eISSN: 2377-4304


Objective: To report the incidence of Natural killer cells peripheral blood (pNK) ≥12% and his relationship with Recurrent Implantation Failure (RIF) in a population of Mexican women.
Methods: Retrospective, cross sectional and observational study that included 74 women with history of RIF, which were subjected to a study to evaluate pNK cell levels in order to avoid complications in future pregnancies. 2 groups were formed: 1) Control and 2) RIF: women with a history of implantation failure and primary infertility (with no history of pregnancies or abortions).
Results: Women in RIF were younger and had higher BMI, compared to the Control. Prevalence of patients with pNK cells ≥12% was statistically higher in RIF than in Control (66.6% vs 20%). RIF showed a significative increase of pNK≥1 cell concentration, compared to Control (12.9±4.6 vs 9.5±0.6, p=0.00). When only women with results of pNK ≥12% were evaluated, RIF showed a level numerically higher than that of the Control (16±1.8 vs 13.5±0.8).
Conclusion: RIF may be the result of increased pNK concentrations and as observed in this study, slightly more than 60% of the Mexican population could be susceptible to abortions.
Keywords: recurrent implantation failure, natural killers, embryo, immunological, delivery
Recurrent Implantation Failure (RIF) is an event that many obstetricians and specialists in assisted reproduction might face. Currently, RIF has several definitions; some authors describe it as an impossibility to achieve a clinic pregnancy after the transference of two embryos of good quality in at least three IVF cycles, where transferences may be done with fresh or frozen embryos (total, 6 embryos), or in at least two ovule donations (total, 4 embryos).1 It is also defined as an impossibility to achieve a clinic pregnancy after the transference of at least 4 embryos of good quality in three or more embryonal transferences in women younger than 40 years old.2 Implantation process depends on 2 main components:
For implantation to be successful, the embryo as well as the endometrium produce mediators (Integrins, MUC 1, COX-2, HOXA 10, LIF, Calcitonin, etc.) that, along with the cytokines produced by lymphocytes [T, B, macrophages, and Natural Killer (NK) cells] from the maternal immune system, support this process.3–6 Among the factors associated to implantation failure, are included those anatomical (uterine anatomic anomalies and thin endometrium), pelvic factors (altered expression of adhesive proteins, hypercoagulative status, immunological disturbances), embryonal factors (genetic abnormalities, hatching alterations (zona pellucida), culture and embryonal transference), energy deficiency and masculine factors.7–8
With respect to immunological disturbances, Th1 and Th2 imbalance, autoimmunity, increase of NK cells (autoimmunity), as well as some combinations of KIR and HLA receptors that disturb the immune balance during pregnancy, have been associated to RIF.9–12
NK cells are found in peripheral blood (pNK cells) (CD16+ CD56dim), contain protein granules involved in lytic activity, and a small amount of cytokines. Their increase in number as well as in activity has been associated to pregnancy loss and implantation failure.9,13 They belong to the innate immune system, their main roll is to defend against tumoral cells by means of cytotoxicity or induced apoptosis.9,14 In uterus, NK cells (uNK) (CD16‒ CD56Bright), have a low cytotoxic activity and produce high concentrations of cytokines, chemokines, and growth factors involved in regulating the trophoblast invasion, angiogenesis process, and remodeling of spiral and uteroplacental arteries.9,15–18 Similarly to pNK cells, an increment of their level may cause reproductive complications such as RIF.19,20
Some of the treatments used to regulate NK cell levels are intravenous gamma-globulins (IVGG), corticoids, anti-TNF, intravenous Intralipid, GMCS-F (Granulocyte and Monocyte Colony Stimulating Factor), PF (Preimplantation Factor), i.v. immunotherapy with lymphocytes and supplementation with D vitamin.9 Particularly, i.v. therapy with parent’s lymphocytes might promote maternal immunomodulation by regulating the levels of pNK, and uNK cells,21 which promotes embryonic implantation.22,23
Accordingly, the present work aims to report the prevalence of pNK cells ≥12% in patients with history of RIF, describing its relationship with what has been reported in literature.
