eISSN: 2377-4304


Case Report Volume 4 Issue 1
1Department of Obstetrics and Gynecology, Lincoln Medical and Mental Health Center, USA
2St. George's University, West Indies
3Department of Vascular & Interventional Radiology, Lincoln Medical and Mental Health Center, USA
Correspondence: Malvina Elmadjian, Department of Obstetrics and Gynecology, Lincoln Medical and Mental Health Center, 234 East 149th Street, Bronx, NY, 10451, USA
Received: January 04, 2016 | Published: January 25, 2016
Citation: Rezai S, Elmadjian M, Hastings A, et al. Pyomyoma following uterine artery embolization (UAE) – dual case report and review of literature. Obstet Gynecol Int J. 2015;4(1):33-37. DOI: 10.15406/ogij.2016.04.00097
Background: Leiomyoma commonly referred to, as fibroids are benign smooth muscle tumors of the uterus. Leiomyomas are the most common solid pelvic tumors in women. The most commonly reported symptoms of leiomyoma are abnormal uterine bleeding and increased pelvic pressure. Uterine Artery Embolization (UAE) is a technique performed by interventional radiologists that involves the occlusion of the uterine arteries via a percutaneous femoral artery approach. This is one of many procedures that may be chosen to treat leiomyoma in symptomatic women and results in the devascularization and involution of the tumor. Pyomyoma is a rare condition that occurs when a leiomyoma has become infected and suppurated after infarction. The formation of a pyomyoma can lead to sepsis and death unless treated with aggressive surgical intervention and antibiotics.
Case(s): This manuscript represents two cases of pyomyoma following Uterine Artery Embolization (UAE). The diagnosis and management of such a rare complication is described.
Conclusion: The rarity of pyomyomas often leads to a missed or delayed diagnosis and subsequently life threatening complications such as peritonitis, septicemia, and respiratory distress syndrome may result. Upon confirmation of the presence of pyomyoma surgical intervention in the form of myomectomy or hysterectomy is the primary method of treatment.
Keywords: fibroid, hysterectomy, leiomyoma, MRI, pyometra, pyomyoma, sterile endometritis, uterine artery embolization (UAE)
Leiomyomas of the uterus, or more commonly fibroids, are benign tumors of the smooth muscle of the uterus.1 A substantial number of women have fibroids, some studies show 70% occurrence in white women and 80% occurrence in black women by the age of 50.2,3 Symptomatic fibroids present with heavy and/or painful menses, abdominal discomfort, urinary frequency/retention, and in some cases infertility.2 There are many medical and surgical treatment modalities to treat fibroids including, but not limited to Oral contraceptive Pills (OCPs), Gonadotropin-Releasing Hormone (GnRH) agonists, myomectomy, and hysterectomy. Notably a popular treatment modality for symptomatic leiomyomas is that of the minimally invasive Uterine Artery Embolization (UAE).2–7
Uterine Artery Embolization (UAE) is a technique performed by interventional radiologists who accesses the femoral artery via percutaneous femoral artery catheterization and deliver gelatinous microspheres leading to occlusion of the uterine artery. Supplemental metal coils can also be used to assist in arterial occlusion.2 The result is the devascularization and involution of the leiomyoma.2–7 One study showed that minor post-op complications including vaginal discharge, leiomyoma expulsion, and hematoma formation were higher in groups that had UAE when compared to groups that had Hysterectomy (58% vs 40%) as well as higher readmission rates (11.1% vs 0%). However the same study acknowledged that upon comparison of UAE, myomectomy and hysterectomy, UAE resulted in shorter hospital stay and quicker return to activity.2
A very rare but serious complication known to exist following UAE is that of pyomyoma, a suppurative leiomyoma of the uterus.3,4,8–10 Pyomyoma (suppurative leiomyoma) results from infarction, necrosis, and infection of the leiomyoma.1,3–5,11–16 Pyomyoma is a rare occurrence in the post-antibiotic era. The first case was described in 1871, between that time and 1945, only 75 cases of pyomyoma were reported.3 Only 13 cases have been reported since 1945. In this dual case report, we discuss two patients who reports back to our tertiary care facility post UAE. Subsequent pyomyoma is diagnosed and surgical treatment and recovery is discussed.
