eISSN: 2377-4304


Research Article Volume 14 Issue 6
Cheikh Anta Diop de Dakar, Senegal
Correspondence: Dr Fatou Samb, Cheikh Anta Diop de Dakar, Senegal, Tel 00221 77 532 32 57
Received: November 16, 2023 | Published: November 27, 2023
Citation: Samb F, Faye PK, Niang MM, et al. Monitoring of pregnancy and labour by cardiotocography: 155 cases from the maternity ward of the institut hygiène sociale Hospital in Dakar. Obstet Gynecol Int J. 2023;14(6):186-194. DOI: 10.15406/ogij.2023.14.00719
Objectives: To determine the epidemiological and clinical profile of patients monitored by cardiotocography, to assess the performance of the device in detecting labour abnormalities and to identify factors influencing the results of cardiotocography.
Patients and methods: We conducted a retrospective, descriptive and analytical study of labour monitoring and pathological pregnancies using the cardiotocograph at the Maternity Unit of the Institut Hygiène Sociale hospital in Dakar over a two-year period from 1 January 2019 to 31 December 2020. All cardiotocographic tracings were subject to a 2nd blind interpretation by a senior. The results were interpreted using the 2007 classification of the Collège National des Gynécologues et Obstétriciens Français (CNGOF). An APGAR score of less than 7 at 1 minute was defined as neonatal asphyxia. Data were collected from the patients' records and entered on a computerised form. Data analysis was performed using SPSS version 22 software.
Results: During the study period, 208 patients were monitored with the cardiotocograph out of a total of 4123 deliveries, i.e. a frequency of use of 5%. Of these, 155 were included in the study (74.5%). These included 118 parturients (76.1%) and 37 pathological pregnancies (23.9%). The epidemiological profile of the patients was that of a woman aged 28 years on average, of low socio-economic status (83.2%), paucigest (48.4%), pauciparous (46.5%), carrying a full-term pregnancy (67.7%) and living outside the South District (72.3%). Ninety-seven FHR tracings contained abnormalities (62.2%). These included 47 pathological FHR tracings (30.1%) and 50 FHR tracings at intermediate risk of acidosis (32.1%). The basic rhythm was most often normal (87.2%). The abnormalities found were bradycardia (4.5%), tachycardia (7.7%) and absent rhythm (0.6%). Variability was mostly normal (78.9%). However, it was reduced in 12.2% of cases. Fifty tracings showed accelerations (32.1%) and decelerations were noted in 49 foetuses (31.4%). These were most often early (16%) or late (7.1%) decelerations. Tocography was mostly normal (60%). The abnormalities noted were dominated by hypertonia (11.7%) followed by hyperkinesia of intensity (7.7%). The majority of patients (54.8%) had given birth by caesarean section and the indications were dominated by the non-reassuring state of the foetus (69.4%). Most of the newborns had an APGAR score greater than 7 at 1 minute (82.7%) and 5 minutes (91.7%). Comparison of the results of the ERCF with the neonatal status revealed 20 true positives, 7 false negatives, 27 false positives and 102 true negatives, giving the ERCF a sensitivity of 74.1%, a specificity of 79.1%, a positive predictive value of 42.1% and a negative predictive value of 93.6% for the diagnosis of non-reassuring foetal status. A bivariate analysis enabled us to identify factors associated with the occurrence of perinatal asphyxia. Basic rhythm abnormalities (p = 0.001) and variability (p = 0.004), hypertension in the pregnant woman (p = 0.034), premature rupture of the membranes of more than 6 hours (p = 0.044) and intrauterine growth retardation (p = 0.013) were significantly associated with the risk of neonatal asphyxia.
Conclusion: Cardiotocography is a powerful tool for monitoring labour, but its effectiveness is influenced by the conditions in which it is performed and the qualifications of the operator.
Keywords: Cardiotocography-ERCF-Labour.
Maternal and neonatal mortality is a public health problem. Worldwide, during 2015, the maternal mortality rate was estimated at 216 deaths per 100,000 live births, or approximately 830 deaths every day.1 The majority of these deaths occur in developing countries, where the rates are highest. Over the same period, in sub-Saharan Africa, the maternal mortality rate was estimated at 546 deaths per 1000 live births, more than double the world average.1 At the same time, perinatal mortality is similarly distributed. In 2013, around 2.8 million neonatal deaths were reported worldwide by UNICEF,2 with the neonatal mortality rate in sub-Saharan Africa exceeding 30 deaths per 1,000 live births, compared with a global average of 20 deaths per 1,000 live births.3
In Senegal, despite the efforts made in recent years to improve indicators, maternal and neonatal mortality ratios remain high. The maternal mortality ratio fell from 434 deaths per 100,000 live births in 20134 to 236 deaths per 100,000 live births in 2017,5 and neonatal mortality from 37 deaths per 1,000 live births in 1997 to 23 deaths per 1,000 live births in 2018.6
The majority of these maternal and neonatal deaths occur during delivery and in the post-partum period.7,8 Optimal monitoring of pregnancy, childbirth and the postnatal period can help prevent them.3 These include focused antenatal consultations and monitoring of labour using the partogram and cardiotocograph. The latter makes an electronic recording of foetal heart rate and uterine contractions. Its use requires training to avoid the risk of misinterpretation, which could lead to inappropriate therapeutic choices. In Zarko's meta-analysis, it was reported that continuous recording of the foetal heart rate during labour was associated with an increase in the caesarean section rate.9
Since 2019, the maternity ward of the Institut d'Hygiène Sociale (IHS) hospital in Dakar has been equipped with a cardiotocograph to improve labour monitoring. After two years of activity, we therefore proposed to carry out this study, the main objective of which was to evaluate our practice in this field. To do this we studied the epidemiological and clinical profile of patients, the performance of cardiotocography in detecting abnormalities in labour and the factors influencing the results of cardiotocography.
