eISSN: 2377-4304


Review Article Volume 12 Issue 6
Gynecologist Oncologist/Medicine Reproductive, President of the Mexican College of Gynecologists Oncologists, Mexican Academy Of Surgery, National Academy of Medicine of Mexico
Correspondence: Victor Manuel Vargas-Hernandez, Gynecologist Oncologist/Medicine Reproductive, President of the Mexican College of Gynecologists Oncologists, Mexican Academy Of Surgery, National Academy of Medicine of Mexico, Tel 5552179782, Fax 5511078738
Received: September 27, 2021 | Published: November 8, 2021
Citation: Vargas-Hernandez VM. Genital tuberculosis in women, its complications and infertility. Obstet Gynecol Int J. 2021;12(6):352-358. DOI: 10.15406/ogij.2021.12.00605
Tuberculosis (TB) remains a major global public health problem with the highest death rate from any infection causing 1.5 million deaths in 2018. Pulmonary tuberculosis is the most common presentation; extrapulmonary and genital tuberculosis are the second most common presentation with an increase in women of reproductive age.
The symptoms of tuberculosis are nonspecific; furthermore, the microbiological tests available for diagnosis have low sensitivity; that cause a delay in diagnosis and treatment, causing irreversible organic damage that causes infertility in women, in some cases surgery is necessary; since it can simulate oncological processes, particularly ovarian cancer; that must be discarded before starting its management. Treatment with multiple anti-tuberculosis drugs lasts for a total of 6 months, the response is clinically evaluated after one month with imaging, Treatment of tuberculosis is prolonged, generally, its total duration is 6 months with the new anti-tuberculosis drugs and its response is evaluated clinically and by imaging. The epidemiology, symptoms, complications, such as infertility, its diagnosis and treatment are reviewed.
Keywords: molecular tests, complications, infertility, imaging, surgery, anti-tuberculosis
The word tuberculosis (TB) was used for the first time in 1834; it is considered a communicable and important disease worldwide; its incidence has been decreasing in developed countries; However, it continues to be one of the main causes of mortality and morbidity worldwide; in emerging countries, where human immunodeficiency virus (HIV) infection is high, incidence, morbidity and mortality; female genital tuberculosis is often discovered incidentally and is asymptomatic; 8 to 9.2 million cases and 1.2 to 1.5 million deaths from tuberculosis are reported worldwide.1–3 Most cases of tuberculosis are reported in Asia (59%) and Africa (26%), it is less frequent in the Eastern Mediterranean (7%), Europe (5%) and North America (3%); only India reports 2 to 2.5 million or (26%) of the world incidence, China reports 0.9 to 1.2 million, South Africa 0.4 to 0.59 million, Indonesia 0.37 to 0.54 million and Pakistan 0.33 to 0.48; only India and China accounted for 38% of the global incidence. It is necessary to develop rapid, sensitive, specific diagnostic tests for timely and effective treatment in less time; nucleic acid amplification-based molecular tests (NAAT) in the early and specific diagnosis of the agent Mycobacterium tuberculosis that causes tuberculosis, which is a preventable and curable infection if diagnosed early.4–6
Pathology
When tuberculosis bacilli infect a susceptible host, the initial reaction is a polymorphonuclear inflammatory exudate. Within 48 hours, it is replaced by mononuclear cells, which become the main sites for intracellular tuber replication. As cellular immunity develops, tuberculosis bacilli are destroyed and caseous necrosis occurs,7,8 Figure 1.
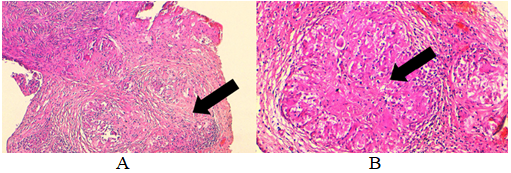
Figure 1 A. Histological section showing ovarian parenchyma with granulomatous lesions and caseous necrosis (arrow) (H&E×100). B. Shown at higher magnification, tuberculosis granulomas include (arrow) (H&E×200).