The patient is a 46 year old African-American woman, premenopausal P3023 with a long history of uterine leiomyomas and abnormal uterine bleeding (menometrorrhagia). She had multiple hospital admissions in the past for symptomatic anemia and had not had success with medical therapy. She contemplated definitive surgery, however opted for less invasive treatment involving uterine artery embolization. Patient’s comorbidities included obesity, chronic hypertension, hyperlipidemia and newly diagnosed HIV on the same admission. Patient underwent UAE and was discharged in stable condition on post procedure Day #1 but presented to the Emergency Department on multiple occasions after with complaints of lower abdominal and back pain with fever. On several occasions, her symptoms were attributed to postembolization syndrome and she was discharged on oral analgesics. On other occasions, she was admitted and treated with IV antibiotics for pelvic infection.
On post procedure day #72 patient returned to the emergency room with pelvic pain and fever of 101.50F. Pelvic exam revealed normal appearing vulva, vagina, cervix; copious amount of foul smelling tan vaginal discharge and a uterus that was consistent with 24 weeks gestation, B-HCG was negative with CBC of: 9.4x 8.3x24.4x 460x 82.3%, patients last CD4 count was 288, with CD4 % of 32% and a CD4/CD8 ratio of 0.842. Patient was placed on antibiotics Zosyn and Metronidazole to treat the presumptive infectious etiology pending results of blood culture and further workup.
Patients Chest X-ray revealed normal findings. Pelvic ultrasound (Figure 1) showed enlarged uterus 16.9 cm x 10.59 cm x 4.95 cm with heterogeneity compatible with a history of multiple large leiomyomas. There were multiple dirty shadows with ring down densities suggestive of air within the uterine parenchyma. A loculus of fluid within the uterus was also noted (Figure 1). Abdominal CT imaging (Figure 2) (Figure 3) confirmed an enlarged lobular uterus. There were heterogenous multilobular masses with decreased attenuation and numerous foci of internal gas. Findings were most consistent with a necrotic fibroid, lesion measured 20 x 11.4cm. Gas was present within the lesion anteriorly and findings consistent with fluid rather than soft tissue density seen within the adjacent portions of the lesion (Figure 2) (Figure 3). No free intraperitoneal air was noted. Patient was soon after admitted to the Gynecology service with a diagnosis of Pyomyoma.

Figure 1 Patient Number 1, Transvaginal Ultrasound: enlarged uterus 16.9 cm x 10.59 cm x 4.95 cm with heterogeneity compatible with a history of multiple large leiomyomas.
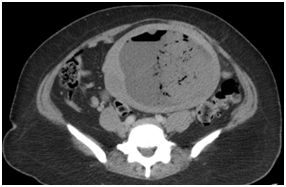
Figure 2 Patient Number 1, Computerized Tomography of Abdomen and Pelvis, Axial View: enlarged heterogenous multilobular masses within uterus, measuring 20 x 11.4 cm, consistent with Infarcted fibroid after embolization with internal gas, air and debris as expected after uterine artery embolization (UAE).
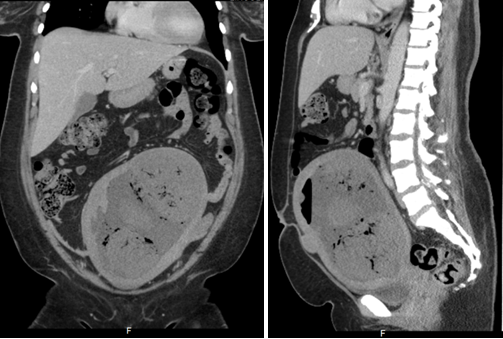
Figure 3 Patient Number 1, Computerized Tomography of Abdomen and Pelvis, coronal and sagittal view: Enlarged heterogenous multilobular masses within uterus, measuring 20 x 11.4 cm, consistent with Infarcted fibroid after embolization with internal gas, air and debris as expected after uterine artery embolization (UAE).
