eISSN: 2377-4304


Research Article Volume 15 Issue 1
1Tocogynecology resident, Sanatorio Güemes, Argentina
2Gynecology department, Sanatorio Güemes, Argentina
3Chief of Gynecology department, Sanatorio Güemes, Argentina
Correspondence: Garcia Balcarce Tomas, Department of Gynecology and Obstetrics of Sanatorio Güemes, Buenos Aires Argentina, Tel +5491169469707
Received: January 22, 2024 | Published: February 26, 2024
Citation: Caviglione M, Pettachi M, García BT, et al. Residual cervical H-SIL after cervical conization with positive margins. Is there any associated risk factor? Obstet Gynecol Int J. 2024;15(1):33-37. DOI: 10.15406/ogij.2024.15.00731
Introduction: Cervical cancer is the second leading cause of death from gynecological cancer. In Argentina, it is estimated that nearly 4,500 new cases are diagnosed each year and 1,800 women die from this disease. The human papillomavirus (HPV) is a necessary but not a major cause to develop this type of cancer and it is responsible for producing both low-grade (L-SIL) and high-grade (H-SIL) squamous intraepithelial lesions (SIL) depending on the viral serotype in addition to other factors specific to the infected patient. Cervical intraepithelial neoplasia (CIN) is treated by local ablation or excision techniques with lower morbidity. The choice of treatment depends on the degree and extent of the disease, as well as the patient age, risk factors and immunity to generate spontaneous regression or persistence/recurrence.
Objective: To identify clinical or pathological factors in patients who presented residual lesion (H-SIL) in the surgical specimens of both re-conization and hysterectomy (HT).
Materials and methods: A retrospective, observational study was carried out at Sanatorio Güemes, Buenos Aires, Argentina. All patients that underwent cervical conization with an electric scalpel and had positive margins in the surgical specimen between January 2017 and May 2022 inclusive were analyzed. Data was obtained from 43 patients who had positive cervical conization specimen margins at our institution in the time period described above. Two patients who only had the exocervical margin involved and also 11 patients who did not meet the inclusion criteria were excluded. Among patients (30), all were reoperated (16 underwent re-conization, while in 14 patients it was decided to have a total hysterectomy). Among all the patients who underwent a new surgical procedure, residual disease was found in 10 patients (33.3%), while 20 patients (66.6%) had no residual lesion.
Results: The highest percentage of patients (66.6%) did not present residual lesions in the posterior resection specimens. The parameter exhibiting the most substantial influence in our analysis was the proportion of lesion extension, exerting a significant effect on the persistence/recurrence of the disease in subsequent surgical samples (Relative Risk [RR] 7.87, 95% Confidence Interval [CI] 1.13-54.66, p < 0.01).
Conclusion: This information brings us even closer to the new reports of bibliographical data: although the presence of the compromised endocervical margin is valuable for estimating the risk of disease persistence/recurrence, it is not sufficient. Therefore, there is a lack of information about the importance of other factors to predict this situation.
Keywords: human papillomavirus, high grade squamous intraepithelial lesions, cervical intraepithelial neoplasia, conization, endocervical margin, persistence/recurrence disease
HPV, human papillomavirus; SIL, squamous intraepithelial lesions; CIN, cervical intraepithelial neoplasia; HT, hysterectomy; RR, relative risk; CI, confidence interval
Cervical cancer continues to be one of the most common tumors among women. It ranks fourth after breast, colorectal and lung cancer; it is also considered the fourth cause of death from cancer in women and the second cause of death from gynecological cancer. According to data from 2020, there would be an estimated 604,000 new cases and 342,000 deaths worldwide.1 It mainly affects women with low socio-economic resources who, for various reasons (geographical, cultural and/or economic barriers), cannot access screening services. In Argentine, it is estimated that around 4,500 new cases are diagnosed each year and 1,800 women die from this disease.2
Human papillomavirus (HPV) is a necessary but not a major cause of cervical cancer3 with 12 oncogenic types classified as group 1 carcinogens by the International Agency for Research on Cancer Monographs.4 Other important cofactors include some sexually transmitted infections (HIV and Chlamydia trachomatis), smoking, increased birth rates, and long-term use of oral contraceptives.5
Cervical cancer is considered almost completely preventable due to highly effective primary and secondary prevention measures. Since 2011, the Argentine Ministry of Health has been carrying out a comprehensive strategy for the prevention of cervical cancer, which includes primary prevention through the HPV vaccine, and secondary prevention, based on the screening of women (with PAP test or HPV test).2
Cervical intraepithelial neoplasia (CIN) is treated by local ablation or excision techniques with lower morbidity. The choice of treatment depends on the degree and extent of the disease.