The subsequent reactivation of a focus of infection results in a proliferative granulomatous lesion, with central caseous necrosis surrounded by concentric layers of epithelial and giant cells, peripheral lymphocytes, monocytes and fibroblasts.8 In pulmonary TB, 50% of patients, when TB is miliary, the symptoms that occur are dyspnea, cough and rales, with hypoxemia, pleural pain, accompanied by pleural rubbing, a rare cause of acute respiratory failure and respiratory distress syndrome in Adults.
Patients with lymphatic TB usually present signs and symptoms referring to the site of the disease, although constitutional symptoms are the only discomfort. Suspected joint TB presents with bone pain (including back pain) with or without focal edema or fever. The clinical course is indolent and only pain is the first symptom. Forms of gastrointestinal involvement include liver disease, enteritis, and tuberculous peritonitis; or as pancreatitis or cholecystitis.9,10 In the central nervous system, with meningitis or tuberculoma, in 15 to 20% and 33 to 54% respectively, the diagnostic suspicion and nonspecific clinical findings: such as headache, low fever and / or focal neurological findings. Tuberculosis of the urinary tract presents with hematuria, proteinuria and sterile pyuria.9,11 Urinary tract tuberculosis presents with hematuria, proteinuria, and sterile pyuria;9,11 The development of Addison's disease or tuberculous heart disease is rare, 12% that presents mainly as pericarditis, and its diagnosis is generally late. In the skin and mammary gland, they are rare9,12 It presents clinically as a solitary hard nodule, poorly defined, unilateral, with nipple discharge, thickening of the skin or lymph nodes in the armpit, clinically and radiographically simulating breast cancer or abscess, generalized spread is by the hematogenous route Figure 2.7,9
Pelvic TB can exist as tuberculous adenitis, in mesenteric or pelvic lymph nodes, without involvement of the genital tract. Generalized miliary peritoneal TB, the tubercles embedded in the abdomen, involving the serous surface, abdominal and pelvic organs without penetrating the mucosa, do not usually affect reproductive function and is different from genital TB.8 Genital TB is rare; but, it is greater, in communities where pulmonary forms or other forms of extragenital TB are common; affects any organ of the body, without clinical manifestations and reactivates, is a public health problem and responsible for infertility. The true incidence of genital TB is not known, and it is diagnosed in 5% of women in infertility study.5,6,8,9 The clinical diagnosis of genital TB is suspected in 20% of patients with a positive Combe sign; or history of primary infertility that is an apparent cause of poor general health for months or years associated with weight loss, excessive fatigue, low-grade fever or pelvic-abdominal discomfort, including extra-genital TB in 30-50% who present systemic symptoms.
Genital tuberculosis is transmitted by direct inoculation during sexual intercourse; ascent and spread of the tuber to the vagina, cervix and vulva, 80% have a history of extragenital tuberculosis, Table 1.4
Systemic |
Weight loss |
Fatigue |
|
Mild temperature (low fever) |
|
Sterility |
Primary |
Secondary |
|
Menstrual disorders |
Amenorrhea |
oligomenorrhea |
|
Proiomenorrhea |
|
Symptoms Pelvic Abdominal |
Inflammation |
Postcoital hemorrhage |
|
Vaginal discharge |
|
Dyspareunia |
Table 1 Symptomatology of genital tuberculosis in women
The common initial symptom in women with undiagnosed tuberculosis is infertility in 15%, of them 85% never got pregnant, or they develop tuberculosis one year after the last pregnancy, in 40-50% and chronic pelvic-abdominal pain in these women with TB is frequent from 25 to 50%; before arriving for the consultation; it is usually not serious and is accompanied by abdominal distension, with episodes of acute pelvic pain due to a secondary infection by pyogenic bacteria. When it progresses, pelvic pain is aggravated, particularly with intercourse, exercise, and menstruation, and later menstrual disturbances are common in 10 to 40%; you probably have normal menstrual cycles and the secretory endometrium is common. Tuberculous endometritis does not interfere with the menstrual cycle due to hormonal stimulation; ovarian failure is not the cause of amenorrhea; it is secondary to the caseous endometrium. Other less frequent symptoms are leucorrhoea, fistulas; It can even simulate or mimic ovarian cancer by presenting with adnexal masses and ascites, elevated serum levels of CA-125 that are only diagnosed after surgery in the histopathological study; physical examination is normal in 50% and only adnexal masses or ascites are palpated;5,6,8 that do not present a correlation between symptoms and findings on physical examination in 35-50% of cases. The fallopian tubes or tuberculous ovarian masses are less painful than those due to a pyogenic infection are, although secondary infection and acute exacerbation can produce an acute abdomen. Other benign or malignant pelvic lesions can coexist with genital TB, Table 2.