This is a retrospective cross sectional, observational study that included 54 women with RIF history, and 20 women that accepted to be part of the Control group, all of them treated at PRONATAL clinic (Bité Médica Hospital, Mexico City) from 2016 to 2020, to whom a study to evaluate pNK cell levels was made.
Collection of anthropometric data such as age, weight, size, and BMI, as well as the pregnancy history, were taken from medical records. Said information was collected by the nursery staff since the first visit of the patients. pNK cell evaluation was made by taking a peripheral blood sample between days 19-23 of the menstrual cycle (middle of the luteal phase). Samples were sent to Diagnomol laboratory, where the pNK cell count (CD16+ CD56+) was made by flow cytometry.
With the data collected 2 groups were formed:
Inclusion criteria: Women in reproductive age with study of pNK-cell (CD16+ CD56+) level, complete medical record [age, weight, size, BMI, and pNK-cell (CD16+ CD56+) study], idiopathic RIF.
Exclusion criteria: Patients with no pNK-cell (CD16+ CD56+) study, women that did not accept to be included in the study, women with RIF associated to anatomical, endocrine, infectious, genetic, masculine factors, and thrombophilia, as well as women with systemic, genetic, neoplastic, thyroid diseases, diabetes mellitus, and polycystic ovary syndrome. Variables to be studied: pNK-cell level and RIF.
All patients were informed about the use and managing of the data collected [age, weight, size, BMI, and pNK cell (CD16+CD56+) results], which allowed their inclusion in this study. Additionally, their anonymity was kept because there was no reference to the origin of the data, and only numerical and statistical data (as the case might be) were published.
For our analysis, pNK-cell level, age, weight, and size of the mother were reported as the mean ( ) ± standard error (SE), and were subjected to a Student’s t test. On the other hand, pNK cell prevalence was reported as percent (%) and was subjected to a Chi-squared test. In both of the cases, the statistical software SPSS version 25 was used.
Anthropometrical data of 74 women included in a Control (n=20) and a RIF (n=54), were analyzed. When evaluating the data collected, RIF showed a statistically significant decrease in age compared to the Control (33.04±0.4 vs 35.1±0.9, p=0.04). In addition, the weight of the women in RIF group was numerically higher compared the Control (56.1±0.7 vs 53.6±1.2), and height of the women in RIF was numerically higher compared to the Control (1.63±0.009 vs 1.61±0.01). As a result of these data, the BMI was statistically higher in the RIF compared to the Control (21.02±0.3 vs 20.4±0.1, p=0.00) (Table 1).
|
|
Control |
RIF |
p |
|
Age (years) |
35.1±0.9 |
33.04±0.4* |
0.04 |
|
Weight (kg) |
53.6±1.2 |
56.1±0.7 |
0.3 |
|
Height (m) |
1.61±0.01 |
1.63±0.009 |
0.6 |
|
BMI (kg/m2) |
20.4±0.1 |
21.02±0.3* |
0 |
Table 1 Anthropometric measurements of mothers
Within the background of the patients, it was found that Control showed a prevalence of vaginal delivery of 69.4%, and Caesarean delivery of 30.5%. In addition, as the methodology indicated, RIF has no history of deliveries and abortions (Graph 1).
Prevalence of patients with pNK cells ≥12% was higher in RIF than in Control (66.6% vs 20%) (Graph 2).
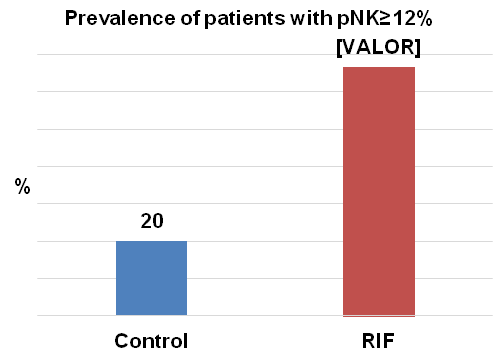
Graph 2 This graph show the prevalence of women with pNK cell levels ≥12% in Control and RIF groups.
