eISSN: 2377-4304


Research Article Volume 7 Issue 5
Department of Obstetrics and Gynecology, KK Womens and Childrens Hospital, Singapore
Correspondence: Joella Ang Xiao Hong, Department of Obstetrics and Gynaecology, KK Women's and Children's Hospital, Singapore, Tel 65-8488-3650, Fax 65-6293-7933
Received: June 12, 2017 | Published: August 11, 2017
Citation: Hong JAX, Mathur M (2017) Resident Quality Improvement Project: Antenatal Magnesium Sulfate Protocol for Fetal Neuroprotection in Preterm Births. Obstet Gynecol Int J 7(5): 00265 DOI: 10.15406/ogij.2017.07.00265
Introduction: Postgraduate medical education has transitioned to the new holistic Residency programme with emphasis on developing leadership skills. As part of the Sing Health Obstetrics and Gynaecology Residency curriculum, residents are required to complete a Quality Improvement (QI) project. A group of residents, the Resident Quality Improvement (RQI) team, sought to increase the rates of antenatal magnesium sulphate (MgSO4) use for fetal neuroprotection.
Methods: The residents completed online modules and attended workshops that taught QI concepts and tools. By using Ishikawa and Pareto charts, root causes were identified as lack of protocol and knowledge. Using the SCAMPER methods of Adopt and Modify, a protocol was developed after multidisciplinary discussions and educational talks conducted during meetings. The protocol was implemented in July 2015. A prospective single-centre study was conducted and included all preterm births less than 32 weeks gestation from July 2015 to June 2016. If eligible for the protocol, women were to receive a bolus dose of 4g of MgSO4 and an infusion of 1g per hour until delivery of the baby or maximum of 24 hours. Medical records were reviewed to determine the demographics, rate of antenatal MgSO4 and neonatal outcomes.
Results: Following protocol implementation, the overall rate of antenatal MgSO4 use increased from 14.0% to 63.5% (p=<0.001). Its use for fetal neuroprotection alone increased from 0.9% to 49.7%. (p=<0.001). Of the 109 eligible women, 94 (86.2%) of them received treatment. Despite their smaller sizes and younger gestation, there was a trend towards lower rates of neonatal death and severe neurological injury. For their efforts, the RQI team received the National Team Excellence (Gold) Award in 2016.
Conclusion: Our study highlights the success of a resident-led QI project to increase the antenatal use of MgSO4 for fetal neuroprotection. A “bottom-up” approach is effective as it gives control and power to the staff working on the ground. They identified potential problems and catered solutions to their own needs. The holistic Residency programme ensures that our future specialists are equipped with essential quality improvement and leadership skills essential to the progress of our healthcare system.
Keywords: Enhancing Performance; Quality improvement; Magnesium Sulphate; Fetal Neuroprotection
QI: Quality Improvement; RQI: Resident Quality Improvement; MgSO4: Magnesium Sulfate; ACGME-I: Accreditation Council for Graduate Medical Education International; IHI: Institute of Healthcare Improvement; EPIC: Enhancing Performance, Improving Care; PDSA: Plan-Do-Study-Act
Postgraduate medical education has seen changes in the recent years, the world over. In Singapore, postgraduate medical education underwent a major transition in 2010 from the Basic and Advanced Specialist Training system overseen by the Joint Committee on Specialist Training by the Specialist Accreditation Board to the new Residency system modeled on the American Residency Programme. This new Residency system has been successfully accredited by the Accreditation Council for Graduate Medical Education International (ACGME-I). There have been significant enhancements in the postgraduate training system with increased emphasis on structured and formative training, and a particular focus on developing leadership skills as well as research and quality improvement (QI) concepts among the doctors in training. Components to the new ACGME-I Residency core competencies include Patient Care, Medical Knowledge, Practice Based Learning and Improvement, Systems Based Practice, Professionalism and Interpersonal Skills and Communication.