Physical signs in genital tuberculosis |
Normal |
Abdominal mass |
Pelvic mass |
Adnexal mass |
Abdominal tenderness |
Pelvic / adnexal tenderness |
Ascites |
Excessive vaginal discharge |
Ulcer on the vulva, vagina, and cervix |
Enlarged uterus with pyometra |
Fistulas |
Table 2 Physical signs in genital tuberculosis
Adnexal masses vary in size and consistency or conglomerate with frozen pelvis due to adhesions, or ovarian tube abscess; fever over 38°C occurs in one third; Acute bacterial infections, surgery, or trauma reactivate latent pelvic tuberculosis.5,6,8 Genital TB is transmitted by direct inoculation during sexual intercourse; ascent and spread of the tuber to the vagina, cervix and vulva, 80% have a history of extragenital TB.
The possibility of primary sexual transmission is not excluded; after primary or secondary infection, the uterine tubas are affected in 95-100%, the endometrium 50-60%, ovaries, 20-30%, cervix 5-15%, vulva / vagina 1% and myometrium, 2.5 %; Cervical TB simulates cervical cancer and only the biopsy rules it out.8,9,13 Adhesions in the tubas, ovaries, omentum, intestine, liver and diaphragm (Fitz Hugh Curtis syndrome); they are common findings. Advances in the medical treatment of TB, pregnancy and live birth after genital TB diagnosis is low and when achieved it is more likely to be an ectopic pregnancy or spontaneous abortion, Table 3.8
Organ |
Frequency (%) |
Uterine Tubas |
90–100 |
Endometrium |
50–60 |
Ovary o |
20–30 |
Cervix |
5–15 |
Vulva and vagina |
1 |
Table 3 Frequency of tuberculosis in genital organs
In 25-50% the tubas remain with recognizable fimbriae, with the appearance of a tobacco bag; granulomas and a chronic inflammatory infiltrate affect the entire thickness of the tubal wall, and caseous necrosis is common in advanced cases. Adnexal masses vary in size and consistency, forming conglomerates that lead to the development of a frozen pelvis due to adhesions or abscesses of the fallopian tubes with the ovary; they present a fever higher than 38°C in a third of these cases. Acute bacterial infections, surgery, or trauma reactivates latent pelvic TB.5,6,8 Genital tuberculosis is transmitted by direct inoculation during sexual intercourse; ascent and spread of the tubercle to the vagina, cervix and vulva, 80% have a history of extragenital tuberculosis. Cervical TB simulates cervical cancer and only the biopsy rules it out.8,9,13
In 25-50% the tubas remain with recognizable fimbriae, with the appearance of a tobacco bag; granulomas and a chronic inflammatory infiltrate affect the TB of the endometrium, size and shape of the uterus are normal. The tuberculous process is generally located in the endometrium, is more extensive in the fundus and decreases towards the cervix. The myometrium is not usually involved, in 2.5% of cases of tuberculous endometritis, there is total destruction of the endometrium and secondary amenorrhea and pyometra in case of internal occlusion; in