Patient was taken to the operating room and examines under anesthesia. Exploratory laparotomy was performed, enlarged uterus was noted (Figure 4) and total abdominal hysterectomy with bilateral salpingectomy was performed. Postoperative examination of the excised specimen revealed pedunculated intracavitary uterine fibroids with evidence of necrosis and purulence. The uterine cavity was filled with pus (Figure 5) and the intraoperative culture of the endometrium grew E. Coli. The definitive surgical intervention was deemed a success as patient recuperated completely from this infectious post embolization complication and was discharged on post procedure day number 81. The Table 1 summarizes all her hospital visits including her presenting symptoms, objective findings, diagnosis, management and outcome. The images below illustrate the results of preoperative workup as well as intraoperative pictures.

Figure 4 Patient Number 1, Intraoperative picture of a globally enlarged uterus with visible areas of purulence seen at the fundus.
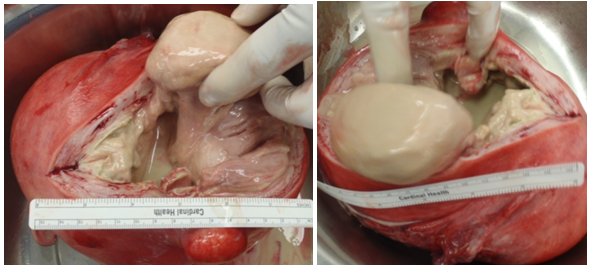
Figure 5 Patient Number 1, Intraoperative pictures showing gross pyometra upon exploration of the uterine cavity.
Date |
Presentation |
Assessment |
Management |
Disposition |
Post Procedure Day 3 |
ER visit for pelvicpain, fever 102.20F, WBC 16.3 |
Post embolization syndrome vs. endometritis |
Admission, triple antibiotics |
Discharged on 11/26/13 |
Post Procedure Day 26 |
Post embolization syndrome |
Pelvic pain due to fibroid ischemia |
Oral analgesics |
Discharged |
Post Procedure Day 37 |
ER visit for pelvicpain |
Post embolization syndrome |
Declined admission for pain control |
Discharged on oral analgesics |
Post Procedure Day 42 |
ER visit for pelvicpain |
Urinary Tract Infection (UTI) |
Antibiotics for UTI and oral analgesics |
Discharged |
Post Procedure Day 48 |
ER visit for pelvicpain |
Degenerating fibroids |
Declined TAH |
Discharged |
Post Procedure Day 52 |
ER visit for pelvic pain and fever |
Pelvic Inflammatory Disease (PID) |
Admissions for IV antibiotics |
Discharged on 1/20/2014 |
Post Procedure Day 68 |
ER visit for pelvicpain |
Degenerating fibroids |
Oral analgesics |
Discharged |
Post Procedure Day 72 |
ER visit for pelvic pain and fever 101.50F. CT showing fibroids with internal gas pockets |
Cannot exclude pyomyoma |
Admission for antibiotics an recommended TAH |
TAH and bilateral salpingectomy on 2/7/14, discharged on 2/11/14 |
Table 1 Summary of clinical course of patient 1
The patient is a 35 year old woman para 1001 with a history of uterine leiomyomas, menometrorrhagia and anemia. Signs and symptoms of anemia were also unresolved despite having an abdominal myomectomy 1-year prior. She was taken back to the operative room for hysterectomy but the procedure was aborted due to extensive, dense, vascular adhesions. The patient opted for a less invasive approach and was subsequently referred to Interventional Radiology for UAE. A uterine artery embolization was performed and the patient was discharged in stable condition on Post Procedure Day #1.
