eISSN: 2377-4304


Commentary Volume 5 Issue 4
1St. George's University Hospitals NHS Foundation Trust, UK
2Kingston Hospital NHS Foundation Trust, UK
Correspondence: Edwin Chandraharan, Consultant Obstetrician and Gynaecologist/ Lead Clinician Labour Ward, St. George's University Hospitals NHS Foundation Trust & Honorary Senior Lecturer, St George's University of London, Blackshaw Road, London SW17 0QT. UK, Tel 00442087252022, Fax 00442087251975
Received: October 18, 2016 | Published: November 8, 2016
Citation: Chandraharan E, El Tahan M, Pereira S. Each fetus matters: an urgent paradigm shift is needed to move away from the rigid “CTG guideline stickers” so as to individualize intrapartum fetal heart rate monitoring and to improve perinatal outcomes. Obstet Gynecol Int J. 2016;5(4):376-379. DOI: 10.15406/ogij.2016.05.00168
Current guidelines on intrapartum fetal heart rate monitoring stipulate arbitrary ranges for baseline fetal heart rate and variability which are, very unfortunately, being applied for every fetus, irrespective of the gestational age, wider clinical context (i.e. presence of meconium staining of amniotic fluid, ongoing chorioamnionitis etc.,) as well as their individual physiological reserve (i.e. growth restriction, exposed to metabolic disorders such as maternal gestational diabetes mellitus etc).
Various “CTG Stickers” (Figure 1) are being used during intrapartum care to facilitate CTG interpretation during labour. However, such “CTG Stickers” may lead to the blind classification of the fetus into “normal, suspicious and pathological” without considering the gestational age of the fetus as well as the wider clinical picture (presence of meconium staining of amniotic fluid, ongoing chorioamnionitis and growth restriction).
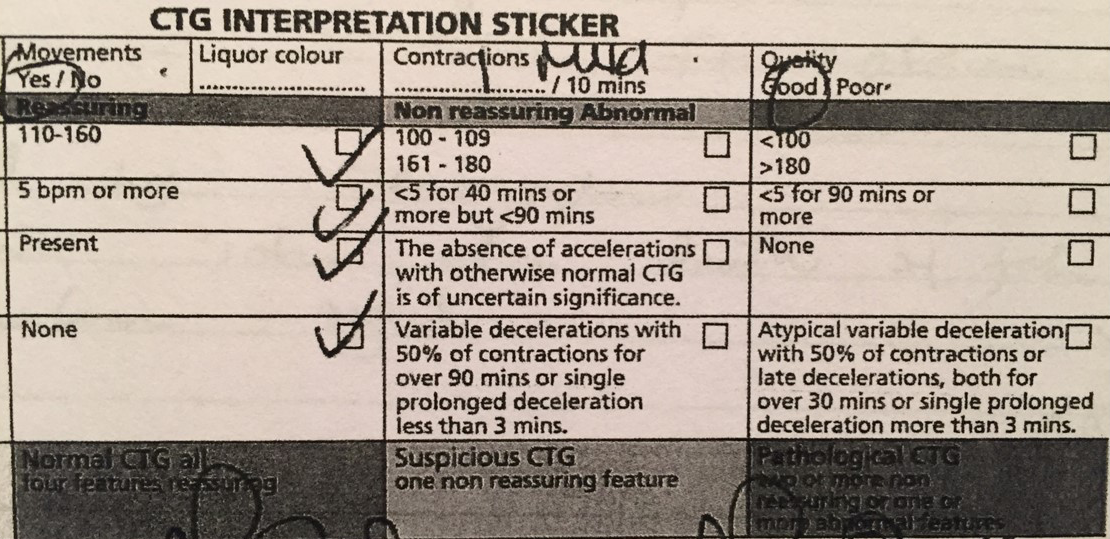
Figure 1‘CTG Guideline Box’ based on ‘National Institute of Health and Care Excellence (NICE) Guidelines used in labour wards in the UK for all babies in labour.