advanced cases fibrosis, calcification and caseous necrosis are formed; they are rarely observed during the reproductive period due to regular cyclical menstruation. The classic lesion in tuberculous endometritis is non-caseating granuloma, composed of epithelial cells, giant Langhans cells and lymphocytes; it is located along the endometrium with greater density in the superficial layers. Granulomatous lesions are identified on cycle days 24-26 or within 12 hours of menstruation.8,10,14,15
Ovarian TB is affected in 11 to 30%, it is generally bilateral where the ovaries are attached to each other and the fallopian thrombi and uterus, which are surrounded or forming a complex mass attached to the pelvic structures such as peritoneum, intestines, covered by tubercles caused by direct spread or hematogenous spread; where a caseating granuloma occurs within the parenchyma.5,8
The TB of the vulva and vagina occurs in 2%. In the vulva, it begins as a nodule on the lips or vestibular region, which forms an irregular ulcer with holes that discharge cheesy material and pus. In the Bartholini gland it presents as an irregular hypertrophic growth. A tuberculous lesion in the vagina mimics a gross carcinoma. The microscopic appearance is granulomatous inflammation that tends to cause central caseation and an associated chronic inflammatory infiltrate.5,6,8,16,17
Tuberculous peritonitis is observed in combination with female genital TB in 45%. In peritonitis, an associated pleural effusion is not uncommon; most do not present parenchymal abnormalities on chest radiography;8,12,13–22 Endometrial sampling is recommended for histological and microbiological examination to make the diagnosis of genital TB, it is useful if granulomas are found or, if smears or cultures are positive for TB. Laparoscopy with targeted biopsies of suspicious areas may be helpful if less invasive methods do not provide the necessary diagnostic information.
Hysterosalpingography is contraindicated in the presence of recent acute pelvic TB, the exacerbation may reactivate pelvic TB; but reveals certain abnormalities that suggest the possibility of pelvic TB. The uterine cavity is deformed, with associated intrauterine adhesions and lymphatic extravasation,7 Figure 3.
Abdominal and transvaginal ultrasound demonstrates the presence of ascites; Bilateral adnexal masses that are predominantly solid and when performed laparoscopy in 14.7%, pelvic TB is suspected,15,23–29 Figure 4.
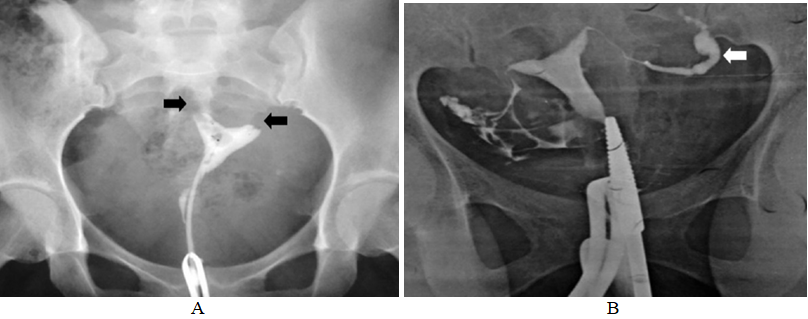
Figure 3 A. Histerosalpingography showing bilateral tubal blockage (arrows). B. Hysterosalpingogram showing left hydrosalpinx with fimbrial block (arrow).

Figure 4 A. Laparoscopy showing the presence of adhesion in the genital organs such as the uterus (large arrow), fallopian tubes (medium arrow) and ovaries (small arrow) B. Laparoscopy showing bilateral hydrosalpinx, tuberous masses ovarian, adhesions (large arrow) and frozen pelvis (small arrow).
