eISSN: 2377-4304


Case Report Volume 15 Issue 1
Prof in ObGyn, University of Nicosia - Medical School, and Aretaeio Hospital, Cyprus
Correspondence: Vasilios Tanos MD, PhD, Prof in ObGyn, University of Nicosia - Medical School, and Aretaeio Hospital, 55-57 Andrea Avraamides Str., Strovolos, 2024, Nicosia, Cyprus, Tel ++357 99683488, Fax + 357 22512371
Received: January 26, 2024 | Published: February 6, 2024
Citation: Tanos V. Hysteroembryoscopy in repeated early pregnancy loss due to suspected thrombophilia. Obstet Gynecol Int J. 2024;15(1):21-23. DOI: 10.15406/ogij.2024.15.00728
Introduction: The cause of a 1st trimester repeated pregnancy loss (RPL) under treatment with aspirin and /or heparin due to suspected thrombophilia was investigated. Using hystero-embryoscopy (HEpy) and embryo genetic analysis the embryo development was correlated to its karyotype.
Patients and methods: Seventeen first trimester pregnant women recruited in the study. They all had a history of at least 2 consecutive 1st trimester recurrent miscarriages, underwent an investigation for the cause of RPL and diagnosed to suffer from hypercoagulation. Thromboprophylaxis was administrated in all 17 pregnant women during their next pregnancy, postulating that their past cause of miscarriage was due to a hypercoagulability state. Twelve patients had positive Anticardiolipin and /or Antiphospholipid antibodies and 5 patients had MTHFR high titers.
Embryo autopsy was performed by hysteroscopy technique using 2.9mm – 5mm hysteroscopes, 5Fr graspers and scissors and normal saline as distending medium. The embryo morphology results were correlated with the genetic results and compared with the patients’ diagnosis and treatment during the last miscarriage.
Results: HEpy revealed that in 11 out of 17 cases embryos had chromosomal abnormalities ensuring patients that the problem of their loss was not the followed treatment. In all 4 cases with decidua haematoma and umbilical cord defect patients received aspirin and LWMH, raising the possibility of anticoagulation overtreatment.
Conclusion: In-situ autopsy of a miscarriage embryo can provide useful information regarding the morphology of the embryo, ruling out anatomical defects and collecting the embryo under direct vision anticipating an accurate embryo karyotyping. Embryoscopy results may assist to change the management of the next pregnancy in RPL cases and patients with hypercoagulability state.
Keywords: hystero-embryoscopy, thrombophilia, repeated pregnancy loss
Repeated pregnancy loss (RPL) occurs in 1–3% of couples aiming pregnancy. Involves mainly young and nulliparous women, usually experiencing miscarriages at 6-11 weeks' of gestation. In these RPLs the embryo aneuploidy is found in over 50% of the cases. Hence, patients with RPL require screening consideration, assessing the risk for prenatal lethal recessive diseases.1–3
Around 19% of RPL cases are diagnosed with antiphospholipid and anticardiopilin syndrome.4 In a study by Jaslow and Kutech in 260 out of 1020 RPL patients, 25% were positive for Lupus anticoagulant, anticardiolipin and Factor V Leiden.5 Although some thrombophilias appear to be more common in women with RPL, screening is not currently recommended due to limited evidence. Many RPL patients might be positive for MTHFR mutations however, it is not proved that leads to thrombosis and miscarriage. American College of Obstetricians and Gynaecology and American Society of Reproductive Medicine do not recommend genetic testing for inherited thrombophilias in women with RPL. Both societies indicate that screening may be considered if patient has personal or family history (1st degree relative) of venous thromboembolism.6,7
Patients follow usually a standard investigation protocol for the RPL cause, excluding congenital uterine anomalies, acquired myometrial, endometrial and cervical pathologies, microbiological, endocrine, alloimmune, autoimmune and congenital thrombophilic factors.7,8 However, a 50% of these patients have no firm diagnosis and are treated empirically.9,10
Patients with RPL, treated with aspirin and heparin or heparin alone due to suspected thrombophilic factors underwent in-situ embryo autopsy and genetic analysis by hystero-embryoscopy. Seventeen patients with history of over 3 RPL, admitted in our department between 2012 – 2016, due to 1st trimester repeated miscarriage. From the selected patients cohort the following data was collected: clinical history, physical examinations including gynecological examination findings and laboratory investigations, along with their results from hystero-embryoscopy and Dilation and Curettage (D&C).