It is vital to remember that the normal ranges proposed by the guidelines are derived for the human population of fetuses and not the individual fetus in question. This is similar to the normal range of adult heart rate of 60-90 beats per minute (bpm): one would not consider if the heart rate of an individual adult goes up from 61 bpm to 89 bpm as normal for the individual adult, even though it is still within the normal range of 60-90 bpm. Conversely, if an individual’s heart rate increases from 88 bpm to 92 bpm, one would not consider this as abnormal, even though it is outside the normal range of 60-90 bpm.
Failure to individualize the features of Cardiotocograph (CTG) trace during labour may lead to missing a fetus exposed to pre-existing (i.e. chronic) hypoxia, chorioamnionitis or catecholamine surge during labour, all of which would alter the baseline fetal heart rate. This may lead to poor neonatal outcomes such as neonatal encephalopathy (hypoxic or inflammatory) or intrapartum or an early neonatal death. Conversely, over-reaction to the features which are ‘outside the guideline’ but are normal for the individual fetus (e.g. prematurity or post-maturity) may lead to unnecessary operative interventions during labour such as fetal blood sampling (FBS), emergency caesarean sections and operative vaginal births
Baseline fetal heart rate
The normal baseline fetal heart rate for a term fetus (i.e. from 36 completed weeks to 41 completed weeks) lies between 110 bpm and 160 bpm and it reflects the metabolic needs of the fetus in question at the given time, modified by the autonomic nervous system: the sympathetic nervous system attempts to increase the fetal heart rate acting vi the sino-atrial (SA) node and the para-sympathetic system attempting to decrease the heart rate acting via the atrio-ventricular (AV) node of the heart.1 A stable baseline fetal heart rate indicates positive myocardial energy balance and ongoing aerobic metabolism. Conversely, an ‘unstable’ or a ‘wavy’ baseline fetal heart rate indicates inability of the fetal myocardium to continue pumping at the given rate secondary to the onset of myocardial decompensation and resultant metabolic acidosis or due to electrical malfunction (i.e. arrhythmias).
A preterm fetus may have a baseline fetal heart rate above the upper limit of the normal range (i.e. >160 bpm) and this is entirely normal (Figure 2). This is because of the late development and maturity of the parasympathetic component of the autonomic system, which becomes gradually predominant after 34 weeks of gestation.2 Similarly, repetitive variable decelerations may occur due to the lack of Wharton’s Jelly protecting the umbilical cord leading to cord compression (Figure 2). Therefore, a higher baseline fetal heart rate observed in a pre-term fetus, in the absence of other non-reassuring features (atypical variable or late decelerations and changes in baseline variability) does not need any intervention. Similarly, a fetus beyond 40 weeks of gestation would be expected to have a lower baseline fetal heart rate secondary to vagal dominance. This may result in the baseline fetal heart rate outside the lower limit of normal (i.e. <110 bpm).3 This is entirely normal for the post-term fetus in question and does not need any intervention, if other parameters (i.e. atypical variable or late decelerations or changes in baseline variability) are absent. Conversely, a post-term fetus displaying a baseline fetal heart rate closer to or above the upper range of normal (i.e. 160 bpm) should not be considered as normal for the fetus in question (i.e. postdates) even though it may be within the range proposed by CTG guidelines. Such an increased baseline fetal heart rate which is more than that would be expected for the gestational age may be secondary to an ongoing intrauterine fetal infection or chorioamnionitis (Figure 3) or chronic hypoxia (Figure 4). Therefore, the use of “Guideline Stickers” (Figure 1) should be viewed with caution as these could give a false sense of security to clinicians caring for fetuses during labour.

Figure 2 CTG of a Preterm Fetus at 28 weeks of gestation. Although, the baseline fetal heart rate is outside the ‘Guideline Range’, it is physiological for a preterm fetus due to the immaturity of the parasympathetic system.

Figure 3 CTG trace in chorioamnionitis at term. Note the baseline fetal heart rate of 150 bpm is still within the normal range, although abnormal for a fetus at 41 weeks +3 days of gestation despite of ongoing chorioamnionitis.

Figure 4 Note a higher than expected baseline fetal heart rate for the gestational age of 40 week + 1 day, loss of baseline variability and shallow decelerations in chronic hypoxia.
