eISSN: 2377-4304


Case Report Volume 14 Issue 5
Residente de tercer año de Ginecología y Obstetricia, Hospital Christus Muguerza Conchita, México
Correspondence: Julio Palau Torre, Residente de tercer año de Ginecología y Obstetricia, Hospital Christus Muguerza Conchita, Monterrey, Nuevo León, México
Received: September 14, 2023 | Published: September 25, 2023
Citation: Palau Torre J. Hysterectomy via vNOTES approach. A case report. Obstet Gynecol Int J. 2023;14(5):134-137. DOI: 10.15406/ogij.2023.14.00711
Background: vNOTES (Vaginal Natural Orifices Transluminal Endoscopic Surgery), performed for the first time in 2010, is an emerging surgical technique that eliminates surgical trauma to the abdominal wall, through the use of natural orifices. Here we describe a case where this approach was used with excellent results. Due to the lack of reports using vNOTES surgery in Mexico, we present a case where this approach was achieved with excellent results.
Objective: To report a case of hysterectomy using the vNOTES approach.
Clinical case: A 60-year-old female, asymptomatic, referred for definitive procedure due to cervical intraepithelial neoplasia, after not accepting conservative management. A hysterectomy was performed using the vNOTES approach, lasting 100 minutes, with no eventualities or postoperative complications. She was discharged 24 hours after surgery, hemodynamically stable and asymptomatic, and without late complications.
Conclusion: A hysterectomy was performed using the VNOTES approach successfully and without complications, with an adequate post-surgical evolution. Current evidence shows that the vNOTES approach to hysterectomy is an effective and safe surgery, which also combines the advantages of the vaginal approach with the laparoscopic approach.
Keywords: vNOTES, hysterectomy, laparoscopic hysterectomy
Transvaginal natural orifice transluminal endoscopic surgery or vNOTES, for its acronym in English, is an emerging technique where access to the peritoneal cavity is made through the vagina (as a natural orifice). The vNOTES surgical approach represents a fusion between the vaginal approach and laparoscopic surgery, improving the safety of the procedure and the gynecologist's confidence, expanding the vision of the surgical field and achieving an adequate hemostatic seal of the pedicles. This procedure preserves the advantages offered by the vaginal approach and eliminates its drawbacks, such as poor visualization and limited surgical space.1
Just as the laparoscopic route has been, the vNOTES technique has also been the victim of skepticism from some gynecologists.2,3 The current trend in surgical procedures is to perform them in an increasingly less invasive manner. The “NOTES” surgical approach has the objective of eliminating surgical trauma to the abdominal wall, through the use of natural orifices and, consequently, reducing the inflammatory response by producing less inflammatory cytokines, resulting in less post-surgical pain.4,5
Hysterectomy was the first gynecological procedure performed by vNOTES in 2010, and since then various benign procedures such as myomectomies and oophorectomies have been performed.2 The vNOTES approach has shown certain advantages compared to conventional laparoscopic surgery, especially for uteruses that do not present prolapse or other benign uterine pathologies. In 2020 Housmans et al.6 conducted a systematic review to describe its advantages and reported that this approach over the laparoscopic approach is related to shorter surgical time, fewer postsurgical infections, shorter hospital stay, and possibly less postsurgical pain.6,7
Currently, the indications for performing a hysterectomy through the vNOTES technique are reserved for benign uterine pathologies that require surgical treatment such as abnormal uterine bleeding, myomatosis and/or adenomyosis, and which ideally relate to nulliparous and/or obese patients with an enlarged uterus that makes the vaginal route difficult, a uterus without descent and restricted vaginal space (including patients who have not initiated sexual activity).6–8
According to the American College of Obstetricians and Gynecologists (ACOG), vaginal hysterectomy has been recommended when the technique is feasible, which depends on the characteristics of the patient (such as body mass index, uterine volume, uterine descent, size and shape of the vagina, history of cesarean section or previous surgeries), as well as the surgeon's experience with vaginal hysterectomy.9,10 In vNOTES hysterectomy, the procedure begins as a conventional vaginal hysterectomy, and after anterior and posterior colpotomy and transection of the utero-sacral ligaments, with or without adnexectomy, it is continued with conventional laparoscopic instruments through vNOTES.11 Through vNOTES surgery, the indications for conventional vaginal hysterectomy can be expanded and allow resection of larger uteri without abdominal incision and/or without comorbidity associated with open surgery. In Mexico there is little experience with this technique, however, it must be recognized that its use is feasible in the region, depending on the resources and experience of the surgeons, as well as the characteristics of the patients and shared decision making between the doctor and the patient. For this reason, we present a case where the vNOTES technique approach was used, with excellent results.
