eISSN: 2377-4304


Case Report Volume 14 Issue 5
1Ginecología oncológica, Hospital Central de Apizaco, Tlaxcala, Mexico
2Anatomopatóloga, Integramedik Tlaxcala, Mexico
3Urología y andrología, Hospital Ángeles Puebla, Mexico
4Academia Nacional de Medicina, Academia Mexicana de Cirugía, Mexico
Correspondence: Víctor Manuel Vargas-Hernández, Women’s Health Clinic, Insurgentes Sur 605-1403, Nápoles 03810, Mexico, Tel (52)5552 179782
Received: September 12, 2023 | Published: September 21, 2023
Citation: Vargas-Aguilar VM, Sanchez-Rodriguez S, Ordoñez AOI, et al. Giant condyloma, buschke-löwenstein tumor in the penis, presentation of a case and review of the literature. Obstet Gynecol Int J. 2023;14(5):129-132. DOI: 10.15406/ogij.2023.14.00710
Background: Buschke-Löwenstein tumor is a presentation of condyloma acuminata; caused by human papillomavirus infection presenting as an exophytic, polypoid, cauliflower-like lesion; characterized by slow growth, local infiltration, contiguous tissue destruction; with a tendency to recurrence and produce fistulas or abscesses around the affected area. The most frequent location is the vulva, scrotum, penis, perineum and perianal region; Transmitted by sexual contact and more common in men, it is controversial whether it should be considered premalignant or a verrucous carcinoma; It does not present cellular atypia and a third can become malignant; recurrences are frequent. The risk factors are HPV, continuous irritation and poor hygiene of the genital area, phimosis, immunosuppression, smoking and drug addiction.
Objective: review literature and case description.
Case presentation: 45-year-old male with condylomatous lesion on the genitals of 4 months' duration, on the foreskin and ligament of the glans penis, and other minor lesions on the shaft of the penis; morbid obesity, uncontrolled type 2 diabetes mellitus. He is scheduled for circumcision and removal of the satellite lesions.
Conclusion: Giant Buschke-Löwenstein condyloma is considered a low-grade squamous cell carcinoma, locally invasive, with aggressive behavior; Surgical treatment is the option.
Keywords: Buschke-Löwenstein tumors, giant condyloma acuminata, human papillomavirus, surgical excision
The Buschke-Löwenstein tumor was first described in 1886 by the German dermatologist Abraham Buschke; It is a strange manifestation of condyloma acuminata, it begins as a small gradual keratotic growth over several years and transforms into a mass similar to a cauliflower; It occurs in the vulva, scrotum, foreskin, coronal sulcus of the penis, perineum and perianal, extremely rare in the rectum and bladder.1,2
Macroscopically, it presents as an exophytic, polypoid lesion; similar to a cauliflower, characterized by slow growth, local infiltration, contiguous tissue destruction, with a tendency to recur and produce fistulas or abscesses around the affected area. The idea that Buschke-Löwenstein tumor should be considered a premalignant lesion with a high potential for malignant degeneration or a clinical manifestation of verrucous carcinoma is controversial;3 occurs more frequently in men than in women; mainly uncircumcised and under 50 years old; Incidence rates are higher in men who have sex with men; It is caused by low-risk human papillomavirus (HPV) serotypes; HPV-6 and 11.3,4
The genome of HPV serotypes encodes DNA sequences that produce E (early) proteins E6 and E7;4 which bind to the tumor suppressor protein that leads to accelerated degradation of p53, immortalizes epithelial cells and accumulates DNA mutations, causing chromosomal instability and finally abnormal growth; They exhibit a densely keratinized and well-differentiated epithelium. Microscopically, it is formed by hyperplastic, well-differentiated epithelium, with hyperkeratosis and the presence of coilocytes exhibiting papillary structures with defined nuclei of fibrovascular nature, characteristics similar to condyloma acuminatum. It is characterized by distinctness and well-developed underlying tissue, often called an endophytic pattern without atypia.5–8 Some authors consider it an intermediate lesion between condyloma acuminatum and verrucous carcinoma. The risk factors are HPV positivity, continuous irritation of the genital area and poor hygiene, phimosis, immunosuppression, low socioeconomic status, smoking and drug abuse. Gadolinium magnetic resonance imaging is used to look for tumor expansion to plan surgical removal.7 Sentinel lymph node biopsy is considered if necessary; although it generally does not metastasize. Latent disease can become active, particularly with pregnancy and immunosuppression; Lesions may return spontaneously, remain the same, or progress.7 Regarding prognosis, its malignant transformation has been reported to be 30 to 50% with an associated mortality of 20%.7–10