Excisional treatment is mandatory for a patient with an unsatisfactory colposcopy, suspected invasion, or glandular abnormality.6 The objective of treatment is to prevent possible progression to cancer in addition to obtaining sufficient histological information to rule out invasion as well as ensuring negative margins of the specimen.7
It has been observed that women older than 35 years with high grade squamous intraepithelial lesions (H-SIL) in the conization sample and involvement of the endocervical glands are more likely to have positive cone margins, which are associated with persistent/recurrent disease.8,9 Therefore, the number of quadrants involved should be evaluated to plan further management.9
Likewise, the management of women who have an excision with marginal endocervical involvement (control vs surgical reintervention) is controversial and is the subject of debate.
It is important to bear in consideration that it is relevant to identify risk factors in patients with H-SIL or greater injury in the surgical specimen from re-excisional treatment (cervical re-conization) or hysterectomy (HT). In the present study, clinical and pathological variables were analyzed to determine their impact on the finding of lesion persistence.
Objective
To identify clinical or pathological factors in patients who presented residual lesion (H-SIL) in both re-conization and HT surgical specimens that were performed due to compromised endocervical margin in the initial surgical specimen.
A retrospective, observational study was carried out at Sanatorio Güemes (Buenos Aires, Argentine). All patients undergoing cervical conization with an electroscalpel who had positive margins in the surgical specimen from the Sanatorio Güemes between January 2017 and May 2022 were analyzed.
The initial surgical specimen (cone) was sent to pathology referenced within Hour 12 (orientation based on clock hours) and was completely processed in order to perform a complete analysis of it (if it is the product of a hysterectomy, the cervix is processed separately). The specimen was painted: anterior lip-H12: black; posterior lip-H6: green - (Figure 1). The vertex (endocervical margin) was dissected and embedded in a paraffin block. The rest of the piece was sectioned into sagittal parallel sections (in the perpendicular direction in which the cone was painted), then these slices are separated and included separately (Figure 2).
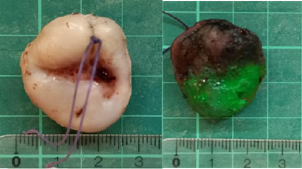
Figure 1 Conization piece. Anterior face (with reference in H12) and posterior face (with corresponding staining).
At the lower genital tract pathology section, the clinical variables of the patients were systematically registered. The baseline characteristics of patients were observed and recorded. The variables of the present study that were considered were: age, smoking (number of Pack Year, p/y), initiation of sexual relations (IRS), number of sexual partners (NPS), immunocompromise, endocervical curettage (ECC) pre-conization and number of quadrants involved in the surgical cone piece.
The information was subsequently categorized in an electronic database designed specifically for the study, including only patients who underwent re-conization/hysterectomy and exhibited involvement of the endocervical margin in a cone surgical specimen. Thus, the patients were divided in two groups: those with residual injury in the surgical specimen and those without injury.
Data was obtained from 43 patients who had positive cervical conization specimen margins at our institution in the time period described above. Two patients who only had the exocervical margin involved and also 11 patients who did not meet the inclusion criteria were excluded (Figure 3). Among participants (30), all were reoperated (16 underwent re-conization, while in 14 patients it was decided to have a total hysterectomy). Of the total number of patients who underwent a new surgical procedure, residual disease was found in 10 patients (33.3%) in the new piece, while 20 patients (66.6%) had no lesion present.
Statistical analysis was performed with the Epi Info program and p < 0.05 was considered significant.