The Sing Health Obstetrics and Gynecology Residency is a six-year seamless training programme. As part of Systems Based Practice in our curriculum, residents in their second and third year of training are required to participate and complete a QI Project. A group of five obstetrics and gynecology residents in their second and third year of training formed the Resident Quality Improvement Team (RQI) Team. They sought to increase the rate of use of antenatal magnesium sulfate (MgSO4) for fetal neuroprotection over twelve months. The Cochrane review of trials reported in 2009 that the antenatal use of MgSO4 in mothers at risk of preterm birth reduces the risk of cerebral palsy in children by 32% and substantial gross motor dysfunction by 39%.1 MgSO4 is widely used in obstetrics in the treatment of severe pre-Eclampsia and impending Eclampsia and its excellent safety profile has been documented. As such, the administration of antenatal MgSO4 has been recommended by the Canadian2 and Australian3 guidelines for women with imminent preterm birth. In the KK Women’s and Children’s Hospital, the rate of use of MgSO4 for fetal neuroprotection was approximately zero percent. The RQI Team noted the potential to improve the quality of patient care and sought to increase the rates of antenatal MgSO4 use. This study aimed to assess the success of a resident-led quality improvement project to increase the antenatal use of MgSO4 by implementation of a protocol.
We conducted a single-centre prospective study in KK Women’s and Children’s Hospital, Singapore which is a tertiary care referral centres with a Maternal-Fetal Department managing high risk obstetric cases. Our centre accounts for approximately 12,000 deliveries per annum. The study period was from 1 July 2015 to 30 June 2016. A group of five Sing Health Obstetrics and Gynecology residents in their second and third year of training mentored by three labour ward consultants formed the RQI team. Their aim was to improve the rate of use of antenatal MgSO4 for fetal neuroprotection to over twelve months. Residents were required to complete the online Institute of Healthcare Improvement (IHI) modules on quality improvement. After successfully completing the modules, residents then attended the Sing Health Enhancing Performance, Improving Care (EPIC) workshop. This workshop gives residents the opportunity to learn principles of quality improvement and apply systematic quality improvement methodology. During these workshops, they are guided in developing and conducting a quality improvement project to implement changes during their residency training. Residents are also taught on the Plan-Do-Study-Act (PDSA) Cycle for learning and improving.
To identify the problem of lack of antenatal MgSO4 use, we conducted an audit to assess the rate of antenatal MgSO4 for the preceding year. Surveys were conducted to assess the baseline knowledge of the use of antenatal MgSO4 in fetal neuroprotection, identify reasons for the lack of use and to identify potential barriers to the protocol implementation. We used the Ishikawa Diagram (Figure 1) to identify potential causes leading to the lack of use of antenatal MgSO4 and classify these causes in a clear and concise manner. The Pareto chart (Figure 2) was also another tool used to identify the root causes leading to the lack of use of antenatal MgSO4. The root causes for the lack of use were narrowed down to the lack of protocol and lack of knowledge.
To develop a solution to the problem of lack of antenatal MgSO4 use, the SCAMPER technique was employed. Based on the SCAMPER technique of Adapt, the team decided to emulate other institutions such as the Society of Obstetrics and Gynecology Canada and the Australian National Clinical Practice Guidelines that have protocols for the administration of antenatal MgSO4 for fetal neuroprotection. We sought advice from senior neonatologists, senior anesthetists and pharmacists during the drafting of the protocol. Nursing managers were also involved in discussions to streamline the labour ward processes and disseminate the changes to nursing and midwifery staff. The protocol was approved by the Labour Ward Working Committee and was implemented on 1st July 2015. The protocol can be found in every labour ward room as a hardcopy. In our protocol, all women with a singleton, twin or triplet pregnancy were eligible to receive MgSO4 if they were admitted with a viable fetus at less than 32 completed weeks of gestation with a planned preterm delivery or when imminent preterm birth was expected. Imminent preterm birth was defined as active labor with cervical dilatation of ≥ 4cm, regular contractions, with or without preterm premature rupture of membranes (PPROM). These women would receive antenatal MgSO4 as a 4g intravenous loading dose over 15 minutes, followed by a 1g per hour infusion of MgSO4 maintenance until delivery of the baby or for a maximum duration of 24 hours. For women with planned preterm delivery, MgSO4 was to be started at least 4 hours prior to delivery. Repeated dosing was not recommended in our protocol. We chose to use the same dosage and regime as our hospital’s protocol for ecliptic seizure prophylaxis to streamline our labor ward processes.