The setting for our study was the Maternity Ward of the Institut d'Hygiène Sociale de Dakar (IHS), which has been a level 1 Public Health Establishment (EPS 1) since 2010. It is located in the South District of the Dakar medical region.
We conducted a retrospective, descriptive and analytical study on the monitoring of labour and pathological pregnancies by cardiotocograph over a two-year period from 1 January 2019 to 31 December 2020.
All pregnant women and parturients who received cardiotocographic monitoring during the study period were included in the study.
Patients whose records could not be used (no or uninterpretable cardiotocographic tracings) were not included in our study.
Data were collected on a pre-established computerised form (Appendix 1) from the patients' records. The equipment used was an EDAN F6 cardiotocograph. Tracings were taken on admission to the labour ward, either continuously or discontinuously over a variable period. The tracing speed was 3 cm/min. All cardiotocographic tracings were subject to a 2nd blind interpretation by a senior.
The following parameters were studied: frequency, general patient characteristics (age, socio-economic level, gestational age, parity, previous history), pregnancy follow-up, mode of admission, entry examination data, cardiotocography results, partogram data, maternal and perinatal prognosis and postnatal follow-up.
Data were entered using Excel and analysed using SPSS version 22. In the descriptive analysis, the qualitative variables were described in terms of numbers and percentages, and the quantitative variables in terms of mean, standard deviation, extremes and median. For the analytical part, the Chi-square test was used to compare proportions. The difference was statistically significant when the p-value strictly less than 0.05. The rhythm is normal when it is between 110 and 160 beats per minute (bpm). Tachycardia is defined as a rhythm greater than 160. The cardiwas otocograph results were interpreted using the classification of the French National College of Gynaecology and Obstetrics (CNGOF) published in 2007. Tracings with a low to moderate risk of acidosis were classified as intermediate and those with a high or major risk of acidosis as pathological. An APGAR score of less than 7 at 1 minute was defined as neonatal asphyxia.
Descriptive results
During the study period, 208 patients were monitored with the cardiotocograph out of a total of 4123 deliveries, i.e. a frequency of 5%. Of these, 155 were included in the study (74.5%). These included 118 parturients (76.1%) and 37 cases of pathological pregnancy (23.9%).
The mean age of the patients was 28 years, with extremes of 15 and 43 years. The 20-34 age group was the most represented (71.6%) (Figure 1).
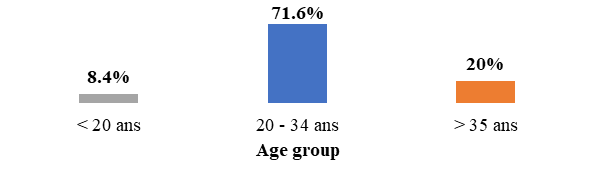
Figure 1 Age distribution of patients who received cardiotocograph monitoring at the IHS maternity unit between 1 January 2019 and 31 December 2020 (N=155).
Almost ¾ of the patients (72.3%) lived outside the South District. Only 25.8% came from the South District and 1.9% from the regions.
The majority of patients (83.2%) had a low socio-economic level, 14.2% had an average level and the remaining 2.6% had a high level.
In our series, paucigravida were in the majority (48.4%), followed by primigravida (39.4%) and multigravida (9%), and large multigravida (3.2%).
The majority were pauciparous (46.5%) and primiparous (45.2%).
Antenatal follow-up
The mean gestational age was 38 weeks' amenorrhoea, with extremes of 30 and 43 weeks. More than half the patients (67.7%) were at term, and 28 (18.1%) had a prolonged pregnancy (Figure 2).
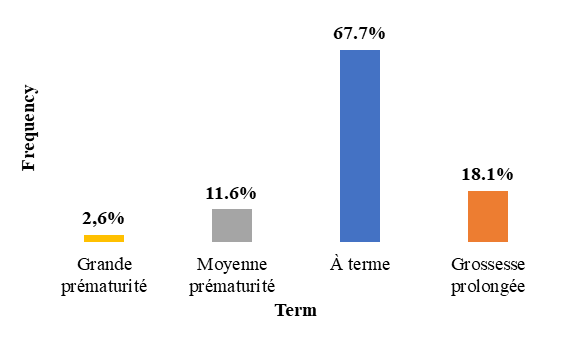
Figure 2 Distribution by term of pregnancy of patients who received cardiotocograph monitoring at the IHS maternity unit between 1 January 2019 and 31 December 2020 (N=155).
Number of antenatal consultations
Nearly ¾ of patients (72.3%) had attended at least 4 antenatal clinics (ANC). One patient (0.6%) had not attended any ANC (Figure 3).