Of a total of 30 patients who were included in the study due to compromised endocervical margins in the initial cervical conization piece, 10 (33.3%) presented residual disease in the surgical piece and 20 (66.6%) did not present the same. The participants were divided into two groups, 2 groups were divided: those with residual lesions formed group 1 and those without residual lesions formed group 2 (Table 1.).
|
|
Group 1 |
Group 2 |
|
Age |
43.5 (29-68) |
37.65 (22-61) |
|
IRS |
17 (15-20) |
15.4 (14-19) |
|
NPS |
6.1 (2-15) |
9.05 (1-30) |
Table 1 Subdivision of groups according to presence or absence of residual disease and distribution of risk factors in each group
The average age was 43.5 years in group 1 and 37.65 years in group 2. The average age of IRS was 17 years in group 1 and 15.4 years in group 2. While analyzing the NPS it was 6.1 and 9.05 respectively. Parity was 0.5 in group 1, while in group 2 it was 1.55.
In group 1, 20% of the patients had immunocompromise, while in group 2 the value was 10% (RR 1.83 95% CI 0.69-4.84, p 0.53)
Regarding the analysis of tobacco consumption, the patients were divided according to it (defining consumption of more than 10 p/y as a variable): thus it was seen that in Group 1, 40% of the patients were smokers who consumed more than of 10 p/y, while in Group 2 only 20% (RR 1.62 95% CI 0.52-5.06, p 0.84) (Table 2).
|
|
Group 1 (n=10) |
Group 2 (n=20) |
RR (CI%95) |
p |
||
|
|
n |
% |
n |
% |
||
|
Immunocompromise |
2 |
20 |
2 |
10 |
1.83 (0.69-4.84) |
0.53 |
|
TBQ (>10 p/y) |
4 |
40 |
4 |
20 |
1.62 (0.52-5.06) |
0.84 |
|
ECC precone |
7 |
70 |
11 |
55 |
1.55 (0.49-4.85) |
0.65 |
|
Extension (4 quadrants + channel) |
9 |
90 |
7 |
35 |
7.87 (1.13-54.66) |
0.01 |
Table 2 Statistical analysis of risk factors in each subgroup
It should be noted that the patients in Group 1 who were immunocompromised (diagnosed with HIV and Lupus with chronic treatment with corticosteroids) had smoking as a common factor, unlike the immunocompromised patients corresponding to group 2 who did not present this history.
Regarding the study of the ECC carried out prior to performing the extended biopsy, it was observed that it was positive for H-SIL in 70% of the patients who belonged to group 1, while in the patients of Group 2 it was positive in 55% of cases (RR 1.55 95% CI 0.49-4.85, p 0.65).
The number of quadrants and involvement of the canal in the surgical piece (1st Cone) were also analyzed as a criterion for the extent of the injury. It was seen that in Group 1, 90% of the patients had involvement of four quadrants in addition to the endocervical canal in the initial conization piece, and only 10% of them did not present involvement of the canal; on the other hand, in Group 2, 35% of the patients had involvement of four quadrants in addition to the endocervical canal in the initial conization piece and the remaining 65% did not have the canal involved with variable involvement of the quadrants of the cervix (RR 7.87 CI 95 % 1.13-54.66, p 0.01)
With a focus on cervical cancer detection, the population of patients with precancerous cervical lesions is on the rise. Anticipating the early-stage development of the disease or potential adverse consequences linked to treatment is crucial.. Furnishing compelling evidence for personalized patient treatment is paramount.10
The American Society for Colposcopy and Cervical Pathology (ASCCP) in 2019 asserted that resection was superior to ablative therapy for H-SIL,11 while the World Health Organization (WHO) opposed cold knife conization as the primary option.12 The consensus among experts from the Chinese Society of Eugenic Sciences for Colposcopy and Cervical Pathology (CSCCP) also lacked pertinent recommendations on surgical methods for cervical lesions. The choice of the surgical method primarily relies on the subjective judgment of the surgeon.
In our center, all patients received conization using an electrosurgical knife as the initial treatment for H-SIL. Those patients exhibiting residual lesions in the surgical specimen and undergoing re-intervention with re-conization or total hysterectomy were included. We scrutinized the risk factors that could influence positive margins in the re-conization and total hysterectomy specimens in these patients.