On post procedure day #21, the patient presented to the Emergency Room with complaints of chills, fever, nausea and abdominal pain. Temperature was noted at 103o F and patient had leukocytosis (12.9) with left shift and, urinary analysis was consistent with infection. Chest X-ray was non-contributory, no infiltrates or consolidations noted; patient was started on aggressive fluid resuscitation and Ceftriaxone 2-gram daily and metronidazole. Symptoms later escalated to vomiting and watery diarrhea, both vomitus and diarrhea were non-bloody. Patient also complained of headache, weakness and dizziness and was transferred to the medical intensive care unit (MICU) for management and monitoring of a presumptive diagnosis of sepsis.
The source of sepsis appeared to be uterine in origin, which was supported by radiological findings. Abdominal ultra sound revealed mildly enlarged liver and spleen without focal lesions and normal gallbladder and kidney. Pelvic ultrasound revealed normal ovaries and no fluid in the cul de sac however there were significant findings of enlarged heterogeneous uterus measuring 14.8 x 13.5 by 20cm with possible air within the substance of the uterus, raising the concern for infection (Figure 6). Persistence of the air within the substance of the uterus three weeks post UAE was of concern and prompted abdominal CT. On comparison with CT scans from the past, previously noted enlarged leiomyomatous uterus were replaced by degenerating fibroids, debris and air similar to the findings noted in case number 1 (Figure 7) (Figure 8). A diagnosis of pyomyoma was then made. She was referred to a higher level of care Gynecology Oncology Service for definitive surgery given her history of extensive adhesive disease of the pelvis. Patient underwent hysterectomy due to pyomyoma with sepsis after UAE and had uncomplicated recovery course. Results of intraoperative endometrial cultures revealed positive findings for E. Coli.
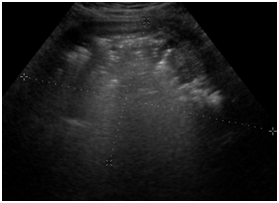
Figure 6 Patient Number 2, Transvaginal ultrasound: enlarged heterogeneous uterus measuring 14.8 x 13.5 by 20 cm with possible air within the substance of the uterus, raising the concern for infection.
Endometritis and sepsis are rare complications associated with UAE. The goal of UAE is to cause ischemia and necrosis of fibroids while preserving the vascularization of the uterus17 as uterine vascularization is back to normal within a few days after embolization of fibroids if proper technique is used. Pyomyomas occur as a result of infarction, necrosis, and subsequent infection of the leiomyoma.11 The ischemic or necrotic area of leiomyoma creates a nidus for organisms to colonize and develop.
Although the true pathogenesis of pyomyoma is not known, a few mechanisms have been proposed, these include:
Direct extension of an infection from the uterine cavity and/or adjacent organs (adnexa/bowel), Hematogenous spread and Lymphatic spread.18
Other sources identify inadequate blood flow to fibroids in the setting of infection as possible as possible predisposing factor to the formation of pyomyoma.13,18 Those with hypertension, hyperlipidemia, diabetes, post-partum, immunocompromised and those with a large dominant leiomyoma are at increased risk for the development of pyomyoma.10,14,19 Though rare, pyomyoma has had other documented links to UAE besides the cases that we presented.4,8,9 Other documented links to pyomyoma include intravenous drug abusers,20 presence of intra uterine devices,1 and hypertension especially when combined with hyperlipidemia.21 Multiple sources have shown an association though not exclusivity of pyomyoma with pregnancy or postmenopausal women who also have underlying vascular disease such as diabetes mellitus and hypertension.1,10
Uterine artery embolization is a viable method of treatment in carefully selected candidates with history of symptomatic leiomyomas.4 UAE is less invasive than other methods of treatment such as Hysterectomy with similar efficacy and relatively less post treatment complications. A major finding in our reports is that both patients developed pyomyoma post uterine artery embolization however prior reports of pyomyoma associated with uterine artery embolization is rare.4,10 Absolute contraindications to UAE include viable pregnancy, coagulopathy and active infection due to risk of abscess formation.8 Relative contraindications to pelvic embolization include immunocompromised states (such as diabetes and HIV), prior pelvic irradiation or surgery, and chronic endometritis or a partially treated pelvic infection.14 Prior to considering a patient for UAE, assessment of risk factors and comorbidities is essential.8 All of these conditions predispose women to a higher risk of an infectious complication.14
