eISSN: 2377-4304


Case Report Volume 15 Issue 1
Gynecology-Obstetrics Department, II– CHU Hassan II- Fez, Morocco
Correspondence: Tazi Zineb, Gynecology-Obstetrics Department, II–CHU Hassan II-Fez, Morocco
Received: January 12, 2024 | Published: February 9, 2024
Citation: Zineb T, Sara B, Sofia J, et al. Ovarian masses and pregnancy: About 2 cases and literature review (experience of Gyneco-obstetrics service 2 Fez). Obstet Gynecol Int J. 2024;15(1):25-27. DOI: 10.15406/ogij.2024.15.00729
Management of adnexal masses during pregnancy can be challenging for the patient and clinician. The specter of a possible malignant tumor may influence the decision to intervene rather than the expected management. The etiologies of ovarian masses vary depending on the age of the parturient, and therefore, benign entities such as functional ovarian cysts, benign cystic teratomas, and serous cystadenomas predominate. In cases of malignancy, these are generally germ cell tumors and borderline, low-grade ovarian tumors. Ultrasound is the primary modality used to detect ovarian masses and assess the risk of malignancy. Morphological criteria identify benign cysts more precisely than malignant tumors. Tumor markers are mainly used to monitor disease status after treatment rather than to establish the diagnosis of ovarian tumor due to lack of specificity, as several markers can be elevated by pregnancy itself (e.g. , CA-125, β-hCG).
We report the cases of 2 patients who consulted the emergency room in a context of pelvic pain during pregnancy whose clinical examination aimed first to eliminate an emergency, notably a torsion of the adnexa, then to explore using ultrasound the etiology and characterize the objectified ovarian mass. The care is specific during pregnancy. Expectant management is recommended for most pregnant patients with asymptomatic, unsuspicious cystic ovarian masses. Surgical intervention during pregnancy is indicated for large and/or symptomatic tumors and those that appear highly suspicious for malignancy on imaging tests. The extent of surgery depends on the intraoperative diagnosis of a benign or malignant tumor. Conservative surgery is most often performed. More aggressive surgery is indicated for ovarian malignancies, including surgical staging. Although rarely necessary, chemotherapy has been used during pregnancy with minimal fetal toxicity in patients with advanced ovarian cancer, in which the risk of maternal mortality outweighs fetal consequences.
Keywords: ovarian masses, pregnancy, tumors, vaginal birth
The incidence of ovarian tumors during pregnancy has increased considerably since the systematic practice of ultrasound in pregnant women, particularly in the 1st trimester.
Adnexal masses are identified in pregnant patients at a rate of 2 to 20 in 1000, approximately 2 to 20 times more frequently than in the age-matched general population.1
The most common types of adnexal masses during pregnancy requiring surgical management are dermoid cysts (32%), endometriomas (15%), functional cysts (12%), serous cystadenomas (11%), and mucinous cystadenomas (8%)2 on the other hand in 2% of cases they turn out to be malignant.3
Surgical intervention during pregnancy is rare since approximately 70% of adnexal masses during pregnancy resolve spontaneously, unless very symptomatic, in the face of a risk of torsion or in cases of suspected malignancy.
Laparoscopic surgery is preferred over open surgery when possible because it has been shown to have fewer complications and less length of hospital stay.
This is a 32-year-old parturient, with no notable pathological history, primigravida, poorly followed pregnancy of 23 weeks according to precise DDR, who consulted for pelvic pain lateralized to the left in a stabbing form preventing walking and any activity without vomiting progressively regressing in intensity; in whom the examination on admission finds a conscious patient, stable on the hemodynamic and respiratory levels normal-colored conjunctiva, afebrile, with on gynecological examination, speculum: gravid cervix with normal appearance , absence of bleeding, no pathological leukorrhea, on vaginal examination coupled with abdominal palpation showing a long closed cervix post, moderate pain on uterine mobilization; no lateral uterine mass, soft abdomen breathes normally, with presence of a mobile mass of hard consistency on palpation at the level of the painful left flank without defense or contracture. Our course of action was to hospitalize the parturient with conditioning (Antispasmodic, Progestogen), carrying out a biological assessment which returned without particularity, an obstetric ultrasound having revealed a progressive single-fetal pregnancy in transverse presentation, homogeneous fundal placenta, amniotic fluid in normal quantity, with a biometry of 23 SA. Furthermore, presence in the lateral uterine of a heterogeneous solidocystic image measuring 87x53 mm, predominantly solid, non-vascularized on Doppler not classified IOTA (Figure 1).
