation was 41SA, regarding the medium term birth, it was 41 SA+3 days. The EFWc found an estimated average weight of 4256.83 grams, the EFWUHc, to 3623.68 grams and EFWACc of 4136.17 grams. The criterion HU greater than or equal to 37 cm was found in 9.52% of the cases. The mean birth weight was 4230.6 grams.
The characteristics of the study population are found in Table 1. The absolute difference between the average weight EFWc and birth weight was 355.7 ± 218.1 grams, with an average margin of error of 9.1% and a Pearson correlation index of 0.53 (Figure 1). The difference in mean absolute weight between EFWUHc and birth weight was 461.0 ± 350.0 grams, with an average margin of error of 9.9% and a Pearson correlation index 1 (Figure 2). For EFWACc, the difference in mean absolute weight with the birth weight of 281.7 grams, with an average margin of error of 7.5% and a Pearson correlation index to 0.45 (Figure 3). The proportion estimates with a margin of error of less than 10% was 61.3%, 50% and 68.4% respectively for the EFWc EFWUHc and EFWACc.
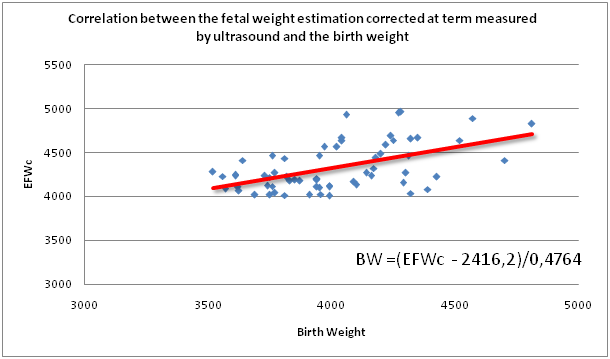
Figure 1 Correlation between the fetal weight estimation corrected at term measured by ultrasound and the birth weight for the detection of macrosomia.
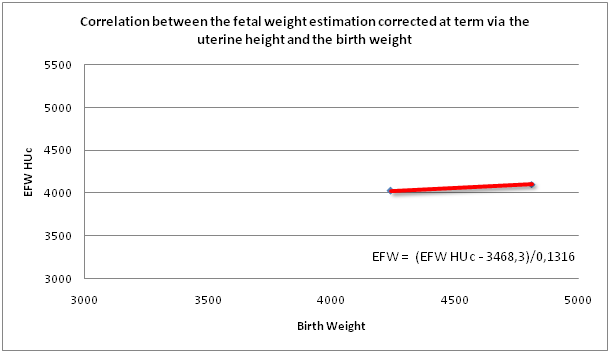
Figure 2 Correlation between the fetal weight estimation corrected at term via the uterine height and the birth weight for the detection of macrosomia.
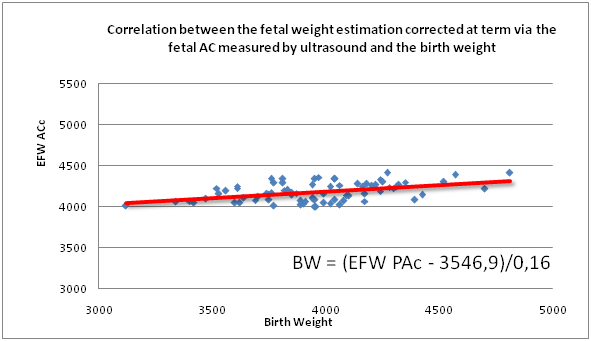
Figure 3 Correlation between the fetal weight estimation corrected at term via the fetal AC measured by ultrasound and the birth weight for the detection of macrosomia.