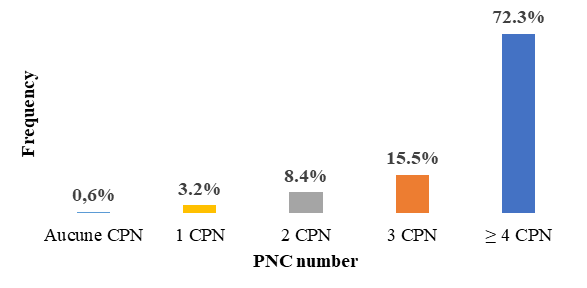
Figure 3 Distribution according to the number of antenatal consultations of patients who received cardiotocograph monitoring at the IHS maternity unit between 1 January 2019 and 31 December 2020 (N=155).
Antenatal assessment
Almost all patients (98.1%) had undergone a prenatal check-up. The results were mostly normal (83.6%). We also recorded 12 cases of anaemia (7.7%) and 9 cases of gestational diabetes (5.8%) (Table 1).
|
Prenatal check-up |
Number |
Frequency (%) |
|
Normal |
129 |
83,6% |
|
Anemia |
12 |
7,7% |
|
Gestational diabetes |
9 |
5,8% |
|
Hepatitis B |
5 |
3,2% |
|
Type 1 diabetes |
1 |
0,6% |
|
Not done |
3 |
1,9% |
Table 1 Distribution according to the results of the antenatal check-up for patients who underwent cardiotocograph monitoring at the IHS maternity hospital between 1 January 2019 and 31 December 2020 (N=155)
Most patients (92.9%) had had at least one ultrasound scan during their follow-up; the average number of scans was 2, with extremes of 0 and 4.
Most ultrasounds were normal (95.1%). Seven patients (4.5%) had abnormalities. These were uterine myomas and severe oligohydramnios (1.3%) (Table 2).
|
Ultrasound results |
Number |
Frequency (%) |
|
Normal |
137 |
95,1% |
|
Myoma |
2 |
1,4% |
|
Severe oligohydramnios |
2 |
1,4% |
|
Anamnios |
1 |
0,7% |
|
Ovarian cyst |
1 |
0,7% |
|
Marginal anterior placenta previa |
1 |
0,7% |
|
Intrauterine growth retardation |
1 |
0,7% |
Table 2 Distribution according to ultrasound findings in patients who had at least one ultrasound and received cardiotocograph monitoring at the IHS maternity hospital between 1 January 2019 and 31 December 2020 (N=144)
Clinical data
In our series, more than half the patients were evacuated (57.4%). The most frequent reason for evacuation was premature rupture of membranes (RPM) (20%), followed by pathological pregnancies (11.6%) and lack of places in the facility of origin (9%). Among patients who came to the centre on their own initiative (42.6%), the most frequent reason for consultation was management of childbirth (28.4%) (Table 3).
|
Admission procedure |
Motifs |
Number |
Frequency (%) |
|
Premature rupture of the membranes |
31 |
20% |
|
|
Vasculo-renal syndrome |
15 |
9,8% |
|
|
Lack of space |
14 |
9% |
|
|
Labour abnormalities |
9 |
5,8% |
|
|
Lack of block |
7 |
4,5% |
|
|
Excessive uterine height |
6 |
4% |
|
|
Intrauterine growth retardation |
2 |
1,3% |
|
|
Evacuated |
Suspicion of macrosomia |
1 |
0,6% |
|
Fetal condition not reassuring |
1 |
0,6% |
|
|
Pregnancy on myoma |
1 |
0,6% |
|
|
Planned caesarean section |
1 |
0,6% |
|
|
Taking decoction |
1 |
0,6% |
|
|
Management of childbirth |
44 |
28,4% |
|
|
Coming from herself |
Amniotic fluid discharge |
11 |
7,1% |
|
Labour abnormalities |
8 |
5,2% |
|
|
Pathological pregnancies |
3 |
2% |
|
|
Total |
|
155 |
100% |
Table 3 Distribution according to reasons for evacuation and consultation of patients who received cardiotocograph monitoring at the IHS maternity hospital between 1 January 2019 and 31 December 2020 (N=155)
Just over half the patients evacuated (56.2%) came from health centres. We also received evacuees from level 1 and 3 hospitals (Table 4).
|
Level of health facility of origin |
Number |
Frequency (%) |
|
Health centres |
50 |
56,2% |
|
Level 3 hospitals |
31 |
34,8% |
|
Level 1 hospitals |
4 |
4,5% |
|
Health posts |
3 |
3,4% |
|
Private clinics |
1 |
1,1% |
|
Total |
89 |
100% |
Table 4 Distribution according to type of referral facility of evacuated patients who received cardiotocograph monitoring at the IHS maternity unit between 1 January 2019 and 31 December 2020 (N=89)
Examination data
The general examination was normal in most patients (78.7%). We counted 33 hypertensive patients (21.3%) including 18 grade 2 (11.6%).
In our series, 118 patients (76.1%) were received in labour and most of them were in the latency phase (64.5%) 1 in the expulsive phase (0.6%) 37 not in labour (23.9%).
Uterine height was mostly normal (91.6%). Excessive and insufficient HU were noted in 5.2% and 3.2% of cases respectively.
Almost all patients (99.4%) were carrying a singleton pregnancy. Only one twin pregnancy was recorded.
In our series, the majority of fetuses were in apex presentation (98.7%). Only 2 (1.3%) were in breech presentation.