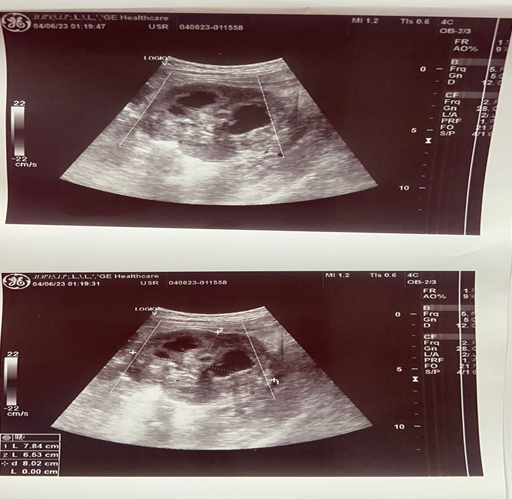
Figure 1 The postpartum consequences are unremarkable with a consultation and ultrasound appointment for management of her myomas.
A pelvic MRI with additional MRI angiography was performed on the patient, revealing the presence of two FIGO 6 and 7 myomas producing reworked left lateral uterine masses (hemorrhagic necrosis and cystic rearrangements) measuring 102 x 74 mm and 98 x 51 mm respectively.
The patient was kept under clinical surveillance, particularly the signs of torsion: pain + vomiting, with fetal monitoring. The pregnancy took place without incident, with an uncomplicated vaginal birth of a new female child. eutrophic, the postpartum consequences are unremarkable with a consultation and ultrasound appointment for management of her myomas.
Case 2
This is a 19-year-old patient, without notable pathological history, 3rd procedure, with only one living child and a spontaneous miscarriage without curettage, who consulted the maternity emergency room for right-lateralized pelvic pain of moderate intensity with minimal metrorrhagia without other associated signs, in particular no vomiting, no urinary symptoms such as urinary burning or pollakiuria on amenorrhea of 7 weeks, in whom the examination on admission finds a conscious patient, stable on the hemodynamic level with a BP 12 /6 and a HR of 80 beats/min, eupneic normal-colored conjunctiva, afebrile at 36.2, gynecological examination, speculum: normal-looking gravid cervix, low-volume bleeding from the endocervix, no pathological leukorrhea on TV +palpate abdominal objectifying pain caused at the level of the right vaginal sac, moreover no lateral uterine mass, no Douglas cries with a cervix of soft consistency. Our course of action was to hospitalize the parturient with conditioning (Antispasmodic, Progestin), carrying out a pelvic ultrasound: intrauterine gestational sacwith LCC embryo of 7 weeks + 5 days, positive cardiac activity, presence in the lateral uterine of a bilocular anechoic image without vegetations or partitions measuring 7.5*6 cm (Figure 2).

Figure 2 The postpartum consequences were unremarkable with a control ultrasound showing no abnormalities.
The patient subsequently benefited from a diagnostic laparoscopy with exploration: gravid uterus of approximately 7 weeks with the presence of a right ovarian cyst of approximately 7 cm, pearly white in color, with smooth wall, without vegetation exocyst, attached to the corpus luteum, otherwise left appendix seen without particularity. Carrying out peritoneal cytology with laparoscopic right cystectomy, the results were unremarkable, the patient having benefited from a depot progesterone injection according to a well-codified protocol, declared discharged with follow-up in prenatal consultation. Histological examination revealed a cystic formation massively remodeled by hemorrhage and bordered by luteal cells. The wall is fibrous and contains an inflammatory lymphoplasmacytic infiltrate suggesting a luteal cyst.
The pregnancy took place without incident, with an uncomplicated vaginal delivery of a new eutrophic female child, the postpartum consequences were unremarkable with a control ultrasound showing no abnormalities.
Aggarwal's meta-analysis grouped 10 series (4 prospective1,4 and 6 retrospectives5,6) reporting that the diagnosis of ovarian tumor is mainly made in the 1st trimester in 40% of cases, in the 2nd trimester in 18% of cases, during the 3rd trimester or at term in 40% of cases, and finally in the postpartum period in 2% of cases. The diagnosis can also be made in the face of a symptomatic pelvic mass such as pelvic pain which is the second mode of discovery of an ovarian cyst or other complications.
