eISSN: 2377-4304


Case Report Volume 13 Issue 2
1Affiliated Physician, Naval Medical Center, Mexico City, 04480, México
2Affiliated Physician, Naval Hospital Chetumal, México
3Affiliated Physician, ABC Hospital, Observatory, Mexico
4Affiliated Physician, ABC Hospital Santa Fe, México
5Affiliated Physician, Militar Medical School, México
6Resident of gynecology and obstetrics, Department of, Naval Medical Center, México
Correspondence: Yanet fermin Aldama, telephone number: 9621525285, Mexico City, Coyoacán delegation, zip code 04480, Tel +52 9621525285
Received: February 28, 2022 | Published: March 16, 2022
Citation: DOI: 10.15406/ogij.2022.13.00632
Sarcomas of the uterus are a group of tumors that make up 1% of neoplasms of the female genital tract.1 The global incidence is 0.5 to 3.3 cases per 100,000 women per year 1 the rarity of this tumor, and its histological diversity, contributes to the lack of consensus on diagnostic behavior and timely treatment.1 The incidence increases in ages over 40years, tied to other risk factors.1 The preoperative diagnosis is a challenge, since the clinical presentation is variable, it frequently presents with transvaginal bleeding and a rapid increase in the size of the uterus,2 accompanied by symptoms of pelvic pressure, anemic syndrome stands out in these women in different degrees.2 however there are high frequency pathologies that share clinical characteristics that direct the diagnosis and is easily confused with benign leiomyoma and adenomyosis3 The objective of this presentation of the case is to take into account as a differential diagnosis in abnormal uterine bleeding and constitutional syndrome,2 due to the rarity of this tumor, only some articles of review and report of cases have been published.3
Keywords: pelvic mass, sarcoma, abnormal uterine bleeding, leiomyosarcoma, abnormal uterine bleeding
The new staging of the International Federation of Gynecology and Obstetrics3 highlights the importance of the diagnosis affects the taking of decisions for the surgical event, in patients with early stages, the complete surgical resection of the tumor with negative margins as primary therapy.3
Given the possibility of the risk of malignancy within abnormal uterine bleeding, imaging studies should be performed that offer the ability to prospectively differentiate benign leiomyomas from leiomyosarcomas, which would ensure that patients receive the appropriate treatment in the first place, which would reduce the risk of overshadowing the disease and negatively affecting prognosis.4 Pretreatment imaging of leiomyomas can be performed with multiple modalities, all of which have limitations with respect to achieving an unsuspected definitive prospective diagnosis.3 Ultrasound is often the first imaging test used for a woman with suspected symptomatic benign leiomyomas.5 Although ultrasonography is helpful and widely available, the patient's body build, operator experience, or both can make a uterine evaluation difficult. complete. Ultrasound also has limitations especially in the evaluation of an enlarged uterus with multiple leiomyomas that may be located beyond the focal zone of the transducer, similarly, ultrasound evaluation may be limited for retroverted uteri and concomitant adnexal processes. Although CT is the primary modality for staging cancers, it does not offer adequate contrast resolution for delineating focal myometrial masses and also carries risks associated with ionizing radiation.4 In addition, CT is inferior to MRI for delineating Reliably, zonal anatomy for precise localization of leiomyomas is a promising modality for confirmation of malignancy, as well as for detecting metastases and recurrence.5
A 46-year-old patient who goes to the emergency room to tocosurgery for presenting abundant transvaginal bleeding of 2 days of evolution, as a history of importance previously she had with anemic syndrome that is conditioned by abundant transvaginal bleeding, with hereditary history of importance, in maternal line: lymphoma, and stomach cancer, has a surgical history consisting of Cesarean section plus bilateral tubal occlusion.
Background Gyneco-Obstetrics: menarche 12 years, cycles of 30 days x 4 days of duration, onset of active sexual life 19 years, gestation 1, Cesarean section 1 plus bilateral tubal occlusion, A targeted examination in the abdomen palpates pelvic mass of approximately 8 cm above the symphysis of the pubis, genital examination; to spectroscopy with abundant transvaginal bleeding, active.
She is admitted for diagnostic protocol and surgical programming: she has cervical cytology reports: 11-22-2021: negative for malignancy, 2020 mammography without alterations. Endometrial biopsy: 11.22.2021: inadequate sample for diagnosis due to hemorrhage, few focal fragments and endometrial fragments.