Examination of the pelvis was mostly normal (88.4%). We also recorded 7 cases of transversely narrowed pelvis (4.5%), 5 cases of borderline pelvis (3.2%) and 2 cases of surgical pelvis (1.3%), and in 2.6% of cases this examination was not reported.
Labour monitoring
Monitoring of foetal parameters
Fetal heart rate
Basic rhythm: The basic rhythm was most often normal (87.2%). Abnormalities included bradycardia (4.5%), tachycardia (7.7%) and absent rhythm (0.6%) (Figure 4).
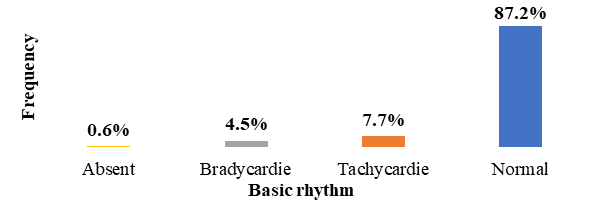
Figure 4 Distribution according to basic rhythm of foetuses born to mothers who received cardiotocograph monitoring at the IHS maternity hospital between 1 January 2019 and 31 December 2020 (N=156).
Variability: In our series, 123 tracings had good variability (78.9%). However, variability was reduced in 12.2% of cases (Figure 5).
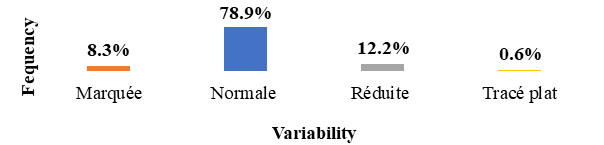
Figure 5 Distribution according to basal rate variability of fetuses born to mothers who received cardiotocograph monitoring at the IHS maternity unit between 1 January 2019 and 31 December 2020 (N=156).
Accelerations: Accelerations were noted on 50 traces (32.1%). However, we recorded one flat trace.
Responsiveness: In our series, responsiveness was assessed in 90 patients (58.1%). The majority were good (51.3%) (Table 5).
|
Reactivity |
Number |
Frequency (%) |
|
Good |
80 |
51,3% |
|
Poor responsiveness |
10 |
6,4% |
|
Not assessed |
66 |
42,3% |
|
Total |
156 |
100% |
Table 5 Distribution according to reactivity on the tracing of foetuses from mothers who benefited from cardiotocograph monitoring at the IHS maternity hospital between 1st January 2019 and 31st December 2020 (N=156)
Decelerations: We noted a deceleration of the FHR in 49 foetuses (31.4%). These were mostly early (16%) and late (7.1%) decelerations (Figure 6).
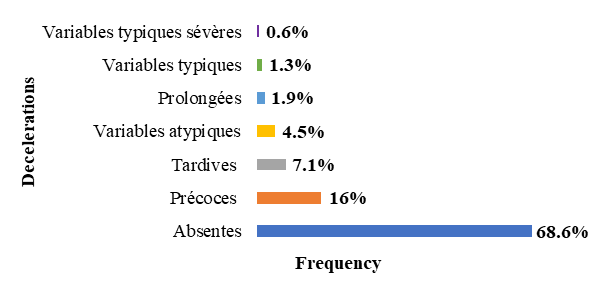
Figure 6 Distribution according to the existence or not of decelerations in fetuses from mothers who received cardiotocograph monitoring at the IHS maternity unit between 1 January 2019 and 31 December 2020 (N=156).
Results of fetal heart rate tracings: Ninety-seven FHR tracings contained abnormalities (62.2%) but 59 were free of abnormalities (37.8%).
Of the 97 abnormal traces, 47 (30.1%) pathological FHR traces were identified. The remaining 50 (32.1%) had intermediate abnormalities (Figure 7).
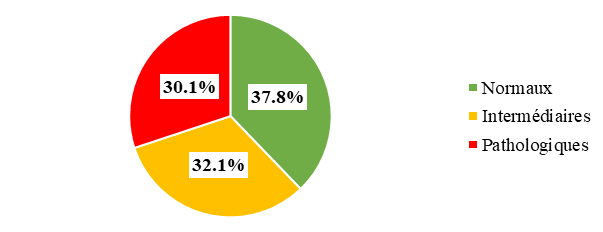
Figure 7 Distribution according to RCF recording results in patients who received cardiotocograph monitoring at the IHS maternity unit between 1 January 2019 and 31 December 2020 (N=156).
Amniotic membranes: In our series, we noted 49.7% premature rupture of membranes and 18.1% artificial rupture. In 21.3% of cases, the membranes were intact (Figure 8).
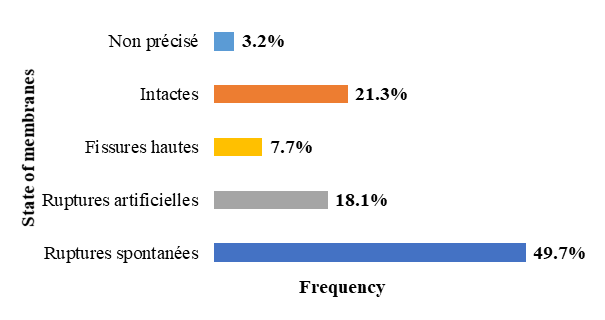
Figure 8 Distribution according to the state of the membranes at the time of labour of patients who received cardiotocograph monitoring at the IHS maternity hospital between 1 January 2019 and 31 December 2020 (N=155).