Pelvic ultrasound is the ideal tool for initial evaluation of a mass. It allows the positive diagnosis but also to characterize the image in order to orient towards the benign or malignant nature of a mass: the size of the tumor, the morphology and the color Doppler.7
Marino et al.8 used a modification of an ovarian tumor scoring system developed by Lerner et al.9 to determine the risk of malignancy (Table 1).
Risk of ovarian cancer |
Sonographic criteria |
Low |
Cystic, unilocular |
Size <5 cm |
|
Intermediate |
Cystic, multilocular |
Complex |
|
High |
Thin septations |
Solid mass |
|
Nodules |
|
Thick septations |
|
Size 5 cm |
Table 1 Risk of ovarian malignancy based on ultrasound criteria
Ultrasound remains the reference examination but it has its limits during pregnancy due to local conditions where the classic diagnostic signs, for example adnexal torsion, may be missing.10
The use of MRI can be interesting when ultrasound cannot conclude as to the nature of the ovarian cyst. The value of MRI in the tissue characterization of ovarian cysts has already been demonstrated.11 It could make it possible to postpone postpartum intervention for complex or suspicious cysts on ultrasound by asserting more precisely the benign nature of the cyst and by allowing an analysis of the pelvis (peritoneum, lymph nodes), without there being any loss luck for the progress of the pregnancy or fetal well-being. One of our patients underwent an MRI to better clarify the organic nature of the ovarian cyst and postpone surgical intervention with simple monitoring.
CT is not recommended as first intention, due to the irradiation imposed on the pregnant patient.
The biology is not conclusive during pregnancy, in particular the level of CA 125 (ovarian cancer marker). Indeed, CA 125 increases from the start of the 1st trimester and therefore has only a very limited role in the differentiation between benign or malignant tumors. The use of these markers cannot therefore be used for diagnosis.
In the vast majority of cases, ovarian tumors diagnosed by ultrasound during pregnancy are simple cysts (unilocular anechoic, regular wall) of less than 5 cm which will disappear spontaneously. Taking the example of the corpus luteum cyst, it will generally enlarge during the first trimester of pregnancy, then regress from 12 weeks and finally disappear later in the pregnancy.12 In the 4 prospective series with ultrasound monitoring, therefore bringing together 380 ovarian tumors discovered and monitored during pregnancy (except in cases of suspected malignancy or symptoms), the spontaneous regression rate was 69.4%.
But certain functional cysts do not regress, they are responsible for pelvic pain, or even complications leading to intervention during pregnancy. The rate of functional cysts operated on during pregnancy in French retrospective series is approximately 18 and 25%.13 The size of dermoid cysts remains stable and approximately 50% of endometriomas will decrease in size. The rate of decidualization of endometriomas is estimated at 12%, which may raise fears of malignant transformation.
Therapeutic management is based on two options: expectant monitoring or surgical intervention.
Simple monitoring during pregnancy can be carried out with regular clinical and ultrasound monitoring (MRI depending on the case), subject to benignity criteria. This treatment has no harmful impact on the outcome of the pregnancy and the newborn. One of our patients who benefited from close monitoring by ultrasound.
Ultrasound-guided transvaginal fine needle puncture,14,15 can be offered in cases of benign ovarian cyst, it is a less invasive method than surgery. It would reduce complications linked to large ovarian cysts. But it often leads to a recurrence of the cyst and other punctures may be necessary. In France, fine needle puncture is not recommended.
Between laparotomy and laparoscopy, the choice depends on the urgency, local conditions, gestational age and experience of the operator. The gold standard is laparoscopy up to 17 weeks.16,17 The laparoconversion rate is approximately 11% in the literature and 28.57% (2 failures out of 7 laparoscopy attempts), one of our patients having benefited from a laparoscopy with cystectomy.
The discovery of an ovarian mass during pregnancy raises the issue of intervention during pregnancy with the risks that this entails for the mother and the fetus or of abstention with monitoring. The course of action must take into account the benign or malignant nature, the complications that may arise as well as the benefit of the surgery.
None.
None.
All authors declare that they have no conflict of interests.

©2024 Zineb, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.