eISSN: 2377-4304


Review Article Volume 2 Issue 4
Birthing Instincts, USA
Correspondence: Stuart J Fischbein, Birthing Instincts, 10309 Santa Monica Blvd. Suite 300. Los Angeles. CA 90025, USA, Tel (310) 892-5151
Received: January 08, 2015 | Published: July 7, 2015
Citation: Fischbein SJ. “Home birth” with an obstetrician: a series of 135 out of hospital births. Obstet Gynecol Int J. 2015;2(4):132-136. DOI: 10.15406/ogij.2015.02.00046
Objective: To evaluate the outcomes of properly selected women in an out-of-hospital birth setting with an obstetrician’s unique skills using a midwifery model of care.
Design: This is a retrospective review of 135 consecutive out of hospital deliveries over a 56 month period from 2010-2015.
Setting: All births took place either in the client’s home or a midwife owned free-standing birth center.
Population or sample: Women were considered candidates if they had no major medical issues, remained healthy and compliant during the prenatal period, went to term and maintained an appropriate maternal positive mindset.
Methods: The births include singleton, VBAC, breech and twin deliveries.
Main outcome measures: The outcomes of the 135 births are presented in a straight statistical format for comparative analysis with current trends in the hospital birth model.
Results: There were 135 women who gave birth to 147 live born infants. 89.6% of the mothers gave birth at home/birth center. The cesarean section rate was 5.9%. There were 96 singleton cephalic births, 27 singleton breech births and 12 sets of twins. There were 32 trials of labor after cesarean (TOLAC) of which 30 were successful vaginal births after cesarean (VBAC) (93.8%). 22 of 27 (81.5%) of the singleton breech babies delivered vaginally. While 11 of 12 (91.7%) of the twin pregnancies delivered at home.
Conclusion: Birth at home for properly selected women with a skilled practitioner is a reasonable and ethical option.
Keywords: homebirth, breech, VBAC, informed consent, twins
The current standard of obstetrical practice in the United States is hospital based and leans heavily on medical and surgical intervention.1-3 In 1970 the United States cesarean section rate was 5.5%. By 1990 it had reached 22.7% and currently almost 1/3 of women are having their babies via major abdominal surgery. There has been little corresponding benefit to this 5-fold increase and, in fact, much data has become available to suggest a rising detriment to both mother and baby from such a high surgical birth rate.4-6 The persistent use of continuous fetal monitoring despite lack of evidence supporting its benefit7 and continued adherence to the Friedman curve in spite of knowledge that it is flawed science8 have not served women well yet they remain standard in most hospital obstetrical units.9
In the early 1980’s breech, VBAC, twin and forceps vaginal deliveries were the standard. Hands on skills were emphasized and the system at that time allowed resident to teach intern to teach medical student. Currently, pregnancy and birth as illness continues to be taught in the medical model with little emphasis on these skills and almost none towards an understanding that normal birth is wellness and does not always need treatment.10
Out of hospital birthing of properly selected women with a qualified midwife has been generally accepted worldwide for generations. Obstetricians have been reluctant to support or enter into this realm. This paper is an observational report on the first 135 out of hospital births attended by a single obstetrician. Some were clients cared for through most of their pregnancy and had prenatal appointments with the same frequency and testing offered in the traditional obstetrical practice. Many signed on in the last weeks when they discovered their options were limited in a conventional hospital practice and a few were those met for the first time when called in labor by a midwife to assist at their birth.
This paper describes a retrospective analysis of a clinical series of 157 consecutive pregnant women who entered into care with a single private practitioner. Of these, 135 went into labor with the intent on delivering outside of the standard American hospital setting. Twenty two developed clinical problems prior to labor requiring transfer of care to a conventional obstetrician/hospital based practice. Most clients self-selected the option of home birthing with an obstetrician while some were referred for conditions outside the scope of a midwife practice or lack of options in a traditional hospital based obstetric practice. Ten came into care while already in labor when physician assistance was requested thus skewing up the number of operative vaginal births and episiotomies.