On ultrasound, the fallopian tubes may appear dilated, thickened, and filled with clear fluid called hydrosalpinx or thick material called pyosalpinx; in women with genital TB, the endometrium is affected in 50–90%, and uterine enlargement may be due to filling with caseous material.29
The endometrium may appear heterogeneous with hyperechoic areas representing foci of calcification or fibrosis, intrauterine adhesions, and a distorted uterine cavity. Findings can range from a normal examination to abnormalities such as thin or thickened endometrium, cornual obliteration, impaired endometrial vascularization during mid-cycle in stimulated menstrual cycles, sub-endometrial calcification, variation in uterine artery flow during mid-cycle, tubal fluid, free, and loculated peritoneal fluid, heterogeneous ovarian enlargement and adnexal fixation. Ultrasound reveals multiple echogenic lesions with surrounding hypoechoic halos.9
Molecular methods are complementary for the identification of TB; with the polymerase chain reaction (PCR), the diagnosis is in a few days or hours with sensitivities of 47 to 100%, the amplification techniques can be used for broth cultures in the detection of growth as soon as possible. Under these conditions, the diagnosis is obtained in 7-10 days with a sensitivity and specificity of 100%; Several nucleic acid amplification techniques (NAAT) allow the detection of TB, identify it directly, allow early identification, and management decisions,8–14,18–22,30–34 Table 4.
Complete blood count of Mycobacterium tuberculosis |
Endoscopy |
|
Chest X-rays |
Liquid Culture of Ascites |
Laparoscopy |
Tuberculin test |
Peritoneal biopsy for culture |
Cystoscopy |
Menstrual blood culture |
Hysterosalpingography |
Hysteroscopy |
Endometrial curettage |
Ultrasonography |
|
Histopathological examination |
Cervical cytology |
|
Table 4 Tests to confirm diagnosis of genital TB
On ultrasound, the fallopian tubes may appear dilated, thickened, and filled with clear fluid called hydrosalpinx or thick material called pyosalpinx; in women with genital TB, the endometrium is affected in 50–90%, and uterine enlargement may be due to filling with caseous material.29
The endometrium may appear heterogeneous with hyperechoic areas representing foci of calcification or fibrosis, intrauterine adhesions, and a distorted uterine cavity. Findings can range from a normal examination to abnormalities such as thin or thickened endometrium, cornual obliteration, impaired endometrial vascularization during mid-cycle in stimulated menstrual cycles, sub-endometrial calcification, variation in uterine artery flow during mid-cycle, tubal fluid, free, and loculated peritoneal fluid, heterogeneous ovarian enlargement and adnexal fixation. Ultrasound reveals multiple echogenic lesions with surrounding hypoechoic halos.9
Molecular methods are complementary for the identification of TB; with the polymerase chain reaction (PCR), the diagnosis is in a few days or hours with sensitivities of 47 to 100%, the amplification techniques can be used for broth cultures in the detection of growth as soon as possible. Under these conditions, the diagnosis is obtained in 7-10 days with a sensitivity and specificity of 100%; Several nucleic acid amplification techniques (NAAT) allow the detection of TB, identify it directly, allow early identification, and management decisions,8–14,18–22,30–34 Table 4.
Diagnosis of latent tuberculosis infection
The denatured protein derivative has great limitations; low sensitivity, false positives or negatives, principalmente en personas infectadas por HIV, corticosteroid therapy, chronic kidney failure, malnutrition, cancer or a serious illness.30,33,37–42
Diagnosis of active tuberculosis
It is based on clinical suspicion, imaging with chest radiography, computed tomography (CT) and, more recently, positron emission tomography (PET) have been used for surveillance and microbiological with bacterial culture and molecular methods such as tests of NAAT nucleic acid amplification. Hematological abnormalities are prominent with normochromic normocytic anemia observed in half of patients, hypercalcemia is rare. Sterile pyuria was found in 32%, negative urine cultures, may be positive for miliary TB.9,40
Imaging
More than two-thirds have a chest radiograph with a miliary pattern, when the miliary nodules are large enough. Other abnormalities include pleural reactions, hilar or mediastinal adenopathy, and evidence of active or healed parenchymal TB (infiltrates or interstitial or alveolar cavities).9 High-resolution computed tomography of the chest is more sensitive. Numerous nodules of 2 to 3mm are seen distributed throughout the lung. Contrast abdominal computed tomography can demonstrate multiple low-attenuation foci, typically without enhancement after contrast administration, Figures 5–8.9,39–44

Figure 5 Diagnostic algorithm for female genital tuberculosis (FGTB). PID, pelvic inflammatory disease; ESR: erythrocyte sedimentation rate; TST, tuberculin skin test; AFB, acid fast bacilli; NAAT, nucleic acid amplification test; PCR, polymerase chain reaction.