In patients with ruptured membranes, the appearance of the fluid was most often clear (Table 6).
|
Aspects of amniotic fluid |
Number |
Frequency |
|
Clear |
62 |
53% |
|
Tinted |
36 |
30,8% |
|
Thematic |
4 |
3,4% |
|
Meconial |
4 |
3,4% |
|
Yellowish |
3 |
2,6% |
|
Unspecified |
8 |
6,8% |
|
Total |
117 |
100% |
Table 6 Distribution according to the appearance of the amniotic fluid during labour of patients with ruptured membranes who received cardiotocograph monitoring at the IHS maternity unit between 1st January 2019 and 31st December 2020 (N=117)
Tocography: More than half of the uterine contraction tracings (60%) were normal. The anomalies noted were dominated by hypertonia (11.7%) followed by hyperkinesia of intensity (7.7%) (Table 7).
|
Results of tocography |
Number |
Frequency (%) |
|
Normal uterine contractions |
93 |
60% |
|
Absence of uterine contractions |
24 |
15,5% |
|
Hypertonia |
18 |
11,6% |
|
Hyperkinesia of intensity |
12 |
7,7% |
|
Hyperkinesia of frequency |
7 |
4,5% |
|
Not assessed |
9 |
5,8% |
Table 7 Distribution according to tocography results of patients who underwent cardiotocograph monitoring at the IHS maternity hospital between 1 January 2019 and 31 December 2020 (N=155)
Length of labour: The duration of labour was recorded for 125 patients (80.6%). It was most often less than 8 hours (62.4%) (Figure 9).
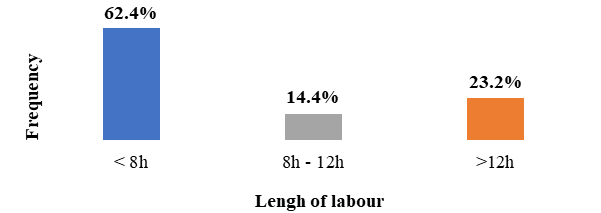
Figure 9 Distribution according to length of labour in patients who received cardiotocograph monitoring at the IHS maternity unit between 1 January 2019 and 31 December 2020 (N=125).
Treatment received: In our series, most patients did not receive any treatment during labour. The administration of oxytocin or antispasmodics was noted in 21.3% and 5.8% of cases respectively (Table 8).
|
Treatment received |
Number |
Frequency (%) |
|
None |
113 |
72,9% |
|
Oxytocin |
33 |
21,3% |
|
Antispasmodic |
9 |
5,8% |
|
Total |
155 |
100% |
Table 8 Distribution according to medication of patients who received cardiotocograph monitoring at the IHS maternity hospital between 1 January 2019 and 31 December 2020 (N=155)
Route of delivery: In our study, more than half the patients (54.8%) had given birth by caesarean section, 42.6% by vaginal delivery and 2.6% with instruments (Figure 4) (Figure 5).
Indications for caesarean section were dominated by non-reassuring fetal status (69.4%), followed by premature rupture of membranes (2.4%) and vascular-renal syndromes (24.7%).
Neonatal prognosis
Condition of the newborn
In our series, almost all newborns (97.4%) were alive. Of these, the majority had an APGAR score greater than 7 at 1 minute (82.7%) and 5 minutes (91.7%) (Figure 10). We also recorded 3 cases of neonatal malformations (1.9%), including a persistent lingual frenulum and a large bursa.
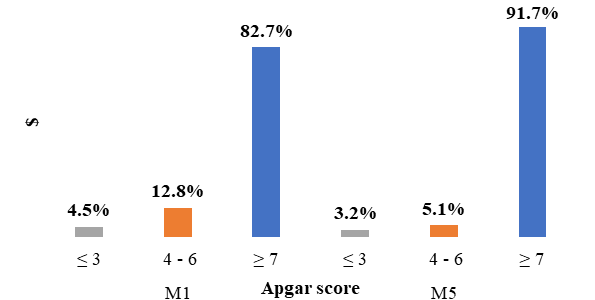
Figure 10 Apgar score distribution of neonates born to mothers who received cardiotocograph monitoring at the IHS maternity unit between 1 January 2019 and 31 December 2020 (N=156).
Transfer to neonatology
In our series, 39 newborns (25%) had been transferred to neonatology. Neonatal distress (41%) and suspected neonatal infection (38.5%) were the main reasons for transfer (Table 9).
|
Reasons for admission to neonatology |
Number |
Fréquency (%) |
|
Neonatal distress |
16 |
41% |
|
Suspicion of neonatal infection |
15 |
38,5% |
|
Prematurity |
10 |
25,6% |
|
Intrauterine growth retardation |
7 |
17,9% |
|
Unspecified |
6 |
15,4% |
Table 9 Distribution according to reasons for admission to neonatology of newborns from patients who received cardiotocograph monitoring at the IHS maternity unit between 1 January 2019 and 31 December 2020 (N=39)
In our series, we recorded 8 neonatal deaths, giving a neonatal mortality rate of 52 per thousand live births.
Analytical results
Performance of fetal heart rate recording in detecting neonatal asphyxia.