The inclusion criteria of the patient cohort were all women with:
During the procedure the patients were placed in the lithotomy position. Neither analgesia nor anaesthesia was used for the stage of embryoscopy. Embryoscopy of the embryos was performed using Hysteroscopes of 2.9mm and /or 5mm telescope with 30o optic connected to cold light and normal saline as distending medium (Figure 1). The embryo was evacuated under direct vision and send to cytogenetic analysis. Hegar 9mm was the maximum cervical dilation before suction curettage.
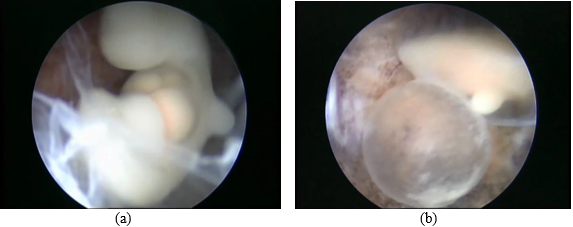
Figure 1 The figure 1 presents, a) embryo with omphalocele and underdeveloped extremeties and b) yolk sac and embryo observed trans amniotic sac membrane.
For the evaluation of embryo development and the classification of the morphologically normal and abnormal embryos, the Carnegie human embryo staging was followed.11 The genetic analysis performed up until year 2014 was using embryo tissue cultures, DNA extraction as well as cytogenetic analysis. By the year 2015 the genetic analysis used was performed using CGH.12
Patients’ mean age was 31 (26-39). Seven women were over 35 years of age. Nine patients were treated with In Vitro Fertilisation and Embryo Transfer (IVF-ET) and the rest were after spontaneous pregnancies. Embryoscopy revealed 11 out of 17 embryos (65%) with chromosomal and morphological abnormalities, 1 case with umbilical cord defect, 3 cases with decidua haematoma and in 2 cases diagnosis failed. In 2 IVF cases TVU diagnose a twin pregnancy prior to hystero-embryoscopy while the second one was discovered only during the procedure.
Embryo in situ autopsy and karyotyping is the method of investigation for the causal identification of miscarriages in RPL cases facing an additional 1st trimester loss, after spontaneous or artificial conception, and while being treated by aspirin and/or low molecular weight heparin (LMWH). The high rate of chromosomal aberrations is expected in RPL, however in 4 out of the 17 cases with normal embryo genetic analysis decidua haematoma and umbilical cord defect were found. In 7 patients with age over 35 the embryos had chromosomal abnormalities. Although age remains the main factor contributing to RPL, the associated high rate of chromosomal abnormalities despite treatment for these patients, further indicates subsequent unknown yet, sub-clinical conditions which can also contribute to genetic abnormalities during fertilization. The assisted reproductive technology techniques employed can correspondingly have an impact. There is a reported increased risk of chromosomally abnormal products of conceptions when compared to natural conception which result in early pregnancy loss (Figure 2).13
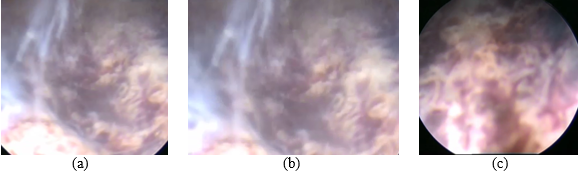
Figure 2 Presents, a) Decidua haematoma panoramic view, b) Decidua haematoma close up view and c) Decidua fresh blood coagulum next to old clot.