Figure 6 CT image (coronal section) showing A: right tube-ovarian mass, B: pelvic collection, C: mesenteric lymph nodes and D: free abdominal fluid.

Figure 7 A. Computed tomography (cross section) showing, A: right tube-ovarian mass and B: pelvic collection; B. Computed tomography (cross section) showing A: intestinal edema.
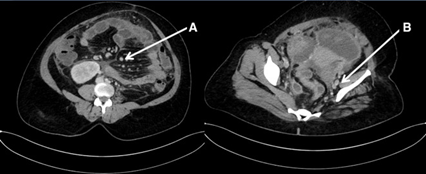
Figure 8 Computed tomography (cross section) showing A: mesenteric lymph nodes and B: pelvic lymph nodes.
Differential diagnosis of tuberculosis
It is broad and depends on the degree of dissemination and involvement of specific tissues and organs; from disorders of the respiratory tract (such as inhalation diseases) or lymphatic processes (sarcoidosis). A miliary pattern on chest X-ray is due to many conditions, including histoplasmosis. Pulmonary manifestations can include pneumonia, adenopathy, lung mass, pulmonary nodule and / or cavitary lung disease.8,9,35
Management of tuberculosis
The treatment of tuberculosis is used the same antituberculous drugs for pulmonary or genital TB; with individualization of the case, surgery may be necessary for diagnostic and / or therapeutic management. In some circumstances, corticosteroids are used for the treatment of tuberculosis involving the CNS or pericardium.8,9 To plan an effective treatment, check if there is an active extragenital focus; extension of Tb in the genital tract; assess whether medical treatment will cure genital TB; if surgery is necessary; assess the possibility of pregnancy after treatment. The extent of the genital lesion is divided into minimal and advanced. Minimal genital Tb is usually asymptomatic, except for sterility. In advanced genital TB, Tubo-ovarian masses are present. Before effective antiphymic medical treatment, surgery was the basis of treatment and postoperative complications were high, such as intestinal fistula (14%) and mortality (2.2%), anti-tuberculosis drugs are effective before surgery,8,9,38,43,45 the schemes with:
Treated genital TB patients should have a long, close follow-up. Recurrence or spread to other organs is rare, it occurs occasionally, surgery is recommended in the following indications; persistent and recurrent disease despite proper treatment; persistent or recurrent pelvic masses after 6 months of adequate treatment; persistent or recurring symptoms such as chronic pelvic pain and abnormal genital bleeding; persistent fistula that does not heal; multidrug-resistant disease; concomitant neoplasm of the genital tract or other pathology, the patient should receive it at least 1-2 weeks before the operation. In patients with minimal genital tuberculosis, no evidence of active TB was found in the tubas after 10 months of treatment. For advanced disease, surgery followed by anti-tuberculosis therapy was advised.11
Surgery is performed mid-cycle in premenopausal patients, and continues for 6-12 months, anti-tubersulose after surgery, and morbidity and mortality are significantly reduced; late complications are rare. The surgery of choice is total abdominal hysterectomy with bilateral salpingo-oopherectomy followed by hormone replacement therapy, especially in a premenopausal woman. If the patient is premenopausal and the ovaries appear normal, they can be preserved, successful pregnancies are reported by early treatment, the patient has a 50% chance of conceiving and achieving a newborn; Although pregnancy can follow a proven minimal TB, patients with advanced disease should be considered infertile, pregnancy after a diagnosis of genital TB is rare. With early diagnosis and appropriate therapy, a more favorable outcome can be expected; the post-treatment fertility rate is 6.7%.11 Tubal surgery has a poor prognosis and only in women with genital TB, in vitro fertilization (IVF) with embryo transfer (ET) (*** MEANING) is