|
Lafont |
Our study |
Age |
33,7±4,5 [16; 43] |
30,76±5,23 [20; 43] |
Gravidity |
2,27±1,4 [1; 8] |
2,47±1,6 [1; 8] |
Parity |
0,9±1,1 [0; 6] |
1,12±1,31 [0; 6] |
Weight (kg) |
68,6±15 [44; 130] |
71,76±14,19 [48; 110] |
Size (cm) |
164,4±6,1 [145; 182] |
165,90±7,07 [151; 182] |
BMI (kg/m2) |
25,3±5,3 [17,1; 46,1] |
25,99±4,37 [18,29; 35,29] |
Term Weight (kg) |
83,3±14,8 [54; 140] |
89,14±14,41 [64; 119] |
Term BMI (kg/m2) |
30,8±5,1 [20,6; 49,7] |
32,33±4,46 [24,1; 42,6] |
Weight gain |
14,7±6,5 [-21; +33] |
17,38±6,78 [4; 33] |
Diabetes |
26 (11,2%) |
4 (9,52%) |
Term at Consultation |
41 SA |
41 SA |
Term at Birth |
41 SA + 3 days |
41 SA + 3 days |
UH |
3600,2±436,4 [2495; 4810] |
34,42±1,79 [32; 38] |
EFW Corrected (g) |
3743,7±454,9 [2619; 4965] |
4256,83±438,71 [3180; 4965] |
EFW HU Corrected (g) |
3623,68±203,57 [3299,95; 4101,49] |
|
EFWAC Corrected (g) |
4136,17±221,71 [3396; 4415] |
|
UH ≥ 37 |
4 (9,52%) |
|
Birth Weight (g) |
|
4230,60±184,61 [4010; 4810] |
Table 1 Characteristics of the population of the true macrosomes and results of the corrected EFW, EFW corrected by measurement of the uterine height, EFW corrected by the measurement of the AC and uterine height greater than or equal to 37
The values are presented with the mean, the standard deviation and the intervals in brackets. Percentages are in parentheses.
These results are presented in Table 2. In regards to the diagnostic performance of these screening methods which are shown in Table 3, the EPFc a sensitivity and a specificity of 66.7% and 82% respectively, EFWUHc 4.8% and 100% but a false negative rate of 95.2%. The EFWACc has a sensitivity of 81% and a specificity of 77%. HU ≥ 37 had a sensitivity of 14.3% and a specificity of 98.4%. Finally we did the ROC curves of EFWc (Figure 4), the EFWUHc (Figure 5) and EFWACc (Figure 6) found the Areas under the curve (AUC) to 0.859, 0.783 and 0.856. Thus, these three equations are better than hazard, and are considered discriminatory. The EFWc and EFWACc are significantly higher than for term screening for macrosomia compared to EFWUHc (p<0.001 and p<0.001 respectively). We note that the area under the ROC curve of the EFWc for screening for macrosomia is slightly higher than the EFWACc but the result was not significant (p = 0.21).
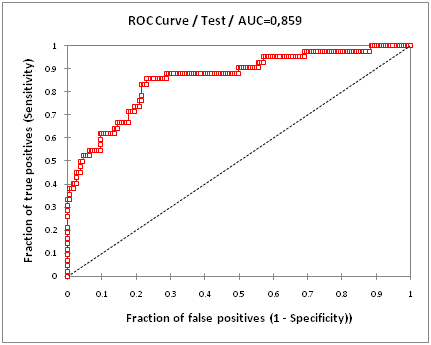
Figure 4 ROC curve from fetal weight estimation to ultrasound corrected at term for macrosomia screening.
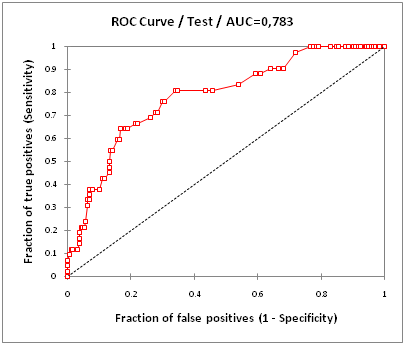
Figure 5 ROC curve of the fetal weight estimation at ultrasound corrected at term via the Uterine Height for the detection of macrosomia.
