eISSN: 2377-4304


Research Article Volume 5 Issue 5
1Department of Obstetrics and Gynecology, Menoufia University, Egypt
2Department of General Surgery, Menoufia University, Egypt
3Department of Radiology, Menoufia University, Egypt
4Department of Pediatrics, Menoufia University, Egypt
Correspondence: Alaa Masood, Department of Obstetrics and Gynecology, Faculty of Medicine, Menoufia University, Egypt, Tel 00201006237186
Received: July 20, 2016 | Published: November 30, 2016
Citation: Masood A, Saleh S, Shaheen A, et al. Maternal and fetal outcome in pregnant women with acute appendicitis: a three year observational study. Obstet Gynecol Int J. 2016;5(5):400-403. DOI: 10.15406/ogij.2016.05.00173
Objective: To assess the maternal and fetal outcome in pregnant women presented with acute appendicitis and to detect predictors of fetal loss.
Methods: A prospective observational study included 118 pregnant women presented with acute appendicitis and divided into two groups, uncomplicated appendicitis group (n=64) and complicated appendicitis group (n=54). Operative details, maternal and fetal outcome were assessed. Univariate and multivariate analyses were used to detect predictors of fetal loss. Data was collected and tabulated.
Results: Patients in the complicated group have gone midline incision, longer operative time, more postoperative fever, more surgical site infection, longer hospital stay (p<0.001), higher rate of abortion and fetal demise (p<0.05) than uncomplicated appendicitis patients.
Conclusion: Poorer obstetric outcome was encountered in complicated cases. In addition to complicated appendicitis, the use of general anesthesia, operative time greater than 60 minutes, midline incision, postoperative pneumonia and hospital stay more than 3 days were other predictors of fetal loss. Larger studies are warranted to confirm or refute our findings.
Keywords: Acute appendicitis, Pregnancy complications
Appendicitis is one of the most common conditions requiring laparotomy during pregnancy (about 40%) for a non-obstetric disease and is known to occur once in every 1,500 pregnant women.1,2 Immediate diagnosis and surgery are recommended, since surgical intervention delayed for more than 24 hours after onset of symptoms increases the risk of perforation with subsequent increase in maternal morbidity and pregnancy loss.3,4 A ruptured appendix is more common in pregnant women, especially in the third trimester, possibly due to these difficulties and the reluctance to operate on pregnant women, which ultimately delays diagnosis and treatment.5 The aim of this study was to assess the maternal and fetal outcome in pregnant women presented with acute appendicitis (uncomplicated and complicated), and to detect predictors of fetal loss.
This was a prospective observational study carried out at the department of Obstetrics and Gynecology in collaboration with Radiology, General Surgery and Pediatric departments at Menoufia University Hospital, Menoufia, Egypt in the period between June 2013 and June 2016. The Medical Ethics Committee for Human Research at Menoufia Faculty of Medicine approved the study protocol and an informed consent was obtained from all participants prior to commencing the study. The assumed total sample size of the study was actually calculated according to a proposed type I error of 5% with an expected difference between rates of fetal loss between the study groups of 10%. Type II error was proposed to be 20% (β = 20%) hence the power was set at (1-β, 80%). Accordingly, 60 pregnant women were needed in each group after adding a 10% for possible drop out of cases.
Pregnant women diagnosed with acute appendicitis after thorough history taking, clinical examination, laboratory testing and ultrasound examination were included. Clinical criteria included acute abdominal pain started as diffuse then settled in the right iliac fossa, anorexia, nausea, vomiting, constipation, low-grade fever, tenderness in the right iliac fossa and rebound tenderness.6 Total leucocytic count (TLC) above 16,000/mm³. Ultrasound was performed at Radiology department by MyLab60 machine (Italy) using high frequency linear transducer by graded compression technique. Ultrasound criteria included the identification of a non-compressible, blind-ended tubular structure in the lower right quadrant, with a maximum diameter exceeding 6 mm, round configuration in the transverse section (Target sign) (Figure 1), alteration of the peri-appendiceal fat in the form of increased echogenicity, localized peri-appendicular fluid collection and hypervascularisation of the appendix in color Doppler study (Figure 2).7,8
Complicated appendicitis was diagnosed in patients with appendicular mass or abscess, appendicular perforation or with signs of peritonitis (Figure 3). Ultrasound examination can also exclude other possible causes of abdominal pain (e.g. ovarian cyst torsion, degeneration or torsion of myoma, nephrolithiasis and cholecystitis). 134 Pregnant women presented to the emergency room in the Emergeny department by acute appendicitis, 16 patients were dropped out (lost to follow up). So, 118 patients completed the study (Figure 4).