Relative contraindications for MgSO4 administration were defined as follows:
In addition, we utilized the SCAMPER technique of Modify by building on current meeting sessions such as the Labour Ward Handover Meetings and National Training Programme as a platform to teach medical staff about the use of antenatal MgSO4 for fetal neuroprotection. The team felt that it was a justified decision as this would allow the team to capitalize on the strong attendance seen at such meetings to disseminate necessary information to the relevant staff. Women with severe pre-Eclampsia or impending Eclampsia would receive MgSO4 for seizure prophylaxis as per our local labour ward protocol, in keeping with the recommendations from the National Institute for Health and Care Excellence.4
The primary outcome for this study was the proportion of women delivered before 32 completed weeks of gestation who received MgSO4 before delivery. Based on three prior implementation studies5-8 assessing the feasibility of implementing a protocol for fetal neuroprotection with antenatal MgSO4, we considered the implementation procedure successful if 60% of all eligible women received the treatment during the study period. Secondary outcomes included neonatal outcomes and maternal safety and adverse side effects. Neonatal medical records were reviewed to assess neonatal death, 5 minute APGAR score<7, intraventricular hemorrhage of grades III and IV according to cranial ultrasound findings, paraventricular leukomalacia and necrotizing enterocolitis grades II and III. Data analysis was performed using the χ2, Fisher’s exact test and two-tailed t-test with the R software. Statistical significance was defined as a p-value of <0.05. The protocol and study was approved by the Sing Health Centralized Institutional Review Board (CIRB).
In order to understand possible reasons for the lack of use of antenatal MgSO4, the team devised an Ishikawa Diagram (Figure 1) to conduct possible root cause analysis. Listed in the diagram are the possible root causes determined after a brainstorming session defined in the areas of People, Methods, Materials and Environment. A survey was conducted in the KK Women’s and Children’s Delivery Suite on 42 staff members to verify root causes for current lack of antenatal MgSO4 use and to identify potential barriers to implementation of solutions. The survey showed that 85.7% (n=36) of the survey respondents actually knew that MgSO4 could be used for fetal neuroprotection. The main reasons for the lack of antenatal MgSO4 use listed by the respondents included the lack of hospital protocol (n=38, 90.5%), lack of knowledge (n=3, 7.1%), and peer pressure as no one else was using MgSO4 for fetal neuroprotection (n=1, 2.3%). The team then used the Pareto Chart (Figure 2) to identify final root causes by ranking the possible root causes in descending order according to the number of staff who found each root cause an issue. This was to identify significant factors to focus our efforts on. The final two root causes were identified as the lack of protocol and the lack of knowledge. The protocol was implemented on 1st July 2015 and there was a total of 11,854 deliveries during the study period from July 2015 to June 2016 in KK Women’s and Children’s Hospital. Of which, 1282 deliveries were preterm (less than 37 week of gestation) and 184 babies were born to 159 women were less than 32 completed weeks’ gestation.
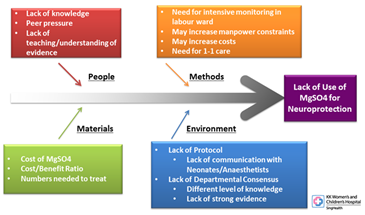
Figure 1 showing the Ishikawa Diagram identifying possible root causes leading to the lack of antenatal MgSO4 use.
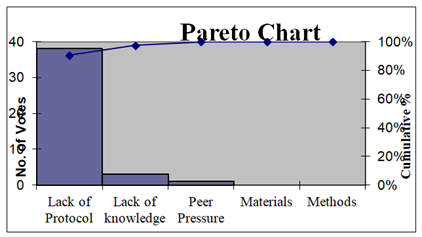
Figure 2 The Pareto Chart identifying the final two root causes leading to the lack of antenatal MgSO4 use.