Different types of treatment are reported that depend on the size, number and location of the lesion, immunological status of the patient, personal preferences and available resources.11 In general, a wide surgical excision is the treatment of choice,12 with a success rate of 63-91% and a lower risk of recurrence. Other treatments are described such as podophyllin gel, 5-fluorouracil, bleomycin combined with cisplatin, methotrexate or interferon alfa to reduce size, there are no standard guidelines or doses, imiquimod 5%, applied 3 times a week at night and up to 16 weeks, complete responses were reported in 37 to 54% of patients; Recurrence occurs in 19% of cases after 12 weeks of follow-up;14,15 cryotherapy alone or in combination with topical 5-fluorouracil obtains good results, laser phototherapy, CO2 or argon laser, is reserved for recurrence; Its advantages are the hemostatic incision and sterilization of the wound (16). Radiotherapy is controversial since it can induce dedifferentiation of tumor cells, progression of the lesion, even malignant transformation to anaplastic carcinoma and metastasis;1,15–17 the effectiveness of neoadjuvant chemoradiotherapy at 45 Gy in the pelvis plus an increase of 14.4 Gy to the primary tumor, for a total of 59.4 Gy concomitant with mitomycin-C or 5-fluorouracil and subsequent local surgical excision, showed complete regression, in case of recurrent tumors after radiotherapy alone or surgical excision. Flap reconstructive surgery is used to cover the defect that remains after its removal.18 Autologous vaccination therapy as a treatment has promising results.11,12
Important differential lesions include condyloma acuminatum, squamous cell carcinoma (including papillary, verrucous, and cuniculatum carcinoma), primary rectal adenocarcinoma, bowenoid papillomatosis, and lymphangiomas.19–21
Inadequate treatment or natural evolution has a fatal course due to its locally destructive nature. It spreads and erodes pelvic organs and bones, even with proper treatment; the mortality rate is 21% and the recurrence rate is 68%; 56% present malignant transformations. Complications are frequent and typical of the treatment and include fistula formation, secondary infections, malodorous discharge, frequent recurrences and malignant degeneration. Parental education is necessary regarding circumcision of the newborn,22 the use of condoms, and The HPV vaccine should be given to people ages 9 to 26.23–26
This is JMLM, a 45-year-old male food merchant, who lives in a common law union in a rural area of Tlaxcala, Mexico. With a condition in the genitals of 4 months of evolution, characterized by condylomatous lesions in the foreskin and glans ligament (Figure 1), and other minor lesions in the shaft of the penis; As a significant history, he has type 2 diabetes mellitus with a history of 15 years and no treatment for 1 year, laboratory with triglycerides of 300 mg, glucose of 306 mg, HbA1c of 15; Treatment for metabolic control was started and a preoperative evaluation was performed to rule out immunodeficiency due to human immunodeficiency virus. PCR for human papillomavirus was not performed; The extent of the lesion was evaluated and circumcision and removal of the satellite lesions by electrosurgery were scheduled (Figure 2), the histopathological report with a diagnosis of condylomas and Buschke-Lowenstein tumor (Figure 3); In the histological sections of the five lesions, skin is identified which presents alteration of its histoarchitecture at the expense of a benign lesion with parakeratosis, hypergranulosis and acanthosis with a papillary growth pattern, with fibrovascular stems with thin-walled vessels that have erythrocytes inside. , are covered with squamous-type epithelial cells, which are medium-sized with eosinophilic cytoplasms, central, round nuclei, some of them hyperchromatic with irregularly shaped membranes and clear perinuclear halos (Figure 4). Surgical procedure ends (Figure 5).