Despite immunological factors being more complex than before, due to the evolution of technology and deeper understanding of disease, coagulopathies including thrombophilia are diagnosed in significantly less patients.10 Acquired and inherited thrombophilia has been implicated in recurrent IVF-ET failure. Oublan et al. 2008 investigated the effect and safety of thromboprophylaxis using LMWH in women with recurrent in vitro fertilization (IVF)-embryo transfer (ET) failure and thrombophilia.10 The LMWH-treated group observed a significant increase in the live birth rate, compared with that of the placebo (23.8% vs. 2.8%, respectively; p < 0.05). Additionally, the abortion rate was significantly higher (p<0.05) in the placebo-treated group compared to the LMWH-treated group. Reportedly, the treatment complications frequency did not differ between the two study groups. It is safe to conclude that the use of LMWH is a safe and effective thrombo-prophylactic treatment for women with proved thrombophilia and recurrent IVF-ET failures.10 Many of the RPL cases are still treated arbitrarily using steroids and/or aspirin or solely low weight molecular heparin. Many colleagues continue to prescribe low dose aspirin in RPL patients and repeated implantation failures after ET by IVF cycles, although this treatment is not supported by the literature. The positive effect of prolonged and / or short treatments of low dose aspirin in RPL or repeated implantation failure is disputed.
All patients received LWMH without clear proved of thrombophilia estimating that their past cause of miscarriage was a hypercoagulability state. This was evident only after borderline laboratory results or MTHFR heterozygous suspicious high titers. Interestingly HEpy revealed that in 11 out of 17 cases embryos had indeed chromosomal abnormalities. This allows the confirmation to patients, explaining that the problem of their pregnancy loss was not the followed treatment. It is important to note that in all 4 patient cases with decidua haematoma and umbilical cord defect received aspirin and LWMH, raising the possibility of anticoagulation overtreatment (Figure 3).
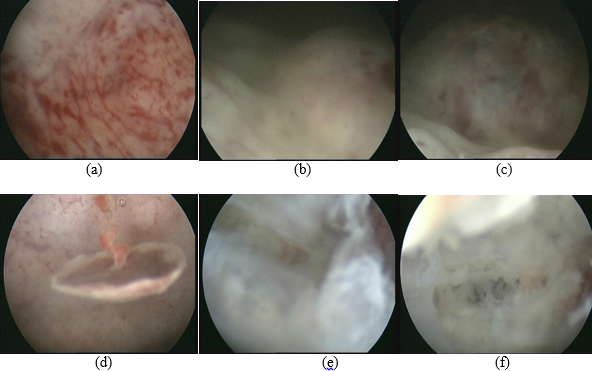
Figure 3 Endometrium covered with clots and petechiae. The pregnancy sac was implanted in the posterior uterine wall very close to the cervico-uterine junction. A pedunculated polyp was diagnosed hanging from the fundus. Prominent extravasation of the decidual vessels. Normal syncytiotrophoblast. The amniotic membrane was irregular with a bundle of threads however, no embryo or yolk sac were identified.
Many RPL cases are treated arbitrarily. This is primarily attributed to a lack of sufficient evidence establishing the connections between patient's and prior miscarriages. HEpy has the potential to reduce both the instances of undiagnosed and misdiagnosed cases, along with minimizing unnecessary treatments, including empirical approaches. Additionally, it has the capability to lower the psychological stress of the women. Additionally, for cases that have undergone diagnosis and treatment, there remains a risk of subsequent miscarriage in subsequent pregnancies. Correlating embryo morphology results with genetic findings and comparing them to the patient's diagnosis, ultrasound observations, and treatment history from the previous miscarriage can enhance our understanding. The outcomes related to the causes of miscarriage post-treatment could contribute to evaluating the accuracy and effectiveness of the therapy.
None.
None.
Author declares that there is no conflict of interest.

©2024 Tanos. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.