Figure 3 shows the rate of antenatal MgSO4 use in women less than 32 completed weeks of gestation. In our study period, 101 women received antenatal MgSO4, of which 79 women received it for fetal neuroprotection alone. A total of 58 women did not receive antenatal MgSO4. Following the implementation of the study protocol the rate of antenatal MgSO4 use for any indication increased to 63.5% from a baseline rate of 14.0% (Jul 2014 to Jun 2015) (p=<0.001), while its use for fetal neuroprotection alone increased from 0.9% to 49.7%. (p=<0.001). Figure 4 shows the rate of MgSO4 use in women that were eligible. Of the 109 women that were eligible, 94 (86.2%) of them received antenatal MgSO4. In our study population, 50 women were not eligible for the protocol due to severe fetal anomalies (6/50), maternal or fetal conditions requiring immediate delivery (25/50) and precipitous delivery or complete birth before arrival (19/50) to the hospital. There were no reported maternal adverse effects. Table 1 shows the characteristics of the women who delivered less than 32 weeks of gestation and their babies. The mean maternal age was 31.6 years while the mean gestation age of our cohort was 28.1 weeks. Women who received antenatal MgSO4 were significantly older than women that did not receive antenatal MgSO4 treatment. (32.4 ± 5.6 years versus 30.2 ± 6.1 years, p=0.018).
The main reasons for preterm birth were preterm labor, preterm premature rupture of membranes (PPROM) and pre-Eclampsia. The rate of MgSO4 use in women delivered for pre-Eclampsia was significantly higher. The rate of normal vaginal delivery tended to be lower in women who received antenatal MgSO4 than in women who did not receive MgSO4. The rate of completed antenatal corticosteroid therapy was also significantly higher in women who did receive antenatal MgSO4. Mean birth weight was 1152g and mean head circumference was 24.8cm. Babies whose mothers received antenatal MgSO4 had significantly lower mean gestational age and mean birth weight compared to babies whose mothers did not receive antenatal MgSO4. (27.9±2.4 weeks versus 28.6±2.6 weeks, p=0.040 and 1100±355g versus 1234±434g, p=0.024 respectively). There was a significantly higher rate of cord pH less than 7.1 and need for adrenaline during resuscitation in babies whose mothers did not receive antenatal MgSO4. (p=0.012 and p=0.025 respectively). The rate of neonatal death, severe neurological disability, cord lactate>5 and external cardiac massage were non-significantly higher in babies whose mothers did not receive antenatal MgSO4 treatment.
|
All Women n=159 |
MgSO4 n= 101 |
No MgSO4 n= 58 |
P-Value |
||||
|
Total number of babies |
184 |
113 |
71 |
||||
|
Characteristics |
|||||||
|
Maternal age, mean (years) |
31.6 ± 5.9 |
32.4 ± 5.6 |
30.2 ± 6.1 |
0.018 |
|||
|
Gestational age, mean (weeks) |
28.1 ± 2.4 |
27.8 ± 2.4 |
28.6 ± 2.5 |
0.052 |
|||
|
Birth weight, mean (g) |
1152 ± 392 |
1100 ± 355 |
1234 ± 434 |
0.024 |
|||
|
Nulliparous |
77 |
-48.40% |
46 |
-45.50% |
31 |
-53.40% |
0.427 |
|
Completed corticosteroid therapy* |
116 |
-73.00% |
86 |
-85.10% |
30 |
-51.70% |
<0.001 |
|
Reasons for Preterm Delivery |
|||||||
|
Preterm Labor |
60 |
-37.70% |
34 |
-33.70% |
26 |
-44.80% |
0.219 |
|
PPROM^ |
36 |
-22.60% |
23 |
-22.80% |
13 |
-22.40% |
1 |
|
Pre-Eclampsia |
29 |
-18.20% |
27 |
-26.70% |
2 |
-3.40% |
<0.001 |
|
Abruption placenta |
11 |
-6.90% |
4 |
-4.00% |
7 |
-12.10% |
0.1 |
|
Non-reassuring fetal status |
10 |
-6.30% |
5 |
-5.00% |
5 |
-8.60% |
0.531 |
|
Ante partum hemorrhage |
5 |
-3.10% |
3 |
-3.00% |
2 |
-3.40% |
1 |
|
IUGR# |
5 |
-3.10% |
3 |
-3.00% |
2 |
-3.40% |
1 |
|
Others |
3 |
-1.90% |
2 |
-2.00% |
1 |
-1.70% |
1 |
|
Mode of Delivery |
|||||||
|
Vaginal Delivery |
52 |
-32.70% |
27 |
-26.70% |
25 |
-43.10% |
0.052 |
|
Breech Delivery |
3 |
-1.90% |
3 |
-3.00% |
0 |
0.00% |
0.301 |
|
Caesarean Section |
104 |
-65.40% |
71 |
-70.30% |
33 |
-56.90% |
0.124 |
|
Neonatal Outcomes |
|||||||
|
Neonatal mortality |
16 |
-8.70% |
7 |
-6.20% |
9 |
-12.70% |
0.145 |
|
Severe Neurological Injury** |
11 |
-6.00% |
6 |
-5.30% |
5 |
-7.00% |
0.531 |
|
Apgar <7 at 5 |
26 |
-14.10% |
16 |
-14.20% |
10 |
-14.10% |
0.994 |
|
Cord pH <7.1 |
9 |
-4.90% |
2 |
-1.80% |
7 |
-9.90% |
0.012 |
|
External cardiac massage |
7 |
-3.80% |
2 |
-1.80% |
5 |
-7.00% |
0.1 |
|
Adrenaline |
6 |
-3.30% |
1 |
-0.90% |
5 |
-7.00% |
0.025 |
|
Maternal-Fetal Infection |
55 |
-29.90% |
34 |
-30.10% |
21 |
-29.60% |
0.88 |
Table 1: showing the characteristics of the women who delivered at less than 32 weeks and their babies.