It is important to differentiate whether a post UAE patient is suffering from pyomyoma or post embolization syndrome. Postembolization syndrome (PES) consists of abdominal pain, nausea, vomiting and fever that usually subsides after the first few days of onset. The presence of intrauterine infection and exclusion of PES can be determined on the basis of one or more of the following: presence of foul-smelling vaginal discharge, presence of high-grade leukocytosis, clinical course of the initial symptoms (PES occurs within a few days of UAE), and clinical improvement with therapy.7,8 The manifestation of pyomyoma can be subtle, developing within days or weeks after a procedure, as in the cases that we presented. Differentiation of PES with acute fibroid degeneration versus those of intrauterine fibroid infection and pyomyoma formation may be difficult clinically due to non specific signs and symptoms.7,8,11,20 In high-risk patients who present with symptoms of abdominal pain and fever after the first week of UAE, pyomyoma must be considered, and appropriate therapy must be offered.8 When presented with non-specific signs and symptoms cases of pyomyoma are often missed or diagnosis is delayed. In view of this; Patwardhan et al.11 suggest that it might be worthwhile considering prophylactic use of antibiotics in conservative management of fibroid degeneration.11
Among the articles reviewed some authors maintain that the clinical triad of pyomyoma is the presence of leiomyoma uteri, sepsis or bacteremia and the absence of other sources of infection.7,8 One study showed that these criteria are not always reliable as patients failed to be diagnosed half the time.18 Additional findings may include; fever, abdominal pain, weight loss, abdominal mass and leukocytosis.12,14 Differential diagnosis when considering pyomyoma may include pyometra, infected abdominal hematoma, tubo-ovarian abscess (TOA), PES in patients that have undergone UAE and malignancy. High clinical suspicion should be followed up by imaging to confirm the diagnosis of pyomyoma.7–9,18,20,22 Ultrasound or CT often reveals a heterogeneous pelvic mass with gas and debris as seen in the two cases that we presented.7,8 It should be noted though that gas commonly appears in asymptomatic patients post-UAE that are devoid of infection.6,9,15 Imaging results may however prove inconclusive and in such cases laparoscopy may be necessary to confirm the diagnosis of pyomyoma.7,8
When pyomyoma is suspected it is imperative to start aggressive treatment. Delay in treatment could be detrimental as pyomyoma could lead to the development of peritonitis, respiratory distress syndrome (RDS), septic shock, and even death.7,18 Intravenous antibiotics should be attempted first. Traditional surgical approaches to treatment of pyomyoma have been hysterectomy and myomectomy, both cases we reported showed complete resolution of symptoms after total abdominal hysterectomy was performed. More recently other approaches have been introduced such as CT guided drainage23 and Pinto et al.7 discussed laparoscopic approach for drainage and lavage of a perforated pyomyoma. These are also viable approaches to patients desiring to avoid irreversible sterility associated with Hysterectomy and a less invasive alternative to myomectomy and hysterectomy.7
Offending organisms that have been identified from pyomyoma are varied ranging from gram positive, gram negative and anaerobic bacteria.8 The organisms most commonly associated with pyomyoma are enteric bacteria such as streptococci and staphylococci.11 Organisms identified from the intraoperative endometrial culture of our two cases were that of the gram negative, facultative anaerobe Escherichia coli.
The rarity of Pyomyomas often leads to a missed or delayed diagnosis and subsequently life threatening complications such as peritonitis, septicemia, and respiratory distress syndrome may result. The clinical triad pyomyoma is the presence of leiomyoma uteri and sepsis or bacteremia, in the absence of other sources of infection.24,25 A differential diagnosis of pyomyoma should be considered in cases with known uterine fibroids septicemia.11 Imaging consisting of Ultrasound and CT are essential to the diagnosis of pyomyoma.7,8 Upon confirmation of the presence of pyomyoma surgical intervention in the form of myomectomy or hysterectomy is the primary method of treatment.
None.
The authors declare there is no conflict of interests.
None.

©2016 Rezai, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.