Finally, when the evaluation of ±SE of pNK≥1% cell levels from all patients was made, we found that the RIF showed a significative increase of pNK cells compared to Control (12.9±4.6 vs 9.5±0.6, p=0.00). When only women with results of pNK≥12% were evaluated, RIF showed a level numerically higher than that of Control (16±1.8 vs 13.5±0.8). In contrast, when only women with a level of pNK<12% were evaluated, the RIF showed a lower concentration compared to the Control (6.8±1.2 vs 8.5±0.4) (Graph 3).
NK cells are derived from stem cells of the bone marrow. Upon differentiation, they enter the bloodstream where it is thought that by interacting with certain molecules (integrins, and adhesion molecules), they induce migration of pNK cells to the endometrial stroma and the decidua, where they differentiate to uNK cells.24 Although most of pNK immunophenotypes are different, endometrial NK cells have shown a deep relationship between these two populations, exposing in some works pNK cells as predictors of the status of uNK cells, and as an indication of possible RIF.24–26
In our results, we observed that the RIF showed a higher level of pNK≥1% cells when compared to the Control (12.9 vs 9.5%, p=0.00). Likewise, when patients with pNK≥12% cells were evaluated, RIF showed a higher pNK cell level that the Control (16 vs 13.5%) (Graph 3). In turn, the prevalence of patients with pNK cells ≥12% was higher in RIF than in Control (66.6 vs 20%) (Graph 2). All of this reflect that the increment of pNK cells might be associated to more than half of the RIF cases. Similarly, Sacks G. (2012), in a study that included 171 women with RIF, report a significant increase of pNK cell levels at the middle of luteal phase in the RIF compared to the Control (11.3 vs 8.7%).27 Similarly, Santillán I. (2015) found a statistical increment of pNK cells at the middle of luteal phase in 73 patients with RIF compared to a Control group (13.4 vs 8.4%).25 In 2005, Matsubayashi H. reported an increment of pNK cell activity in the follicular phase of patients that could not get pregnant after 6 months or more, compared to women that got pregnant within the same period of time (42.3 vs 34.5%).28
Currently, there is no consensus about the relationship of pNK cell levels and RIF, as shown by Fukui A. (2008) in a study that included 35 women, where they found that the Control group showed a higher pNK cell level than RIF (12.27 vs 8.3%).4 Zhang H. (2019) in a work that included 27 women with RIF, did not find differences when evaluated cytotoxicity levels by substances produced by pNK cells at the middle of luteal phase, such as granzyme B (70.6 vs 68.3%), granulysin (64.7 vs 66.1%), and perforin (61.4 vs 62.3%); and likewise, pNK cell levels showed no difference between groups (14 vs 13.4%).29 Tohma Y. (2020), in a study integrated by 42 women with RIF, found an increment only of uNK cell levels (12.7 vs 9.9%) and not of pNK cell levels (9.8 vs 12.6) sampled at the middle of luteal phase, compared with a Control.30 Ho Y. (2020), in a work with 283 women considered as RIF with pNK cell levels ≤10.6, found that they showed lower implantation rates, which is contrary to what was found in this study.31
Notwithstanding the foregoing, when this work was carried out we found just a few articles evaluating pNK cell levels in patients with RIF, which turns of great importance the realization of prospective studies with a good methodology in order to elucidate whether pNK cell levels at the middle of luteal phase provide information of what is happening in uterus. This would allow to anticipate whether patients have a high probability of RIF caused by a possible rejection of the embryo, if high levels of pNK cells established as abnormal are found. Additionally, the importance of this study lies in the information that, as a clinic (PRONATAL), we may draw from our patients (Mexican population) by evaluating the prevalence of pNK cell level ≥12% associated to RIF.
A little more than 60% of Mexican women with a history of RPL might have pNK cell levels ≥12%, which may be indicative of higher risk of RIF if all of these women would react similarly to those attending to PRONATAL clinic in Mexico City. Data reported in this study reflect a small population, and for this reason it is necessary to carry out more studies in Mexican populations to verify what was found in this work.
None.
None.
The authors report no conflict of interest.

© . This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.