Comparison of ERCF results with neonatal status revealed 20 true positives, 7 false negatives, 27 false positives and 102 true negatives. This gives the ERCF a sensitivity of 74.1%, a specificity of 79.1%, a positive predictive value of 42.1% and a negative predictive value of 93.6% (Table 10).
|
|
Neonatal asphixia |
Total |
|
|
Yes |
No |
||
|
NRFS detected by the ERCF |
VP : 20 |
FP : 27 |
47 |
|
NRFS not detected by the ERCF |
FN : 7 |
VN : 102 |
109 |
|
Total |
13 |
143 |
156 |
Table 10 Performance of ERCF in screening for neonatal asphyxia at the IHS maternity hospital between 1 January 2019 and 31 December 2020 (N=156)
TP, true positive; FP, false positive; FN, false negative; TN, true negative; NRFS, non-reassuring fetal status; FHRR, fetal heart rate recording
Performance of doctors specialising in the diagnosis of non-reassuring fetal status on FHRR.
In our series, of the 62 cases (39.7%) of non-reassuring foetal state detected by the doctors in specialisation, 36 (58.1%) were confirmed by the senior doctor and the APGAR score at birth was normal in 22 newborns (35.4%). Also, among the 94 tracings judged normal by the DES, there were 11 cases of FNRFS (11.7%) (Table 11).
|
|
NRFS confirmed by the Sénior |
Total |
|
|
Yes |
No |
||
|
NRFS détected by par the DES |
36 (58,1%) |
26 (41,9%) |
62 |
|
NRFS not detected by the DES |
11 (11,7%) |
83 (88,3%) |
94 |
|
Total |
47 |
109 |
156 |
Table 11 Performance of doctors specialising in the diagnosis of EFNR at the IHS maternity hospital between 1 January 2019 and 31 December 2020 (N=156)
NRFS, non-reassuring foetal state; DES, Doctor's speciality
Cardiotocograph abnormalities and risk of neonatal asphyxia
Basic rhythm abnormalities and risk of neonatal asphyxia
In our series, neonatal asphyxia was noted in 57.9% of cases of bradycardia, whereas this rate was only 38.5% in cases of tachycardia. We also noted 17 cases of neonatal asphyxia (12.6%) when the basic rhythm was normal. There was a statistically significant association between abnormal basal rate and neonatal asphyxia (p = 0.001) (Table 12).
|
Basic rhythm |
Neonatal asphixia |
Total |
|
|
Yes |
No |
||
|
Tachycardia |
5 (38,5%) |
8 (61,5%) |
13 |
|
Bradycardia |
4 (57,9%) |
3 (42,9%) |
7 |
|
Normal |
17 (12,6%) |
118 (87,4%) |
135 |
Table 12 Basic rhythm abnormalities and risk of neonatal asphyxia at the IHS maternity hospital between 1 January 2019 and 31 December 2020 (N=155)
p = 0,001
Variability anomalies and risk of neonatal asphyxia
Neonatal asphyxia was noted in 36.8% of cases of tracings with reduced variability and 30.8% of cases where variability was marked. There was a statistically significant association between variability anomalies and neonatal asphyxia (p = 0.004) (Table 13).
|
Variability |
Neonatal asphixia |
Total |
|
|
Yes |
No |
||
|
Marked (>25 bpm) |
4 (30,8%) |
9 (69,2%) |
13 |
|
Reduced (≤5 bpm) |
7 (36,8%) |
12 (63,2%) |
19 |
|
Normal |
15 (12,2%) |
108 (87,8%) |
123 |
Table 13 Variability anomalies and risk of neonatal asphyxia at the IHS maternity hospital between 1 January 2019 and 31 December 2020 (N=155)
p = 0,004
Accelerations and risk of neonatal asphyxia
Neonatal asphyxia was noted in 20% of cases of acceleration without there being a statistically significant relationship between the existence of accelerations on the FHR trace and the occurrence of neonatal asphyxia (p = 0.458) (Table 14).
|
Accelerations |
Neonatal asphyxia |
Total |
|
|
Yes |
No |
||
|
Present |
10 (20%) |
40 (80%) |
50 |
|
Absent |
15 (14,3%) |
90 (85,7%) |
105 |
Table 14 Acceleration abnormalities and risk of neonatal asphyxia at the IHS maternity hospital between 1 January 2019 and 31 December 2020 (N=155)
p = 0,458
Decelerations and risk of neonatal asphyxia
In our series, neonatal asphyxia was noted in all cases of severe typical variable decelerations, in 57.1% of atypical variable decelerations and 50% of typical variable decelerations. However, there was no statistically significant association between the existence of deceleration and the risk of neonatal asphyxia (p = 0.109).
Uterine contraction abnormalities and risk of neonatal asphyxia
Neonatal asphyxia was noted in only one third (33.3%) of cases of hypertonia and in 20% of cases of hyperkinesia of intensity. There was no statistically significant relationship between uterine contraction abnormalities and the risk of neonatal asphyxia (p = 0.295).
Maternal pathologies and ERCF results
Arterial hypertension and ERCF results
In our series, 48% of women with hypertension had a pathological FCR trace, compared with 26.7% without hypertension. There was a statistically significant association between abnormal FHR and hypertension during pregnancy (p = 0.034) (Table 15).
|
|
RCF patholigical tracing |
Total |
|
|
Yes |
No |
||
|
High blood pressure |
12 (48%) |
13 (52%) |
25 |
|
Normal blood pressure |
35 (26,7%) |
96 (73,3%) |
131 |
Table 15 Hypertension and risk of FCR abnormalities at the IHS maternity hospital between 1 January 2019 and 31 December 2020 (N=156)
p = 0,034
Maternal anaemia and ERCF results
In our series, a pathological FCR trace was noted in 18.2% of anaemic patients. There was no statistically significant association between maternal anaemia and the occurrence of fetal heart rate abnormalities (p = 0.370).