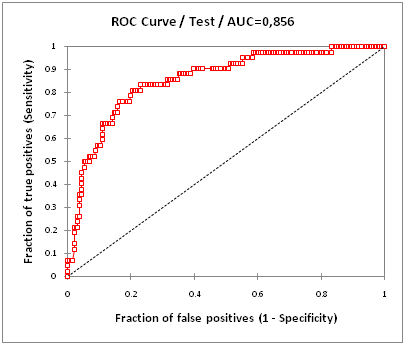
Figure 6 ROC curve from fetal weight estimation to ultrasound corrected through the abdominal perimeter for the detection of macrosomia.
|
Correlation with BW Pearson index |
Average error margin in% |
Proportion of estimations with a margin of error of less than 10%, in% |
EFW c |
0,53 |
9,1% |
61,3% |
EFWUH c |
1 |
9,9% |
50,0% |
EFW AC c |
0,45 |
7,49% |
68,40% |
Table 2 Correlation and margins of error of corrected EFW, corrected EFW by measurement of uterine height, EFW corrected by measurement of AC for prediction of birth weight
|
Sensibility % (CI 95 %) |
Specificity % (CI 95 %) |
PPV % |
NPV % |
FP % |
FN % |
LR + |
LR - |
EFW c |
66,7 (51,5; 79) |
82 (76; 86,9) |
45,2 |
91,8 |
17,90 |
33,3 |
3,8 |
0,4 |
EFW HU c |
4,8 (0,6; 16,8) |
100 (97,5; 100) |
100 |
82,6 |
0 |
95,2 |
_ |
0,95 |
EFW AC c |
81 (66,3; 90,2) |
77 (70,9; 82,7) |
44,2 |
94,8 |
22,6 |
19,0 |
3,6 |
0,25 |
UH ≥ 37 |
14,3 (6,4; 28,3) |
98,4 (95,2; 99,7) |
66,7 |
35,9 |
1,6 |
85,7 |
9,1 |
0,87 |
Table 3 Screening performances of corrected EFW, corrected EFW by measurement of uterine height, EFW corrected by measurement of AC and Uterine Height greater than or equal to 37 for the detection of macrosomia
With IC: 95% Confidence Interval, PPV, positive predictive value; NPV, negative predictive value; FP, false positives; FN, false negatives, LR+, likelihood ratio positive; LR-, likelihood ratio negative
The aim of our study was to evaluate the forward's performance ultrasound to screen for macrosomia. Indeed, many articles show that screening for macrosomia, and more at term, is a difficult and less accurate diagnosis.8,9,15 Indeed, in a review of the literature in 2014, Filkaszova et al.5 showed that the sensitivity for detection of ultrasound averaged 64% for EFW and 83% for the EFWAC.5 For Dimassi7 who conducted a study on a cohort of 299 patients to evaluate the performance of the EFW conducted by specialty in internal work room, the day of delivery, after 37 weeks, found sensitivity of 38% for EFW.7 Noumi15 in a 2004 study, comparing the performance of estimating the clinical and sonographic fetal weight carried by specialty’s resident during labor in a cohort of 199 patients. He shows, for screening for macrosomia, a sensitivity of EFW 50% with a specificity of 97%, and equivalent results for clinical testing.15 Both studies, which have the merit of achieving a EFW during labor, which can be a source of inaccuracy (low fetal head, uterine contractions) and may explain the worse outcomes for screening macrosomia, than those found in these studies. Finally Kayem et al.16 conducted a study in 2009 on a broad population of PREMODA cohort study, from which they selected in 1689 singleton pregnancies patients including 124 children born macrosomic, to compare the performance of the estimated fetal weight extrapolated via the uterine height (EFWUHc) compared to estimated fetal weight estimation via ultrasonographic measurement of AC (EFWAC). In their study, they found a sensitivity of 37.1% for the detection of macrosomia by EFWUH, and 54% for EFWAC, and a specificity of 95.0 and 95.2% respectively. The degree of correlation with birth weight according to Pearson index was 0.61 for EFWUH and was 0.76 for EFWAC,16 but in this study, different measures were not carried forward. To our knowledge, no study has evaluated the performance of screening for macrosomia at term, comparing the performance of ultrasound estimation by experienced practitioners versus the clinic taking into account the effect growth in term patient population. Most studies, including those mentioned above, did not take into account the effect growth between the estimated weight and birth, especially since they were not, for the most part, and carried forward and therefore with an important estimate-childbirth period. One of the great strengths of our study is taking a term population and having taken into account of the effect growth of 25 grams per day.14