*: Completed two doses of antenatal corticosteroid; ^: Preterm Premature Rupture of Membranes; #: Intrauterine Growth Restriction; **: Grades III and IV Necrotising Enterocolitis + Periventricular Leukomalacia.
Feasibility and success of the RQI
This study demonstrates the success of a resident-led implementation of a protocol for antenatal MgSO4administration in women of less than 32 completed weeks of gestation for fetal neuroprotection. Overall, 86.2% of mothers that were eligible for antenatal MgSO4 received treatment. The overall rate of antenatal MgSO4 use and its use for fetal neuroprotection alone increased significantly after protocol implementation highlighting its success. To our knowledge, there have been four studies5-8 assessing the feasibility and maternal safety of implementing antenatal magnesium sulfate for fetal neuroprotection. Ow et al.6 reported a rate of 40% after implementation of their guideline and that the MgSO4 infusion was discontinued in 2% of their women due to side effects. Bouet et al.5 & Gibbins et al.7 & Tan et al.8 have also implemented similar protocols in their departments with implementation rates of 51%, 82% and 68% respectively. Our implementation rate of 86.2% is similar to their reported rates. In addition, our discontinuation rate of 2% is comparable to the rates reported in the literature.6,8 Similar to the previous studies, there were no reports of severe maternal adverse effects in our study.
We noted a significant drop in the rate of antenatal MgSO4 use in eligible mothers in October 2015. We attributed this to a changeover in the residents working in labour ward as many were found to be working in a different institution prior to protocol implementation. The RQI team then sent out an email blast to the department updating the staff about the rates of antenatal MgSO4 use and encouraged the continued administration of treatment. The team also put up posters in prominent areas of the labour ward such as in the triage area where the women are first seen, in the different rooms of the labour ward and in the doctor’s lounge. The rates of antenatal MgSO4 use in eligible mothers then improved thereafter. Mean birth weight and gestation age of babies whose mothers received antenatal MgSO4 were significantly lower. This may reflect the heightened vigilance in managing women at a lower gestation age. Despite their lower birth weights and younger gestation, there was a trend towards lower neonatal mortality and severe neurological injury. The implementation was a success and the team received the National Team Excellence (Gold) Award in 2016. The award is a national award by the Singapore Productivity Association, a strategic partner to SPRING Singapore which recognizes individual’s contributions to continuous improvement and innovation.
Reasons for the Success of the RQI
The success of the project may be attributed to the dedicated team members of the RQI Team. In our labour ward, residents are the first line of contact and are responsible for seeing and managing the patients whilst being supervised by the labour ward consultants. Having a resident lead the RQI project was effective as not only were there ongoing platforms for dialogue across all levels of staff; the residents were also involved on the ground. The residents were involved in addressing the initial problem, identifying potential causes, assessing problems encountered during the implementation and suggesting solutions. This “bottom-up” approach is an effective way in ensuring the success of the project as it gives more power and control to the staff working on the ground9 to which they can identify problems encountered and implement innovative solutions that caters to their own needs.10 The team also had dedicated leaders that were keen to embrace and implement change. There was also early and continued engagement of key stakeholders such as senior management staff and involvement of a multidisciplinary team such as neonatologists, anesthetists and nursing and midwifery staff. Moreover, by capitalizing on the strong attendance at the daily Labour Ward Handover Meetings, the labour ward consultants were able to disseminate the information and identify eligible women for antenatal MgSO4. This ensured the high rates of eligible women receiving treatment.