Admission laboratories highlight the blood count with leukocytes: 8000, hemoglobin 8g/l, hematocrit: 24%, platelets 250,000,000, rest of laboratories without alterations, ultrasonography 11.28.2021 tumor in pelvic cavity dependent on uterine body of 14 is reported cm, heterogeneous, with fine echoes inside, without data of vascular alterations, endometrium not visible, ovaries not visible (Image 1).
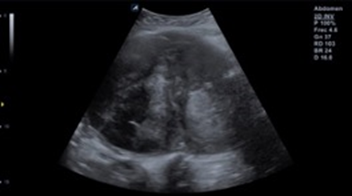
Image 1 Pelvic ultrasound. The anatomical topography of the uterus shows the presence of an oval image with lobulated edges and heterogeneous echogenicity due to solid areas with a cystic appearance (white arrow), which shows partial flow saturation after applying the color Doppler modality.
Magnetic resonance imaging 11.30.2021 uterus with loss of morphology, with the presence of an intramural fibroid of 16x11x16 cm, with areas of hyaline degeneration (Image 2) (Image 3).
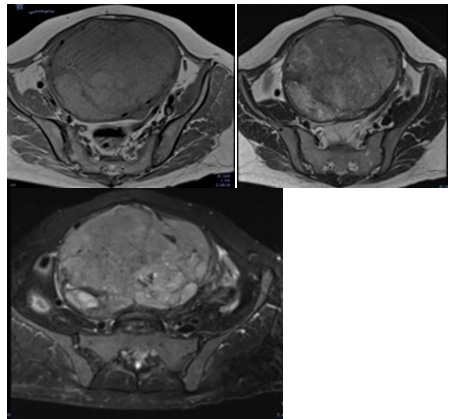
Image 3 MRI of the simple pelvis. It is observed in axial plane sequence T1, image dependent on uterus iso intense to the muscle and with areas of solid appearance and some of cystic appearance in T2 (Image 4) and incipient areas of fat content (white arrow) in SEQUENCE FAT SAT (Image 5).
Surgical programming is performed and a total abdominal hysterectomy is performed, the procedure is completed without complications, with a bleeding of 500ml.
During her postoperative period, course with satisfactory evolution, 3 erythrocyte concentrates and 1 plasma were transfused, after 48 hours a histopathological report is reported with the report of spindle cell variant uterine leiomyosarcoma with tumor site anterior uterine wall and fundus. Figure 1, Figure 2 It is concluded with gynecological oncology in uterine sarcoma EC IB with probable metastasis.
Sarcomas account for 3-5%, leioiosarcoma being the second most frequent group among these,1 considering that the clinical stage is the most important prognostic factor, for which special attention should be paid in the clinic and the systematic form in the that uterine bleeding is addressed, since the clinical, analytical and imaging studies are not characteristic;4 However, pelvic ultrasound, magnetic resonance imaging and tomography provide important data that incline us towards diagnostic suspicion,4 the most characteristic symptom in our patient is uterine growth, in this case due to the rapid progression of the disease and the clinical context of the patient, surgical treatment was the first choice, consisting of total abdominal hysterectomy. The form of clinical presentation is varied, its origin can be associated with a uterine fibroid, although in most cases it arises independently of the benign neoplasm,2 and between the two the difference is the number of mitosis.4 Because there is no specific screening for uterine sarcoma, clinical, ultrasound factors must be taken into account to expand the diagnostic study.4
There is no effective preoperative screening, however, according to risk factors and suspected diagnosis, a pelvic magnetic resonance should be requested, as well as a postoperative study. In order to effectively stage and achieve neoadjuvant treatment.4
Ultrasound is usually the first-line imaging study performed in the study of pelvic masses; however, this modality is limited in its evaluation of an enlarged uterus and soft tissue characterization,5 in contrast, MRI can offer a comprehensive map of the uterus and the size, location, and distribution of focal uterine masses, and allows a greater characterization of these masses, however primarily for the evaluation of abnormal uterine bleeding and pelvic mass ultrasound as the first choice according to clinical practice guidelines,5 they are still effective and should be thoroughly evaluated using MRI for evaluation comprehensively.5
None.
None.
Any conflict of interest exists.

©2022 , et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.