This probably contributed to our sensitivity and specificity figures that are above the data we found in other studies. Remember, we find a sensitivity of 66.7 and specificity of 82% for EFWc and EFWACc for a sensitivity of 81% and a specificity of 77%. Our other results for EFWUHc and gross UH are not satisfactory. Nevertheless, one of the main weaknesses of our study is the sample size. Indeed based on 233 patients, only 42 were really carrying a macrosomic child. This is likely one of the reasons why we could not decide significantly the performance of the EFWc and EFWACc. Their ROC curves showed areas under the curve quite satisfactory but comparable (for memory 0.859 and 0.856 for EFWc and EFWACc). We believe that with a more effective population, we could separate the performance of the EFWc and EFWACc significantly for screening for macrosomia term in our study. Our average percentage error, although lower than 10%, was higher than those found in the articles, even though our population specifically studying the futures macrosomic, for which we have little data.
Another moot point in our study may be the choice of our formulas for fetal weight estimation. Many studies used a clinical evaluation method, the Johnson method, for calculating the EFW.4,17 Kayem et al.16 according to this method it calculates a new equation to estimate fetal weight through a large sample of pregnant women (about 19,400 patients) as part of the large cohort PREMODA, conducted in France and Belgium.16 We have therefore chosen to use this new formula, because the characteristics of the PREMODA population are closer to those in our study than those that served for Johnson to develop its equation.
Similarly we chose the formula of fetal weight estimation via the PA formula developed by Warsof,18 which demonstrated its superiority especially vis-à-vis to that of Cambell.19 On the other hand, we used formulas to calculate the weight like Hadlock's formula11 or Warsof18 which are formulas created from eutrophic fetus. Indeed, as Porter et al.20 we wonder if we should not use specific formulas for screening for macrosomia.20 In this spirit Hart et al.21 created a new formula that seems to improve detection of macrosomic fetus.21
A research path being developed to improve the detection of macrosomia is 3D ultrasound. Indicator measurement of the thickness of subcutaneous tissue22 by measuring the diameter "cheek to cheek"23 appears to improve detection of more than 4,000 grams fetus.
In conclusion, our study demonstrated that the measurement of the EFWc and EFWACc were reliable ways, although perfectible, to screen for macrosomia at term. These are simple ways that can easily be used routinely.
Nevertheless it would be interesting to perform the same study on a larger sample in order to discriminate significantly EFWc and EFWACc for screening for macrosomia term. In our study area under the ROC curve of the EFWc is 0.859, and the EFWACc has an area under the ROC curve of 0.856 for screening for macrosomia term, which according to our study, is far from just a trend. Finally it would be interesting to see in the future the contribution of 3D ultrasound in screening for macrosomia.
None.
Julie Sellier is the principal author of this work and wrote this manuscript.
Marine Lafont MD supervised this work as director.
Cécile Choux, MD, reviewed this manuscript.
Cyrille Bernard MD, helped to this work.
Patrick Dellinger MD, is the chief of the Auxerre Hospital maternity, France.
Paul Sagot MD PhD, is the chief of the gynecology and obstetrics department in the University Hospital of Dijon, France.
The authors declare there is no conflict of interests.
None.

©2017 Sellier, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.