Figure 3 Irregular fragment of skin measuring 4.5x2x2 cm. On one side it has a gray epidermis with a rough appearance and a papillary appearance. When cut, it has a soft consistency, with a white internal surface with a fibrous appearance.
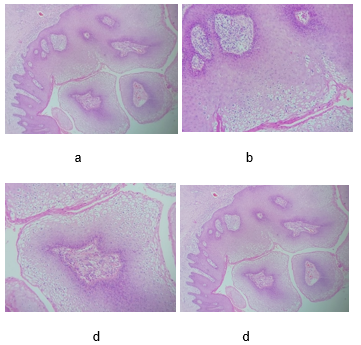
Figure 4 10X microscopy, stained with H&E, showing cytopathic changes associated with human papillomavirus infection, superficial cells with clear perinuclear halos and irregularity in the membrane. In the histological sections of the five lesions, skin is identified which presents alteration of its histoarchitecture at the expense of a benign lesion with parakeratosis, hypergranulosis and acanthosis with a papillary growth pattern, with fibrovascular stems with thin-walled vessels that have erythrocytes inside. , are covered with squamous-type epithelial cells, which are medium-sized with eosinophilic cytoplasms, central, round nuclei, some of them hyperchromatic with irregularly shaped membranes and clear perinuclear halos. Diagnostic impression: condylomata acuminata of foreskin; surgical edges free of injury.
Sexually transmitted diseases are one of the main causes of morbidity in the world; It is estimated that around 330 million people are affected each year. Unprotected sexual contact is the main cause of infection and autoinoculation of genital warts through personal or poorly sterilized items, use of humid areas such as bathrooms, saunas and swimming pools shared with patients carrying the disease. The incubation period for human papillomavirus is one to six months. HPV co-infection is common with HIV, as the two viruses share a common transmission route. Furthermore, patients with HIV are more susceptible due to a local immunodeficiency that makes it difficult to eliminate HPV and this causes the progression of the lesions.29,30–35
Giant condyloma or Buschke-Löwenstein tumor often pose a diagnostic dilemma. These patients may present with nonspecific signs and symptoms, such as pain, hemorrhage, abscesses, and anogenital/penile tumor, which presents as a slowly growing, exophytic, warty, cauliflower-shaped benign lesion; how was the development in our patient.29,30 It is currently considered a locally invasive low-grade squamous cell carcinoma, which is why it sometimes shows aggressive behavior due to rapid growth and develops complications such as fistulas and destruction of neighboring structures; In this case it did not reach those circumstances and did not have a malignant transformation; although, up to 50% can become malignant; It can be confused with condyloma acuminata, cutaneous squamous cell carcinoma (papillary, verrucous and cuniculatum), primary adenocarcinoma of the rectum, bowenoid papulomatosis and lymphangiomas; In this case, the diagnosis was made with physical examination and confirmed by histopathological study.31,32
During the physical examination, a cauliflower-like mass with fistulization is inspected and it is difficult to know with certainty its identification without histopathological and imaging studies.3,4 Management with a multidisciplinary team of specialists that includes a primary care physician is important. primary surgeon, internist, imaginologist, infectologist, pathologist, plastic, oncological or urological or proctological; according to each particular case; Mainly when the growth affects other structures, in our patient the lesions were localized which allowed their removal without complications.
Providing an adequate history in the medical history plays a vital role in determining the cause; mainly in immunocompromised or pregnant patients.33–35 There is controversy about the approach and treatment to reduce morbidity and improve results, there is a 68% risk of recurrence, patient education should be emphasized on the constant use of condoms, circumcision and vaccination against the papillomavirus. Human as possible preventive strategies against derived injuries;22,23 Our patient was given information about safe sex and HPV vaccination was proposed to his children.
Buschke-Löwenstein tumor is a rare lesion that is considered a non-malignant disease, although it has a local destructive character. The treatment of choice is surgical resection of the tumor. Currently it is considered a squamous cell carcinoma of low malignancy, locally invasive, which is why it sometimes shows aggressive behavior and accelerated growth with complications such as bleeding, fistula and infection.
None.
None.
The authors declare no conflict of interest.

©2023 Vargas-Aguilar, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.