The women in this series were all in good health prior to entry into care. They received prenatal and labor care using the midwifery model. This model offers the same frequency of prenatal visits and options for testing as the common obstetric model. The difference lies in the approach to care and the concept that pregnancy and birth are wellness, not illness. All clients desiring care with the obstetrician went through an initial 60-90 minute consultation. At this meeting their history was reviewed, specific questions were answered and evidenced based literature referenced before an agreement for care was reached. Prenatal visits lasted 45-60 minutes allowing for preventative care that encouraged a healthy lifestyle, stress reduction and nutrition. In most cases the prenatal care, labor support and delivery were solely with the author or a designated team consisting of the author, a midwife and a midwifery student. This allowed for a relationship to develop that instilled confidence in both parties. Family members were encouraged to participate. Informed decision making was respected. At 36-37 weeks a home prenatal visit was performed which included the usual prenatal assessments as well as a discussion of expectations, back-up plan and home preparation.
Criteria for selection was dependent on the basic premises of good health and compliance but was individualized based on client history and allowed for some flexibility. This model was not limited by strict protocols and allowed for guidelines to be merely guidelines. Women over 35, VBAC, breech and twin pregnancies were not excluded from this series simply because those labels existed. Each client was evaluated on her own merits and the comfort of the practitioner. Selection of candidates for breech and twin delivery was based on well recognized guidelines.11
For term breech vaginal delivery this included 8 basic criteria:
Candidates for twin delivery were required to be beyond 36 weeks, concordant, with EFW beyond 2250 grams with tolerance to spontaneous labor. Twin A was required to have a stable longitudinal lie. Intermittent fetal monitoring was used in all births and portable ultrasound was available in all twin deliveries.
While the mammalian model prefers home birthing where the mother never has to leave her surroundings it is understood that this setting is not ideal for all families. However, the equipment for a home or birthing center birth is the same. Birth kits and some supplies were ordered online by the family while most of the birth supplies and equipment were brought by the birth team. These include, but are not limited to, a portable birthing tub and liner, IV fluids and tubing, sterile gloves, gauze, pads, betadine, suture material and instruments. Medications include antibiotics, lidocaine, pitocin, misoprostol, vitamin K, oxygen and some herbal remedies. In this series a portable ultrasound machine was available for all twin deliveries and the physician carried a mity-vac vacuum, Piper forceps, Simpson forceps and Tucker-McLean forceps. In all 135 births the women were encouraged to drink and take nourishment. They were free to ambulate and in most cases to choose the position and location for delivery.
In an ideal midwifery model it is preferred to have early entry into care so that the advantages of this model can be fully appreciated. However, due to unique situations, near term women desirous of reasonable yet limited options were accepted as clients late in their pregnancy. Women were accepted at all gestational ages. There was no selection bias to embellish results. The data was not analyzed prior to completion of the 135th birth.
There were 135 healthy women included in this series who delivered a total of 147 live born infants over a period of 56 months. The author attended all the out of hospital births. A total of 157 women began prenatal care, however 22 developed obstetrical complications prior to labor necessitating transfer of care (TOC). None of the women developed gestational diabetes. One developed preeclampsia. Maternal age range was from 23 to 44 years of age with the average age being 33.3. No abnormalities or increased risks were seen in women >35 years of age (Table 1).
The average pre-pregnancy weight was 148 lbs. with 19 women having a BMI greater than 30. Average weight gain was 36.9 pounds. Average gestational age of all delivered clients was 40 weeks (range 36-43.5 weeks). Of the 51 spontaneous vaginal births (non-breech, twin, VBAC or operative vaginal) 58.8 % (n=30) were multiparous and 41.2% (n=21) were primiparous. Additionally, a vacuum extractor was used 15 times and Simpson forceps were applied twice. All operative vaginal births were successful.
There were 33 total breech deliveries. 27 were singleton. 23 of the 27 (85.2%) were primiparous and all were either complete or frank. A total of 4/33 (12.1%) were assisted by Piper forceps. Of all breech babies in this series, 84.8% (n=28) delivered successfully while 15.2% (n=5), all singleton functional primiparas, were transported non-emergently for arrest and underwent cesarean section as their only hospital option.
There were 12 sets of twins in the series with 91.7% (n=11) delivering vaginally at home. Of these 11, 6 were vertex/vertex, 4 were vertex/breech and one was breech/breech12,13 (Table 2 & 3).