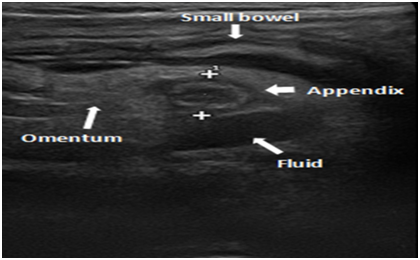
Figure 3 Appendicular inflammatory mass : appendix , small bowel loop, free intraperitoneal fluid and omentum.
Patients were divided pre-operatively into two groups for comparison:
Group 1 (uncomplicated appendicitis): Included 64 patients who underwent appendectomy through Mc Burney's incision.
Group 2 (complicated appendicitis): Included 54 patients who underwent either Mc Burney's incision exploratory laparotomy via lower midline incision with thorough washing and drainage of the peritoneal cavity after appendectomy.
Patients underwent appendectomy at the General Surgery department within 2-5 hours from arrival to Emergency department, with a standard protocol of antibiotics, tocolytics and antenatal corticosteroids as indicated. Antibiotics in the form of Ampicillin 1 gm every 6 hours for 48 hours followed by Amoxycilline 500 mg every 6 hours orally daily for 10 days with addition of Metronidazole 1 gm rectal suppositories every 12 hours for 5 days in complicated cases. Tocolytic therapy in the form of rectal Indomethacin 100 mg every 12 hours for 48 hours in pregnancy before 30 weeks gestation and oral Nifedipine 20 mg orally initially followed by 10 mg every 8 hours for 48 hours in pregnancy after 30 weeks. Dexamethazone 6 mg every 12 hours for 4 doses in pregnant patients after 24 weeks gestation. All included women underwent regular antenatal visits every 1-3 weeks till delivery to record their obstetric outcome.
Outcome measures
Maternal outcome: operative details (including type of anesthesia, type of incision, operative time and postoperative complications as fever, wound infection, re-exploration, thromboembolism and length of hospital stay), abortion, preterm delivery (defined as delivery before completed 37 weeks), placental abruption and mode of delivery.
Fetal outcome: fetal demise, prematurity and admission to neonatal intensive care unit (NICU) and neonatal death (defined as death during the first 28 days after birth). Predictors of fetal loss were also assessed.
Statistical analysis
Statistical analysis was performed using Statistical Package for the Social Sciences Version 16 (IBM Corp., Armonk, NY, USA). Quantitative data are expressed as means and standard deviations. Chi-squared test and t-test were used to compare the two groups. Logistic regression was used to assess the crude association between the risk of pregnancy loss and operative details. Covariates exhibiting an association with pregnancy loss (p<0.05) were included when developing univariate and multivariate logistic regression analyses. p≤ 0.05 was considered to indicate significance and p≤ 0.001 was considered to indicate strong significance.
Table 1 reveals the maternal characteristics. There was no significant difference between the two groups regarding the age, parity, body mass index and pregnancy trimester on presentation (p>0.05). Table 2 shows the operative and postoperative details. There was a highly significant difference between the two groups regarding type of incision, operative time, postoperative fever, surgical site infection and length of hospital stay (p<0.001), with more patients underwent midline incision, longer operative time, more postoperative fever, more surgical site infection and longer hospital stay in complicated appendicitis group.
|
Uncomplicated |
Complicated |
Student |
P-value |
|
|
Age (in years) |
28.4±5.18 |
28.5±5.56 |
0.13 |
>0.05 |
|
Parity |
1.12±1.03 |
1.09±1.13 |
0.2* |
>0.05 |
|
Body Mass Index |
24.86±1.94 |
24.9±1.9 |
0.18 |
>0.05 |
|
Gestational age |
|
|
|
|
|
First Trimester |
25 |
22 |
1.4† |
>0.05 |
|
Second Trimester |
28 |
24 |
||
|
Third Trimester |
11 |
8 |
Table 1: Maternal characteristics
*Mann Whitney test, †Chi-square test.
|
Uncomplicated appendicitis (n=64) |
Complicated appendicitis (n=54) |
Chi-square test |
P-value |
|
|
Type of anesthesia |
||||
|
General |
28(43.75%) |
24(44.44%) |
0.9 |
>0.05 |
|
Spinal |
36(56.25%) |
30(55.56%) |
||
|
Type of incision |
||||
|
Mc Burney |
62(96.8%) |
5(9.25%) |
28.8 |
<0.001 |
|
Midline |
2(3.2%) |
49(90.75%) |
||
|
Operative Time |
Range (30-72) |
Range (55-132) |
9.35* |
<0.001 |
|
Postoperative Fever |
11(17.2%) |
37(68.5%) |
13.5 |
<0.001 |
|
Surgical site Infection |
8(12.5%) |
26(48.1%) |
9.9 |
<0.05 |
|
Thromboembolism |
0 |
0 |
- |
- |
|
Re-Exploration |
0 |
0 |
- |
- |
|
Hospital Stay (days) |
1.2±1.4 |
4.6±2.5 |
9.29* |
<0.001 |
Table 2 Operative and postoperative data
*Student t-test
Table 3 reveals maternal and fetal outcome. There was a higher rate of abortion and fetal demise in complicated appendicitis group (p<0.05). Table 4 show predictors of fetal loss in the two groups collectively by univariate and multivariate analyses. In addition to complicated appendicitis, the use of general anesthesia, operative time greater than 60 minutes, midline incision, postoperative pneumonia and hospital stay more than 3 days were strong predictors of fetal loss (p<0.05).