In author’s (EC’s) own medicolegal practice, very unfortunately, term fetuses have been found to sustain damage or suffer an intrauterine death due to blind adherence of arbitrarily ranges proposed by national guidelines4 without considering the gestational age as well as the physiological reserves of the fetus in question (Figure 3).
Chorioamnionitis
A fetus who is exposed to an intrauterine infection resulting in inflammation and infection of the amniotic fluid and the placenta may develop congenital pneumonia as a result of inhalation of infected amniotic fluid. Release of inflammatory mediators secondary to congenital pneumonia may lead to an increase in the fetal heart rate. Considering the fact that the heart rate increases by approximately 10% for each degree rise of temperature secondary to the raised metabolic rate, a fetus may show a baseline increase in the heart rate of approximately 30 bpm for a 2°C rise of temperature at 37 weeks of gestation (i.e. 10% of 150 bpm for each degree rise of temperature) leading to a baseline fetal heart rate of approximately 180 bpm. This would be noted as outside the normal range for the baseline fetal heart rate proposed by the national guidelines.
However, if the same fetus presents four weeks later (i.e. at 41 weeks of gestation), the baseline fetal heart rate would be expected to progressively decline with the maturity of the parasympathetic component of the autonomic nervous system to approximately 110 to 120 bpm. Therefore, if the fetus acquires the same infection (i.e. chorioamnionitis) at 41 weeks of gestation, the baseline fetal heart rate would only increase to 24 bpm for a 2°C rise of temperature (i.e. 10% of 120 bpm for each degree rise of temperature). This will result in the baseline fetal heart rate rising to approximately 144 bpm, and, although, this is still within the normal range proposed by the national guidelines on CTG interpretation, the fetus is not normal but is experiencing a serious intrauterine infection.
Evolving hypoxia
The fetus who is exposed to evolving hypoxia would compensate by reducing the myocardial workload (i.e. decelerations) to maintain an aerobic metabolism within the myocardium and restriction of non-essential body movements (i.e. loss of accelerations).4 However, continuation of the hypoxic stress (repetitive umbilical cord compression or a reduction in the utero-placental circulation) would result in release of catecholamines (adrenaline and noradrenaline) so as to compensate for the hypoxic stress. The catecholamines not only increase the baseline fetal heart rate but also cause peripheral vasoconstriction to divert oxygenated blood from non-essential to essential organs (i.e. centralisation), increase systemic blood pressure secondary to increased peripheral vascular resistance as well as provide additional energy substrate wire glycogen arises.
A post-term fetus with a baseline fetal heart rate of 110 bpm may not mount sufficient catecholamine surge to go beyond the upper limit of the proposed normal guideline range (i.e.> 160 bpm). Therefore, blind adherence to the normal range proposed by national guidelines on CTG interpretation may lead to the failure in the recognition of such a fetus exposed to a persistent catecholamine surge which may undergo decompensation with continuation of hypoxia. Therefore, it is not only the absolute value of the baseline heart rate that is important but also, the changes in the baseline fetal heart rate over a period of time which indicate a catecholamine surge secondary to evolving hypoxia or an ongoing evolving intrauterine infection (i.e. chorioamnionitis). Use of the current “Guideline Stickers” would lead to the failure recognition of a fetus exposed to an intense catecholamine surge which has increased its baseline fetal heart rate from 110 bpm to 155 bpm, despite still within the normal range (i.e. 110 to 160 bpm).