Most reports indicate that positive endocervical margins are associated with postoperative persistence/recurrence. A recent meta-analysis by Arbyn et al.13 summarized 97 studies involving over 44,000 women undergoing conization, revealing a positive margin rate of 23.1%. The risk of persistent lesions in surgical specimens with positive margins was four times higher compared to those with negative margins. However, negative margins also had a persistence rate of 1.8%, which may be due to the presence of an omitted H SIL lesion. The reason for this phenomenon is that the ectocervix can be accurately estimated through colposcopy; however, judging the depth of the lesion, especially when the transformation zone is not fully observed, is challenging. Therefore, patients with positive endocervical margins should be subjected to a stricter surveillance strategy, and some may require repeated conization or hysterectomy.14
Our study reveals that out of a total of 30 patients with compromised endocervical margins in the initial cervical conization specimens who underwent further surgical treatment (conization or hysterectomy), 33.3% still had residual lesions (H SIL or higher), while in 66.6% of the specimens, no pathology was observed. This finding was consistent with the reported incidence ranging from 5.4 to 60% in previous studies.15,16
In relation to risk factors associated with residual lesions, the literature demonstrates that age, menopausal status, lesion grade, and margin status were related to residual lesions after conization.17,18
Despite the findings of previously studies, the importance of positive conization margins remains controversial: some studies argue that positive margins are significantly associated with residual lesions in the subsequent resection and with recurrent intraepithelial neoplasia.19–22 Others have shown that many relapses also occur in the group of patients with unaffected conization margins.21,23
Several explanations are proposed for this situation. If the surgical specimen shows clear margins, and there is a recurrence/persistence of the disease, it could be explained by a surgeon's error in omitting some compromised margins, the loss of dysplastic epithelium from the compromised margin due to its friability during surgery, or, in some instances (rare), cervical intraepithelial neoplasia may represent a multifocal disease (and not all foci have been eliminated) or an entirely new occurrence (de novo).21,23–25
Similarly, there are various explanations for the absence of disease when cone margins are involved with high-grade lesions. On one hand, the apparent cone margins may not represent the actual resection lines; post-conization endocervical curettage (ECC) can eliminate the disease, and the use of cauterization for hemostasis as well, as it can destroy dysplastic foci.19,23
In our study, the variable that demonstrated an impact was the percentage of lesion extension, significantly affecting the persistence/recurrence of disease in subsequent surgical specimens. Within Group 1 (33.3% with residual lesion in re-conization/ hysterectomy specimens), 90% of patients had involvement of all four quadrants in addition to the endocervical canal in the initial conization specimen, while only 10% of them showed no canal involvement. In contrast, in Group 2 (66.6% without residual lesion in re-conization/hysterectomy specimens), where 35% of patients had involvement of all four quadrants in addition to the endocervical canal in the initial conization specimen, and the remaining 65% showed no canal involvement with variable quadrant compromise of the cervix. This finding could be of great importance when defining a therapeutic approach and patient follow-up.
In our research, the majority of patients (66.6%) did not present residual lesions in subsequent resection specimens. This information brings us closer to recent literature reports where the compromised endocervical margin, although valuable in estimating the risk of persistence/recurrence of disease, lacks information about other risk factors that estimate the follow-up pathway.
We did not obtain statistically significant results in the study of risk factors such as smoking, immunocompromise, and pre-conization ECC. It is important to clarify that cervical conization or hysterectomy was performed based on criteria such as the patient's older age, fertility desires, immunocompromised status, smoking, economic conditions, and poor compliance with follow-up.
An essential point to consider is the immune response, as it may be responsible for the development of precancerous and cancerous lesions.26 Currently, there is high-certainty evidence that HPV vaccines protect against cervical cancer in adolescents and women vaccinated between the ages of 15 and 26. The protection is lower when a portion of the population is already infected with HPV. Longer-term follow-up is needed to assess the impact on cervical cancer.27
This study had several limitations. Firstly, it was a retrospective single-center study, which may limit the generalization of our results to a broader geographic area. Secondly, the small sample size makes it challenging to precisely estimate the correlation between lesion extent, margin status, and residual lesions. Thirdly, we did not evaluate the post-initial conization endocervical canal because it was not systematically performed in all patients.
The most crucial risk factor to consider in re-conization and hysterectomy specimens with residual lesions is the percentage of extension of the initial lesion, as it significantly influences the persistence/recurrence of the disease.
We should bear in mind that a positive endocervical margin is an important but not the only, nor an independent factor to estimate the follow-up and the need for retreatment in patients, considering the option of strict monitoring for them.
None.
None.
Authors declare that there is no conflict of interest.

©2024 Caviglione, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.