The strength of protocol implementation is further supported by multiple research studies that highlight the role of standardized protocol and guidelines in healthcare in improving patient care by improving consistency of care and providing appropriate recommendations for medical treatment.11,12 The team believed that establishing a standardized protocol would be the most fitting way of introducing use of MgSO4 for neuroprotective intent in the KK Women’s and Children’s Hospital. Moreover, the protocol calls for the same dose and regime that is already present in the labour ward for pre-Eclampsia. By streamlining these processes, the nursing staff could easily adopt the new protocol without necessitating additional training. It has been shown that new information can be integrated more readily if there are pre-existing protocols and practices in place.13
Limitations of the study
One possible limitation of our study is the method is our small sample size and short follow up time. Long term audits will be done to ensure consistent high rates of antenatal MgSO4 use, and to complete the next Plan-Do-Study-Act (PDSA) cycle. Larger studies are required to further assess maternal and neonatal morbidity and to validate the neuroprotective effects of antenatal MgSO4. Long term outcomes such as rate of cerebral palsy and developmental delay requires at least 2 years of follow up of the babies born and data is in the process of being collected now. Also, our audit data were based on both hardcopy and electronic patient records. Timings and dosages reflected may have inherent inaccuracies in the reflection of the actual events.
Lessons Learnt
The “bottom up” approach as discussed earlier is an effective way to implement quality improvement changes. Residents identify problems on the ground and are able to suggest and implement innovative solutions that cater to the needs of the staff on the ground.10 This approach empowers junior residents by considering them as the actual change-makers and implementers of new practices.9 By presenting our successful study at various hospital wide conferences and talks it can also empower and inspire other residents to take a step into initiating other quality improvement projects. Delving deeper, after the successful implementation of this RQI project, residents are now part of the Patient Safety and Healthcare Quality Committee in KK Women’s and Children’s Hospital. The Healthcare Quality arm of the committee is looking into enhancing the Quality Improvement training for mentors and residents. Insights into successful QI training from residents themselves can help identify problems in the current QI training and possible solutions to ensure continued innovation and improvements to our healthcare and postgraduate education system.
The new holistic Residency programme emphasizes on equipping residents with quality improvement and leadership skills early in their training. The Residency programme also gives the residents opportunity for hands-on experience by initiating and conducting their own hospital-wide resident-led QI projects whilst being supervised by mentors trained in quality improvement. While there are merits in the old system of training in preparing their trainees for clinical practice, there was little emphasis on clinical improvement and leadership roles. The new Residency program is thus more structured and holistic, preparing our new generation of doctors to take up additional roles in quality improvement and leadership which is essential in improving our healthcare system.
In conclusion, our study shows that a resident-led quality improvement project to increase the antenatal use of MgSO4 for fetal neuroprotection is feasible. A “bottom-up” approach is effective as it gives more control and power to the staff working on the ground and they are able to identify potential problems and cater solutions to their own needs. We hope that the success of this resident-led QI project will motivate and inspire younger generations of residents to step up and be involved in other hospital-wide QI projects. Also, improvements in the QI training for residents and mentors can be enhanced for continued innovation and improvements to both our healthcare and postgraduate education systems. Moving forward in the new Residency programme, the holistic education for future specialists ensures that they are equipped with essential quality improvement and leadership skills essential in the progress of our healthcare system.
We would like to sincerely acknowledge the contributions of the members of the Resident Quality Improvement Team: Dr Joella Ang, Dr Sheri Lim, Dr Chuah Theng, Dr Ng Zheng Yuan, the labour ward consultant obstetricians Dr Manisha Mathur, Dr Shephali Tagore, Dr Ann Wright, the nurses, midwives and pharmacists of the KK Women’s and Children’s Hospital Delivery Suite. We would also like to acknowledge the contributions of Prof Victor Samuel Rajadurai, Dr Eileen Lew, Ms Irene Quay and Ms Thilagamangai for their valuable input in the development of the protocol.
The authors declare that there are no conflicts of interest.

©2017 Hong, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.