Intrauterine Fetal Growth Restriction (IUGR)
A fetus who is growth restricted at term may not have sufficient physiology reserves to mount a successful and sustained response to ongoing intrapartum hypoxic stress. Due to the smaller size of the internal organs secondary to intrauterine growth restriction, which include smaller adrenal glands, the baseline fetal heart rate may not increase to 160 bpm in a fetus with IUGR so as to cross the upper limit of the proposed normal range (110 to 160 bpm) by the national guidelines. A blind adherence to the “CTG Guideline Sticker” would lead to the failure of recognition of an IUGR fetus mounting the very best catecholamine response that it is capable of doing so, and yet, being unable to cross the upper limit (i.e. more than 160 bpm) proposed by the national guidelines on CTG interpretation. In addition, arbitrary time limits proposed by national guidelines on CTG interpretation (i.e. atypical or late decelerations lasting for 50% of contractions were 30 minutes or typical variable decelerations lasting for 50% contractions 90 minutes) should be applied with caution in a fetus with IUGR. In adult cardiology, such arbitrary time limits are not applied for individuals undergoing cardiac stress test. This is because based on the individual reserve, the ST segment changes would be observed a different time in different adults. Similarly, a growth restricted fetus (IUGR) would not be expected to have the same physiological reserve as the term well grown fetus to withstand ongoing hypoxic stress for 30 or 90 minutes as proposed by the guidelines.5
Pre-existing (or chronic) hypoxia
A fetus who is exposed to a pre-existing or chronic hypoxia secondary to an ongoing chronic utero-placental insufficiency may have already attempted to protect its vital organs by a sustained release of catecholamines during the antenatal period. Therefore, the baseline fetal heart rate would be in the upper limit of the normal range proposed by the National Guidelines. However, the fetus in question exposed to chronic hypoxia would not be able to withstand continuation of labour because with the onset of uterine contraction and resultant repetitive and sustained compression of the umbilical cord as well as reduction in utero-placental circulation may result in rapid fetal decompensation leading to hypoxic-ischaemic brain injury and/or an intrapartum stillbirth or an early neonatal death. Blind adherence to the “CTG Guideline Box” (Figure 1) would lead to the failure of recognition of chronic hypoxia as this fetus would not have sufficient physiology reserves to mount a further catecholamine surge so as to go about the upper limit of the guideline range (i.e.> 160 bpm).
Presence of meconium and other intrapartum risk factors
Fetal neurological injury may occur where are multiple pathways which include metabolic, inflammatory, genetic, thermal as well as hypoxic insults. Moreover, presence of other risk factors such as inflammation and pyrexia may potentiate the effects of hypoxia on the fetal brain.6,7 Scientific evidence from both animal had human studies suggests that a combination of such insults can significantly increase fetal neurological injury.6,7 Therefore, the same “CTG Guideline Box” should not be applied blindly to a fetus exposed to additional risk factors during labour as it would result in missing a serious neurological injury due to a combination of risk factors acting together and potentiating the magnitude of fetal brain injury. Increase in the baseline fetal heart rate is associated with doubling the risk of fetal meconium aspiration syndrome.8
In the author’s medicolegal practice, very unfortunately, failure to ensure individualized care for fetuses in labour and the blind application of the “CTG Guideline Box” in every fetus during labour without considering the gestational age and the wider clinical picture has resulted in poor neonatal outcomes which include hypoxic-ischaemic brain injury, intrapartum stillbirth and early neonatal death as well as long-term neurological sequelae such as cerebral palsy. Recent publication by the Royal College of obstetricians and Gynaecologists (RCOG) titled “Each Baby Counts” has confirmed that out of 921 babies who had poor perinatal outcomes, 199 suffered an intrapartum stillbirth, 147 had an early neonatal death and 655 babies had a severe brain injury in 2015.9 Blind adherence to clinical guidelines and the use of “CTG Guideline Stickers” in every fetus should be actively discouraged and should be eliminated to improve perinatal outcomes. Similar to adults, each fetus is different with individual physiological reserves and risk factors and therefore, they should be treated differently during labour.
Each fetus has a different baseline fetal heart rate in accordance with the gestational age and to meet their metabolic needs at the given time. They also have different risk factors (i.e. presence of meconium staining of amniotic fluid, ongoing chorioamnionitis, maternal gestational diabetes which increases the risk of fetal acidosis and reduced placental perfusion) and therefore, it is nonsensical the use a single “CTG Guideline Sticker” in every fetus and used the same arbitrary cut-offs for the baseline fetal heart rate as well as duration of decelerations.
Albert Einstein stated that “insanity is repeating the same processes again and again and expecting different results”. During intrapartum care, insanity, in our opinion, is “the use of the same “CTG Guideline Sticker” in every fetus, irrespective of the gestational age and wider clinical picture, and expecting a good perinatal outcome. It is time to start the switch on the “Thinking Box” and stop the application of the same “CTG Guideline Box” on every fetus and to treat each fetus as its own control. Each fetus matters and deserves such an individualised care during labour.
None.
None.

©2016 Chandraharan, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.