Moments for age |
|
N |
119 |
Mean |
34 |
Std. Deviation |
4.3 |
Variance |
18.9 |
Minimum |
23 |
Maximum |
44 |
Mode |
30 |
Skewness |
0.04 |
Kurtosis |
-0.37 |
Table 1 We use logistic regression to determine the probability of having a caesarian section given a mother’s age. The results show that the age of the mother does not impact the results. Caesarian section rates remain low regardless of mother’s age
Delivery |
Singlet on birth |
Twin or breech birth |
Total |
Vaginal Delivery |
95 |
32 |
127 |
Cesarean Delivery |
3 |
5 |
8 |
Total |
98 |
37 |
135 |
Table 2 We evaluate whether the proportion of caesarian deliveries varies depending on breech births or twin births. A two-way contingency table analysis (see table below) was conducted and the results show that the type of delivery varies depending on whether the birth was a singleton birth or a breech or twin birth; ,p=0.04. These results show a 96.9% vaginal delivery rate in vertex, singleton home births
Delivery method |
Frequency |
Rate |
Vaginal delivery |
32 |
86% |
Cesarean delivery |
5 |
14% |
Total |
37 |
100% |
Table 3 Post hoc tests indicate that even among these twin or breech births, the rate of caesarian deliveries was much lower (14%) than the rate of vaginal deliveries (86%); ,p<0.05. These results support the claim that caesarian delivery rates are low among homebirths even with breech or twin births
Vaginal birth after cesarean section was attempted 32 times with 30 delivering successfully out of the hospital (93.8%). Of these, 4 were VBA2C and 3 were VBA3C and all of these were successful. Two VBAC moms were transported. One for suspected early scar dehiscence symptoms at 10 cm and the other for a breech arrested at 8 cm. There were no uterine ruptures (Figure 1).
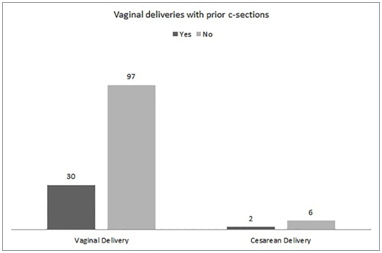
Figure 1 Fischbein Vaginal Deliveries with Prior Cesarean. Chi-Square tests do not show any association between type of delivery and prior C-sections ( , p=.14). These results support the claim that vaginal deliveries increased among this group of homebirth patients even with a previous C-Section.
Many of the mothers chose to labor in water for its analgesic effect. 17% of the mothers delivered their babies in water. There were no complications related to laboring or delivering in the tub. Mothers were allowed to ambulate freely, fluid and nourishment were encouraged and intermittent fetal monitoring by Doppler was performed. Vaginal exams were kept to a minimum, often, not until maternal guttural vocalizations occurred. The birth team consisted of a licensed or certified nurse midwife, the author and often a midwifery student. All licensed personnel were certified in neonatal resuscitation. The assistance of a doula was encouraged.
There were six postpartum hemorrhages (EBL>1000cc) not requiring transport or transfusion in the 127 vaginal deliveries (4.7%).14 Estimated blood loss, based on experience and direct observation, averaged 384ccs. Episiotomy under local anesthesia was performed in 9.9% (n=12) of the 121 women who had a home vaginal birth. There was one 4th degree tear repaired on site. Group B Strep was cultured in 16.3% (n=22) of the women in this series with 22.7% (n=5) not receiving antibiotics either by choice after informed consent or lack of time due to precipitous labor. All babies were evaluated by pediatrics within 2-4 days of delivery and there were no newborn infections. There was one newborn (0.74%) with an Apgar score of 9/9 who was transported to the hospital for persistent tachypnea and found to have a small spontaneous pneumothorax. Only one newborn (0.74%) had a 5-minute Apgar score<7 and this was after a vacuum delivery for prolonged second stage. One baby suffered a fractured humerus during a breech delivery. Neither of these two babies required transport. Average newborn birth weight for singletons was 3649gms (range 2637-5046). Average weight for the vaginal breech singletons was 3369gms (range 2722-4224). Average weight for the 14 twin babies was 2910gms (range 2155-3771).