the option to achieve pregnancy. Perinatal morbidity is similar in pregnant women without genital TB, when treatment is timely. Extrapulmonary tuberculosis lesions other than lymphatic adenitis are associated with adverse outcomes after pregnancy and delivery. Mycobacterium tuberculosis infection during pregnancy represents a risk of maternal and neonatal complications, and the incidence of preterm delivery, perinatal death, and low birth weight is higher. Vaccination in childhood with Bacillus Calmette-Guérin (BCG) in endemic areas reduces the incidence of TB, with 78% protection.12 TB decreased with isoniazid-based combination therapy (5%). Age, late presentation, severe underlying disease, and nonreactive tuberculin skin test are predictors of mortality.11
Comments
Tuberculosis (TB) represents a higher mortality rate than any infectious disease, causing 1.5 million deaths in 2018 and 10 million people develop active TB annually with 1.33 million deaths from it.46 Pulmonary TB remains the most common presentation and extrapulmonary TB, female genital TB is the second most common presentation; mainly in emerging countries that is reported from 5 to 21%,35 affecting mainly women of reproductive age worldwide;28 tuberculosis spreads from the lungs to other organs through the lymphatic, hematogenous, or directly to adjacent organs. It can be sexually transmitted from a sexual partner with active genital TB; infection with immunodeficiency virus and the current COVID-19 pandemic worsens the clinical outcomes of TB by impeding the immune response of the host.26,29,46
Genital TB can present with infertility, menstrual problems, unexplained abdominal pain, or a pelvic mass. Patients present with systemic symptoms of fever, weight loss, and night sweats. Ectopic pregnancy and cervical/vulvar lesions are rare presenting features. A postmenopausal woman with vaginal bleeding should also be evaluated. Rare presentations of genital TB include a cervical growth that mimics carcinoma of the cervix, vulvar and vaginal ulcers; TB treatment should be started only after confirmation with microbiology, histopathology, or laparoscopic appearance suggestive of TB.35 Laparoscopy plays an important role for the diagnosis of genital TB with the presence of tubercles in the peritoneum, Tubo-ovarian mass, caseous nodules, cystic ascites, pelvic adhesions, hydrosalpinx, appearance of a tobacco bag in the tube and tubes with beads.9,19,47,48 The fertility outcome is poor in female genital TB, IVF-ET can be performed for tubal blockage with normal endometrium with a good result. Surrogacy may be recommended in case of damaged endometrium and adoption if the ovaries are damaged. Newer vaccines, diagnostics and drugs (such as bedaquiline, delamanid) and stem cell therapy are being developed and tested.13,15,26,27,29,47,51–53
Tb continues to be a public health problem in emerging countries and genital TB is responsible for infertility; Sometimes it simulates cancer of the genital tract, and its diagnosis is challenging, the true incidence is not known, due to its asymptomatic presentation and many cases are not diagnosed. Early medical management improves the prognosis of the woman and in the demonstrated minimum TB; pregnancy can be achieved, unlike the advanced who are infertile and occasionally require surgery. Genital tuberculosis is one of the main causes of infertility in women Most patients present in an advanced stage with scarring, severe fibrosis, and adhesions, and the results of treatment, especially with regard to infertility, are poor. Therefore, early diagnosis and correct treatment are vital to avoid complications and restore fertility.
None.
None.
The authors did not report any potential conflicts of interest.

©2021 Vargas-Hernandez. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.