|
Uncomplicated appendicitis (n=64) |
Complicated appendicitis (n=54) |
Chi-square test |
P-value |
OR (CI 95%) |
|
|
Abortion |
4(6.25%) |
12(22.2%) |
4.82 |
<0.05 |
15.9 (1.67-30.23) |
|
Preterm delivery |
5(7.8%) |
5(9.25%) |
0.07 |
>0.05 |
12.7 (10.4-13.3) |
|
Placental abruption |
2(3.1%) |
3(5.5%) |
0.39 |
>0.05 |
8.7 (6.7-11.5) |
|
Mode of delivery |
|||||
|
Vaginal delivery |
48(75%) |
28(51.8%) |
1.51 |
>0.05 |
23.2 (4.46-41.9) |
|
Cesarean delivery |
16(25%) |
26(48.2%) |
|||
|
Fetal demise |
5(7.8%) |
13(24.1%) |
4.37 |
<0.05 |
16.3(1.43-31.17) |
|
NICU admission |
5(7.8%) |
5(9.25%) |
0.07 |
>0.05 |
12.7 (10.4-13.3) |
|
Neonatal death |
1(1.56%) |
2(3.7%) |
0.51 |
>0.05 |
7.5 (5.3-9.7) |
Table 3 Maternal and fetal outcome
|
Risk Factor |
Crude Odd’s ratio |
Upper and Lower limit |
|
Complicated appendicitis |
0.68 |
0.58– 0.80 |
|
Use of general anesthesia |
0.74 |
0.63– 0.86 |
|
Operative time (>60 minutes) |
1.25 |
1.02– 1.54 |
|
Midline laparotomy |
1.57 |
1.32– 1.86 |
|
Postoperative pneumonia |
0.73 |
0.64 – 0.84 |
|
Hospital stay (>3 days) |
1.29 |
1.09– 1.53 |
Table 4 Predictors of fetal loss in the two groups collectively by univariate and multivariate analyses
Complicated appendicitis was encountered in 45.7% (54/118) of pregnant patients attending the Emergency department at our hospital with acute appendicitis. The incidence rate of perforated appendicitis during pregnancy was 43% and that rate was associated with the time from the onset of symptoms to surgery. The risk of developing perforation is high when the time from the onset of symptoms to surgery exceeds 20 hours.9 In our study, only 16.1% (19/118) of patients were in the third trimester of pregnancy. The lowest risk of acute appendicitis during pregnancy was reported during the third trimester.10
In this study, more patients underwent midline incision, longer operative time, more postoperative fever, more surgical site infection and longer hospital stay in complicated appendicitis group. In pregnancy, there was an almost two-fold increase in sepsis and septic shock, transfusion, pneumonia, bowel obstruction, postoperative infection and length of stay >3 days when compared to non-pregnant women.11
In this series, there was a higher rate of abortion and fetal demise in complicated appendicitis in comparison to uncomplicated cases (22.2% vs 6.25% and 24.1% vs 7.8% respectively). Although the rate of preterm delivery and cesarean section was higher in complicated appendicitis, it does not reach to a significant difference (9.25 vs 7.8% and 48.2 % vs 25% respectively). The risk of fetal loss is increased when the appendix perforates (fetal loss 36 versus 1.5% without perforation) or when there is a generalized peritonitis or abscess (fetal loss 6 versus 2%, premature delivery 11 versus 4%).12
Pregnant women with appendicitis were more likely to deliver preterm OR 2.68 (95 % CI 2.31-3.11) and had an increased risk in abruption placentae. Among the 27 % of patients with peritonitis, the rate of preterm birth was fourfold higher, and the caesarean section rate was almost doubled.13 Also, the increase in preterm labour is affected by increases in perforation and gestational age.9 The fetal death rate in non complicated appendicitis has been reported at 1.5 to 4%, but in cases of perforated appendicitis, the rate is still high at 21 to 35%.14 In our study, open appendectomy was preferred to laparoscopic approach since it is associated with a lower rate of fetal loss as evidenced in previous two systematic reviews and meta-analysis.15,16 Our study was conducted to detect predictors of fetal loss other than complicated appendicitis, the use of general anesthesia, operative time greater than 60 minutes; midline incision, postoperative pneumonia and hospital stay more than 3 days were found to be strong predictors of fetal loss. Future research should explore predictors of fetal loss in a larger number of patients with uncomplicated appendicitis to confirm or refute our findings.
None.
None.

©2016 Masood, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.