Fourteen women (10.4%) were transported to the hospital in labor with care transferred to an attending obstetrician. Two went by ambulance. One was the TOLAC woman with the possible signs of scar dehiscence who complained of a change in character of lower abdominal pain and new onset variable decelerations at 10cms. She had a non-emergent repeat cesarean. The other was a multiparous woman with an audible deceleration early in labor who went on to a normal rapid vaginal birth. The remaining twelve went by car. Of these twelve, 5 delivered vaginally and 7 by cesarean section. The overall cesarean section rate was 5.9% in this series (Figures 2 & 3).
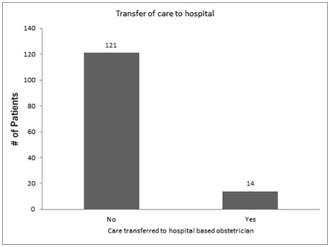
Figure 2 Fischbein Transfer of Care to Hospital.
We also explored the likelihood of hospital transfer among these home births. The rate of transfer of care to a hospital based obstetrician were found to be significantly lower (
, p=<.0001). These results support the hypothesis that properly selected home births result in minimal hospital transfers.
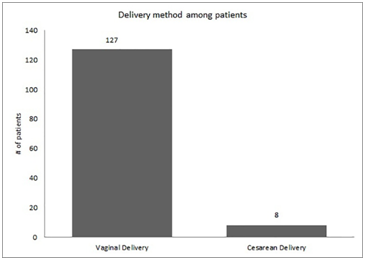
Figure 3 Fischbein Delivery Methods among Patients.
A one sample chi-square was conducted to assess whether home birth affected the number of caesarian deliveries. The results of the test were significant,
, p=<.0001. The cesarean rate of 5.9% is much lower than the 25-40% average rate of caesarian deliveries in Los Angeles County.15
During the 56 months encompassing the delivery of these 135 consecutive women, 22 additional patients were seen in consultation. After proper informed consent, these 22 had planned to deliver at home or birth center. However, prior to the onset of labor they were diagnosed with conditions that made the choice of a hospital birth with an obstetrician a recommended necessity. Therefore, these transfer of care (TOC) clients were not included in the statistics of the first 135 births.
The TOC clients included seven sets of twins. Two had an unstable lie of twin A, one mother developed cholestasis requiring induction, two women had SPROM at 34 weeks, and another went into active premature labor at 34 weeks while the seventh went beyond 41 weeks without any signs of impending labor. Three of these women delivered vaginally. Nine women had breech presentations. Two went into labor when the obstetrician was not in town, one was thought to be macrosomic, two developed oligohydramnios, two went beyond 42 weeks with no signs of impending labor, one developed cholestasis and another decided on elective cesarean birth. All breech mothers in this series were informed of current techniques in encouraging their babies to turn. Most tried chiropractic Webster technique, acupuncture, inversions and suggestions from web sites such as spinningbabies.com.16 External cephalic version was offered when appropriate after education and informed consent. All nine of these breech TOC mothers had cesarean section as no physician on staff at the local hospitals would consider induction or attempt a vaginal delivery. The remaining six TOC mothers had singleton cephalic pregnancies. Two mothers underwent emergent cesarean, one for decreased fetal movement and an abnormal fetal heart monitor at 37 weeks and the other woman had a placental abruption at 34 weeks. One mother had a fetal demise at 39 weeks related to a spontaneous avulsion of a velamentous insertion and another developed preeclampsia at 37 weeks. Both of these women had a successful induction. Of the other two TOC mothers, one went beyond 42 weeks and underwent cervical ripening and medical induction leading to a hospital vaginal birth. The other developed a DVT, received proper medical treatment but went into preterm labor at 35 weeks and delivered vaginally.
Main findings
In this series of 135 consecutive deliveries outside of a hospital the numbers are revealing. The women in this series were selected based on evidence based principles of modern obstetrics. They received prenatal and labor care using the midwifery model of pregnancy as wellness. The success rate of laboring women with planned home delivery was 88.9%. Included in the 135 births were 30 VBACs, 27 singleton breech deliveries and 5 of 12 sets of twins with at least 1 twin with a non-vertex presentation yet there were only 8 cesarean sections.