A patient was selected who met the criteria for performing the technique, previously scheduled for laparoscopic hysterectomy and with authorization to perform the technique, with prior informed consent, where the advantages of the approach were explained through vNOTES. Since the patient had no contraindications for the previously planned laparoscopic approach, the vNOTES approach was considered after the patient expressed her preference for a surgical method that did not leave scars, as well as a lower risk of incisional hernia.
This was a 60-year-old patient referred for a definitive procedure due to a low-grade cervical intraepithelial lesion since she did not accept conservative management. As important history, the patient had high blood pressure, type 2 diabetes mellitus, hypothyroidism and osteopenia. Under adequate medical control, weight of 67 kg and body mass index of 26.5kg/m2. Surgical history: tonsillectomy, salpingoclasia and bilateral saphenectomy. Obstetric and gynecological history: 4 pregnancies, 4 births, menopause at 53 years of age. On physical examination: atrophic vagina and cervix, without uterine descent.
For the procedure, the GelPOINT Mini advanced access platform (Applied Medical, Rancho Santa Margarita, CA) was used (Figure 1) to maintain pneumoperitoneum and introduce the laparoscopic forceps. After the application of balanced general anesthesia, the patient was placed in a gynecological position, asepsis and antisepsis of the vulvovaginal region were performed, and a Foley catheter and sterile fields were placed. The steps that were carried out are described below:
In this case, the technique was successful and was carried out without any eventuality or complications, with a total duration of 100 minutes. The patient's evolution was favorable, with mild or no pain during follow-up, well controlled without requiring rescue analgesia, with removal of the urinary catheter 8 hours after surgery and initiation of early ambulation. The patient was discharged 24 hours after surgery, where she remained hemodynamically stable and asymptomatic. In the days after surgery, no late complications were reported. Local treatment with estrogens was indicated for one month to improve the conditions of the epithelium and genitourinary symptoms associated with menopause.
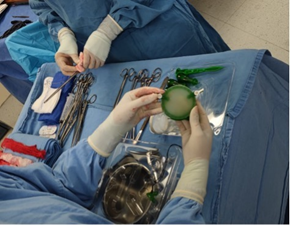
Figure 1 The GelPOINT Mini advanced access platform (Applied Medical, Rancho Santa Margarita, CA) was used to maintain pneumoperitoneum and introduce the laparoscopic forceps.
Hysterectomy remains one of the main surgical indications for benign gynecological pathology around the world.12 There are currently four approaches to perform this surgery, including vaginal, abdominal, laparoscopic, and robot-assisted hysterectomy. The proportions of performing each of these vary between countries, however, the one that is most commonly performed as a preferred route for benign indications is abdominal hysterectomy.9 Despite this, vaginal hysterectomy is superior to all previous ones,13 because it is the safest and least invasive, with the advantage of a faster return to activities of daily living. This technique is the first choice when it is feasible to perform it, and it is recommended by both ACOG and the International Society of Gynecology and Endoscopy ( ISGE).9,10 However, vaginally , prophylactic resection of salpinges and/or ovaries is performed 4 to 12 times less compared to the laparoscopic or abdominal route.14
The surgical approach through natural orifices is a technique with increasing popularity in recent years, since it represents a fusion between the ideal procedure for performing a hysterectomy (vaginal) and technological advances with the use of tools used in surgery laparoscopic. Although some patient characteristics (such as large uterine size, narrow vagina, lack of uterine descent, and previous cesarean section) may limit vaginal access, in experienced hands, they should not be contraindications to vaginal hysterectomy.9,10 In practice, the lack of gynecologists with adequate training in vaginal hysterectomy has been associated with an increase in laparoscopic hysterectomies as the standard for the management of benign gynecological pathology.9 vNOTES may be an approach that adds the advantages of endoscopy with better visualization of the pelvic anatomy, increasing the indications for conventional vaginal hysterectomy in cases of limited vaginal access.
The first surgery using the VNOTES technique was performed in September 2021 at the Hospital Clínica Nova de Monterrey, Nuevo León, Mexico. To our knowledge, this is the first national report on the use of this technique, considering the approach described by Dr. Chua,15 where he suggests that this procedure is safe and effective in multiparous patients, without a history of cesarean section or major abdominal surgeries, with a minor degree of uterine prolapse (grade 1 or 2), clinical examination with adequate uterine mobility and benign gynecological pathology.