Membrane condition and ERCF results
In our series, FCR abnormalities were more frequent in cases of MTR of more than 6 hours (44.1%) compared with situations where the membranes were intact (26.2%). There was a statistically significant relationship between the condition of the membranes and the occurrence of FHR abnormalities (p = 0.044).
Fetal pathologies and ERCF results
Intrauterine growth retardation and ERCF results
In our series, 80% of fetuses with IUGR had pathological fetal heart rate tracings, whereas this rate was only 28.5% in cases of normal fetal growth. There was a statistically significant association between IUGR and abnormal FHR (p = 0.013) (Table 16).
|
|
RCF pathologigical tracing |
Total |
|
|
Yes |
No |
||
|
IUGR |
4 (80%) |
1 (20%) |
5 |
|
Normal foetal growth |
43 (28,5%) |
108 (71,5%) |
151 |
Table 16 IUGR and ERCF abnormalities at the IHS maternity hospital between 1 January 2019 and 31 December 2020 (N=156)
p = 0,013
Prematurity and ERCF results
In our study, in 42.9% of cases of preterm delivery, the RCF trace was pathological. This rate was 28% for full-term deliveries. However, there was no statistically significant relationship between prematurity and the occurrence of RCF abnormalities (p = 0.172).
Frequency of use of cardiotocography
During the study period, 208 patients were monitored using cardiotocography out of a total of 4123 deliveries, i.e. a frequency of 5%. Variable rates of use are reported in African series. Indeed, in 2013, a study carried out at the Centre de Santé Philippe Maguilen Senghor on the contribution of the ERCF to labour monitoring found a frequency of use of 2.2% of deliveries, lower than that which we recorded.10 However, in Lubumbashi, Mwansa11 reported a higher frequency. Out of 5092 women, 548 had been monitored using a cardiotocograph, a rate of 10.8%. In industrialised countries such as France, labour monitoring is carried out exclusively by cardiotocograph.12
This low frequency of use in our practice could be explained by various reasons, in particular the high cost of the device, which makes it inaccessible to certain health facilities, and the lack of expertise and training of healthcare providers in the use of the cardiotocograph and the interpretation of tracings. However, the Pinard stethoscope, which is used in most maternity units in developing countries, remains effective in monitoring labour and its use is recommended by the WHO in the absence of risk factors for dystocia.
Epidemiological profile
In our study, the epidemiological profile of the patients was that of a woman aged 28 years on average, of low socio-economic status (83.2%), primiparous (45.2%) or pauciparous (46.5%), carrying a full-term pregnancy (67.7%) and living outside the South district (72.3%). This profile does not differ from those reported in the literature. Indeed, Mbaye10 at the Philippe Senghor Health Centre found an average age of 27 years and a predominance of primiparous women (67.2%). In India, the same finding was made in the study by Kumar,13 where the 21 to 25 age group was the most represented and primiparous women were in the majority (61.1%). He also reported a higher proportion of full-term pregnancies, which could be explained by the fact that the cardiotocograph is often used to monitor labour.
Results of fetal heart rate recording
Among the pathological FHR tracings, we recorded 12.8% abnormalities of the basic rhythm, 21.1% abnormalities of variability and 31.3% decelerations. Basic rhythm abnormalities were dominated by tachycardia (7.7%) followed by bradycardia (4.5%). Mbaye10 reported a higher proportion of bradycardia (11.8%). However, his rate of tachycardia was lower than ours, estimated at 6.4% of FHR abnormalities. When bradycardia is persistent and severe, or when it is associated with a lack of variability, it is considered to be at high risk of foetal acidosis [80]. This is confirmed by our results. In our study, bradycardia was associated with 57.9% of neonatal asphyxia (p =0.001). On the other hand, moderate and isolated tachycardia is not associated with an unfavourable neonatal outcome except in cases of maternal infection.14
In our series, variability was most often reduced (12.2%) or marked (8.3%) in cases of anomalies. In his study, Mbaye10 reported a much higher proportion of reduced variability (49.1%). Reduced variability, when associated with late decelerations, may indicate foetal asphyxia or neonatal encephalopathy.15 On the other hand, when it is isolated, it is not necessarily pejorative. This could explain the fact that most of the fetuses with reduced variability in our series (63.2%) had a normal APGAR score at 1 minute.