Of the 135 women in the series there were 15 transports of which 7 delivered vaginally resulting in an overall 5.9% cesarean section rate. Five of the eight cesareans were breech mothers who had a stalled labor beyond 7cm. If they had the option of a transport for an epidural and pitocin augmentation as mothers with vertex babies do the overall cesarean rate may have been lower still. Immeasurable, but no less important, was the respect for the microbiome and mother-baby unity as well as personal satisfaction and emotional health of the mother and the family unit at the moment and in the future. There is growing evidence that health is directly related to early exposure to parental bacteria.6 Vaginal birth and skin to skin contact are essential for proper gut and respiratory tract colonization. This is enhanced in the home birth model where there are no restricting policies or protocols to interfere. There is also growing evidence to suggest the mode of delivery can affect the epigenetic state of neonatal stem cells which may have important implications for health and disease in later life.5 Eliminating the unnecessary surgical birth is clearly a worthwhile goal.
Strengths & limitations
It is acknowledge by the author that many of these pregnancies would be considered high risk and not standard fare for out of hospital delivery. In addition, specialist training in the skills of breech and twin delivery has been waning limiting the possibilities for easy replication or confirmation. In this series labor was seen as a normal process and when allowed to progress unfettered we did not see the sudden deterioration that is common in the intervention-induction-epidural cascade. Women seeking home birth tend to be more educated about and involved in their care and decision making for the very reason they are going outside of the norm.
Interpretation
The practice of the modern day obstetrician has changed significantly over the past 30 years. Much has to do with outside forces of economics, expediency and medico-legal concerns. However, the response of the academic and organizational leaders of our specialty has been ill-directed and not led to a commensurate level of improved outcomes. Technology and specialty consultation have seen an increase while training in the skill set that make obstetricians unique has all but disappeared.17 The process of growing a human fetus and laboring is not a disease. When a laboring mammal is anxious, disturbed, interrupted, restricted in movement or starved its labor will likely be dysfunctional. The human female is no different. Respecting the normalcy of human birth will lead to better outcomes. When given true informed consent, highly motivated women with what is classically considered “higher risk” pregnancies can deliver safely at home with low cesarean section rates when attended by a skilled practitioner.6,9
The midwifery model of care respects the normalcy of mammalian pregnancy and birth and the woman as an individual. Extensive experience working in both hospital and home is relatively rare in the birthing debate but has given the author a unique perspective from which to observe and comment. When healthy mothers are given individualized preventative care and selected properly by a well-trained practitioner the results are enlightening. When families are given true, not skewed, informed consent and take an active role in their own pregnancy then the ethical obligation to respect their reasonable choices is fulfilled.18
Home birth is not for everyone but informed choice is. The patronizing statement, “home delivery is for pizza”, is unprofessional and has no place in the legitimate discussion. Some suggest making hospital birth more homelike. While this may be a beginning and deserves investigation, it fails to recognize the difficult balance between honoring normal undisturbed mammalian birth and the reality of the hospital model’s legal and economic concerns and policies. This series of 135 home deliveries by a team of obstetrician and midwife clearly shows there is a model that can do better than what we have now as the American standard. Safety is always considered and the home birth clients in this series were well informed and aware that there are no guarantees of perfect outcomes in any setting. Pregnant women deserve to know that midwifery style care, both in and out of hospital, is a reasonable choice. A collaborative model between obstetrician and midwife can provide better results than what is occurring today. Midwives are experts in normal birthing and therefore readily recognize abnormal. Obstetricians are trained as experts in abnormal pregnancy and in that we excel. It would be wise to put the constructive energy of our profession towards the training of future practitioners in the skills that make obstetricians truly specialists such as breech, twin and operative vaginal deliveries. Lowering the cesarean section rate is a worthy goal and educating the next generation of obstetricians in these skills must be done before they are lost. Home birth will continue to grow as educated women realize that the current hospital model has many flaws. Cooperation, respect and smooth transition from home to hospital honors the pregnant woman and is our ethical obligation.
The author wishes to thank the midwives he works so closely with.

©2015 Fischbein. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.