From September 2021 to July 2022, 7 hysterectomies have already been performed using the same approach with excellent results, in patients with an average age of 45 years (with a range between 34-60 years), 3 (42.8%) with a BMI <30kg/m2. The uterus with the highest weight reported was 440 gr. With the exception of the patient reported in this case, all had an indication for hysterectomy due to abnormal uterine bleeding that required surgical management. All patients had a successful approach, without immediate or late post -surgical complications. The median operative time was 110 (interquartile range [IQR], 100-130) minutes, with a median surgical blood loss of 85 (IQR, 50-350) ml. Nulens et al.16 reported 114 cases in a study of vNOTES hysterectomy indicated by enlarged uterus. In their study, the average age of the patients was 50 years, 19% were obese and 3.5% were morbidly obese. The sizes of the resected uteri were 281 to 3361 g, with an average weight of 559 g, and with an average surgical time of 63 minutes, 13 minutes shorter compared to the patient in our case. The main complications reported by the authors were: bleeding in the first 24 hours in 2.6% patients, one case of late minor complication, a conversion rate to open surgery of 0.9% and a success rate of 99%. Similar to our data, the authors reported no complications from ureteral, bladder, or intestinal injuries, nor life- threatening complications or intensive care unit admission.16
Housmans et al.6 published a study with meta-analysis that included a controlled clinical trial and five studies that compared vNOTES hysterectomy with conventional laparoscopic hysterectomy (total or laparoscopic-assisted vaginal hysterectomy) in adults with benign gynecological pathology, and found an association of shorter surgical time and blood losses with the vNOTES approach, although there were no differences in the rate of postoperative complications, pain scores at 24 hours and changes in hemoglobin levels one day after surgery. Their study also recognized the lack of more reports about specific populations that use this technique.6
On the other hand, Mat et al.17 reported six cases of obese patients with early-stage endometrial cancer who were approached by hysterectomy by vNOTES. According to the authors' data, no patient required conversion of the surgery and they highlighted the importance of expert management for this technique in malignant pathologies,17 therefore, this procedure can be useful for patients with malignant pathology, although it is required more studies to be able to establish the precise indications that could demonstrate the feasibility of surgery in this group of patients, as well as the short and long-term repercussions. Kaya et al.18 compared the outcomes of laparoscopic hysterectomy with vNOTES hysterectomy for obese patients, and found that the latter technique was associated with shorter surgical time and shorter hospitalization time compared to classic laparoscopic hysterectomy, and similar to the aforementioned study, they commented on the need of appropriate surgical skills and competencies in vNOTES.18
Regarding the results found with vNOTES, there have been discrepancies between authors. Similar to our data, Kale et al.18 have reported a favorable evolution in patients treated by vNOTES. In their work, where they reported their experience with the vNOTES technique for hysterectomy and salpingo-oophorectomy in 13 women with indication for benign pathology, in which there were no complications or conversion of the surgery, high patient satisfaction, advantages cosmetics and, above all, less postoperative pain.8 However, one of the current limitations of this technique is that, because it is new and not so widely used in different centers, there is a lack of studies with sufficient evidence that can support the preference of this technique over other approaches for hysterectomy. In addition, in our center we currently have insufficient cases using this technique to detail a complete report. Furthermore, one of the limitations presented in our case report was a more detailed documentation of the patients' characteristics (or the communication of a series of similar cases in our center), as well as a longer-term follow-up or assessment of patient satisfaction months after surgery.
Some recommendations can be made based on the experience that has been developed with the team, which is undoubtedly an effective approach. Also, it is a safe route for resection of salpinges and/or ovaries. I agree with you different authors mentioned and based on the analysis that has been seen of the patients operated with vNOTES, their satisfaction levels are high. Likewise, there is talk of an approach that equals the effectiveness of laparoscopic hysterectomy. In some particular cases, such as early-stage endometrial cancer, it could be an option in well-selected patients. However, it should be taken into account that it is not an alternative to vaginal hysterectomy, rather it is an alternative option to the laparoscopic route.
Technological advances have improved the tools available to doctors in order to improve the quality of their surgical procedures and obtain better outcomes for patients. Although the vNOTES approach has been practiced for approximately a decade, this is the first hysterectomy using this technique reported in Mexico. With the publication of this case report, the recommendations of the VNOTES approach, and the advantages it offers, it is intended to serve as a watershed for this technique to be adopted more frequently, since it has been shown to be less invasive, with better aesthetic results, less time surgery, shorter hospital stay and decreased post-surgical pain, as well as a faster recovery of patients and return to daily activities in less time. Another advantage of this technique is that it offers greater ergonomics to the medical team. It is important to mention that the objective of the laparoscopic approach when performing a hysterectomy is to avoid the abdominal route, the VNOTES technique aims to be a substitute for the laparoscopic approach and thus return to the vaginal route as the approach par excellence for this surgery.
None.
Ethical considerations
The patient gave her informed consent and the Ethics Committee of Hospital Clínica Nova, and also gave her consent for the publication of the clinical case.
None.
The authors declare no conflict of interest.

©2023 Palau. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.