In our series, variable, early, late and prolonged decelerations represented respectively 6.4%, 16%, 7.1% and 1.8% of all FHR anomalies. In Mbaye's study, variable decelerations were more frequent than in ours. They accounted for 11.8% of patients. However, their proportions of early (1.8%) and late (2.7%) decelerations were lower than ours. A variable deceleration pattern can lead to acidosis and fetal distress.16 This is confirmed by our results, as neonatal asphyxia was found in all cases of severe typical variable deceleration, 57.1% of atypical variable deceleration and 50% of typical variable deceleration. On the other hand, early decelerations do not reflect a non-reassuring foetal state in our study (p=0.418) and are rather related to uterine contraction. As for late decelerations, several studies have reported their association with a low Apgar score at the 1st and/or 5th minute.17,18 Prolonged decelerations were not associated with a low Apgar score in our study (p=0.180). Apart from certain specific situations such as retro placental haematoma and hyperkinesias, prolonged deceleration is not a pejorative sign, especially if it is sporadic, isolated, without any other abnormality of the FHR and if the return to the previous normal rhythm is rapid.19
The results of the tracings were interpreted according to the 2007 CNGOF classification. In our series, 37.8% of the tracings were normal and we recorded 32.1% intermediate anomalies and 30.1% pathological tracings. In the Lubumbashi study by Mwansa,11 61.3% of tracings were normal and 19.9% pathological. In India, a study of cardiotocograph screening for FCR abnormalities on admission found 69.4% normal FCR tracings, 22.2% intermediate tracings and 8.4% pathological tracings.13 The low percentage of normal traces that we recorded compared with the literature could be explained by the fact that in most studies parturients were monitored systematically by the cardiotocograph, whereas in our series the cardiotocograph was reserved for high-risk situations.
Performance of fetal heart rate recording in detecting non-reassuring fetal status.
In our study we found that the cardiotocograph had a sensitivity of 74.1%, a specificity of 79.1%, a positive predictive value of 42.6% and a negative predictive value of 93.6%. These figures are almost similar to those reported by Mwansa11 in 2018 in Lubumbashi with a sensitivity of 82.98%, a specificity of 83.85%, a positive predictive value of 45.35% and a negative predictive value of 96.83%. Tournemire20 in 2014 found that using the 2007 CNGOF classification, the sensitivity and specificity of ERCF for predicting fetal acidosis were 88.8% and 46.9% respectively. In 2015, Ana and Edwin21 confirmed this low positive predictive value of cardiotocography in intrapartum assessment of the risk of fetal hypoxia, estimating it at 30% in their study.
This low positive predictive value of cardiotocography found in most studies could explain the high caesarean section rates most often performed for a non-reassuring foetal condition in parturients monitored by the cardiotocograph. This is one of the disadvantages of continuous labour monitoring by cardiotocograph. Isolated or sporadic FHR abnormalities should be correlated with the clinical situation for better interpretation. In 2007, the CNGOF22 recommended the use of second-line techniques for a more detailed analysis of FHR anomalies.
Performance of doctors specialising in the diagnosis of EFNR Maternal pathologies and RCF anomalies.
The diagnosis of EFNR on the ERCF made in 62 patients by the specialist doctors was confirmed retrospectively in only 36 of them by the senior doctor. The APGAR score at birth was normal in 22 newborns (35.4%). According to FIGO, it has been well demonstrated that cardiotocographic trace analysis is subject to considerable intra- and inter-observer disagreement, even when experienced clinicians use widely accepted guidelines.23,24
Route of delivery
In our series, 54.8% of women monitored by cardiotocograph delivered by caesarean section, whereas the overall caesarean section rate in the department was 44.6% in 2020. According to a NICE report,14 the increase in the caesarean section rate in England and Wales from 9% in 1980 to 21% in 2001 is partly linked to abnormal FHR patterns, which accounted for 22% of caesarean section indications. Alfirevic,9 in a Cochrane review published in 2013 and updated in 2017, concluded that CTG during labour is associated with a reduced rate of neonatal seizures, but no clear difference in cerebral palsy and infant mortality. However, continuous CTG was associated with a 63% increase in caesarean sections and a 15% increase in instrumental vaginal deliveries.
Maternal pathologies and FCR abnormalities
In our study, the maternal pathologies associated with FCR abnormalities were arterial hypertension (p=0.034) and premature rupture of membranes (p=0.044). In Lubumbashi, the factors associated with pathological FHR abnormalities were prolonged labour, chorioamniotitis, chronic maternal anaemia, primiparity, prematurity and prolonged pregnancy. Mwansa11 states that hypertension increased the risk of late decelerations by 2.74 times. In fact, pre-eclampsia causes a disturbance in foetal-maternal exchanges, with a risk of IUGR and foetal heart rhythm abnormalities.25 In 2020, Peru26 found more foetal heart rate abnormalities (44.6%) after premature rupture of the membranes. Several mechanisms could be responsible, in particular compression phenomena and chorioamniotitis.
Fetal pathologies and FHR anomalies
In our study, the only foetal pathology associated with cardiac rhythm disorders was intrauterine growth retardation (p=0.013). Fetal heart rate abnormalities during labour are more common in IUGR.27 When associated with FHR abnormalities, IUGR is often of vascular origin. This accounts for 30% of the causes of IUGR. It is characterised by a reduction in uteroplacental flow, which disrupts maternal-foetal exchanges, leading to foetal hypoxia and EFNR during labour. IUGR can also be caused by other factors. These include foetal anomalies (chromosomal, genetic, congenital, malformative), infectious, nutritional, toxic, placental, uterine causes, multiple pregnancies and low socio-economic status.28
The availability of cardiotocographs and ongoing training of healthcare staff in the interpretation of tracings, while taking account of the clinical situation in the interpretation of tracings, would make it possible to improve neonatal and maternal prognosis. However, its systematic use in labour monitoring would be associated with an increase in the caesarean section rate.
None.
None.
All authors declare that they have no conflict of interests.

©2023 Samb, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.