eISSN: 2377-4304


Case Report Volume 10 Issue 4
1Muneta Maternity Clinic, Chiba, Japan
2Japan Low Carbohydrate Diet Promotion Association (JLCDPA), Kyoto, Japan
3Tokushima University/Medical Research, Tokushima, Japan
4Takao Hospital, Kyoto, Japan
Correspondence: Hiroshi Bando, MD, PhD, FACP, Tokushima University/Medical Research, Nakashowa 1-61, Tokushima 770-0943 Japan, Tel 81-90-3187-2485
Received: August 22, 2019 | Published: August 28, 2019
Citation: Muneta T, Kawaguchi E, Hayashi M et al. Clinical effect for diabetic pregnant female by Low Carbohydrate Diet (LCD) and Continuous Glucose Monitoring (CGM). Obstet Gynecol Int J. 2019;10(4):326-329. DOI: 10.15406/ogij.2019.10.00461
In the diabetic medical practice, continuous glucose monitoring (CGM) has been recently used with beneficial efficacy. Authors have continued women’s medical care and research on Calorie Restriction (CR) and Low Carbohydrate Diet (LCD), and developed medical and social LCD movement by Japan LCD Promotion Association (JLCDPA). In this study, a diabetic female case with remarkable improving effect is shown using CGM and LCD. The case is 27 years-old female with type 2 diabetes mellitus (T2DM). She has been pregnant and on multiple daily insulin injection (MDI) with insulin 48 units/day in the university hospital. She was on this treatment until 28th weeks with no preeclampsia symptoms, and hoped to change the treatment of LCD. She came to our women’s clinic with the current data of weight 101kg, BMI 37.1 and HbA1c 7.0%. By application of FreeStyle Libre (Abbott, USA), her glucose variability showed around 160mg/dL with some episodes of hyperglycemia. The meal was changed from CR to LCD after 29th week, then insulin administration could be discontinued in 10 days. This glucose variability showed remarkable efficacy for combination of LCD and CGM. These results would become basal and reference data and contribute to the development of future research.
Keywords: continuous glucose monitoring, low carbohydrate diet, glucose variability, Japan LCD promotion association, freestyle libre, registered dietitian nutritionist
CGM, continuous glucose monitoring; LCD, low carbohydrate diet; T2DM, type 2 diabetes mellitus; CR, calorie restriction; JLCDPA, Japan LCD promotion association; MDI, multiple daily insulin injection; RDN, registered dietitian nutritionist
Across the world, the recent situation of diabetes mellitus shows the gradual increasing prevalence in developed countries and developing countries.1 Consequently, the important problem would be the adequate management and treatment for diabetes mellitus.2
For the therapeutic concept for diabetes, nutritional treatment has been the basal way of the therapy. There were a variety of dietary therapies until now, such as calorie restriction (CR), low carbohydrate diet (LCD), Mediterranean diet, high protein diet, vegetarian diet, Paleolithic diet and so on.3 Among them, CR had been formerly usual nutritional treatment method for diabetes.
After that, LCD has been introduced into the health field and medical practice.4 Consequently, Dietary Intervention Randomized Controlled Trial (DIRECT) Group reported the better efficacy of LCD5 and similar results with longer years.6 With various reports, the comparison studies between CR and LCD have been continued.7 There are predominant clinical effects in LCD rather than CR. Recently, LCD has been known and spread in North American and European countries.8
On the other hand, LCD was launched in Japan by Dr. Ebe who is main researcher in our group.9 Successively, authors and colleagues have continued clinical research concerning LCD, related themes and ketones bodies.10 Among them, the author reported that the values of ketone bodies are extremely elevated in the axes of fetuses, placenta, newborn and pregnant women, indicating the significant physiological role of ketone bodies.11
There are recently several reports concerning clinical efficacy of LCD.12,13 Through our clinical investigation, authors have combined research on CR/LCD meals and continuous glucose monitoring (CGM).14,15 Authors have continued the medical practice for female diabetic patients in women’s clinic. One of the cases with pregnant diabetic patient will be described in this article, associated with the detail investigation of LCD and CGM.
History of present illness: The enrolled patient was 27 year-old female for type 2 diabetes mellitus (T2DM). She has been treated using insulin for 5 years, and delivered the first child by Caesarean section 3 years ago. Her weight had been approximately 98 kg before the pregnancy. Her usual physique has been 165㎝ in height and 98 kg in weight with Body Mass Index (BMI) 36.0.
During current pregnancy, she had been treated in University Hospital. She was given the meal of 1600 kcal a day and insulin therapy. The insulin administration method has been multiple daily insulin injection (MDI). It includes Novo rapid (Novo Nordisk) three times a day and Insulin Glargine (Eli Lilly and Company) at night once a day. The former is Insulin Aspart provided by pre–filled pen including 100units/mL, and the latter is Insulin Glargine by BS injection kit FFP including 300units/mL. The administration schedule of the insulin therapy was that Aspart is given 6, 6, 6 units on 0700h, 1200h, 1800h and Glargine is given 30 units on 2200h. For MDI therapy by University hospital, her HbA1c value was 9.7% in 12 weeks, and 7.0% in 28 weeks of pregnancy. She showed a little hypertensive with stable condition until 28 weeks without preeclampsia symptom or other clinical problems during this period.
Authors and colleagues have continued LCD treatment for various patients with T2DM and pregnancy cases, and LCD educational movement through the activity of Japan LCD Promotion Association (JLCDPA). This patient came to know the beneficial effect of LCD and hoped to be treated in our women’s clinic. Then, she visited our clinic for further evaluation and treatment for LCD at 28 weeks of pregnancy.
Physical examination: On the first contact in our women’s health and medical clinic, she showed 165 cm in stature and 101kg in body weight. Her Body Mass Index (BMI) was 37.1. Her consciousness was alert, and physicals were hypertensive and otherwise normal. There were no remarkable findings in her lung, heart, abdomen and neurological axis. Chest X-ray and Electrocardiogram (ECG) were unremarkable.
Laboratory tests: The data of the basal blood chemistry were as follows: AST 40U/L, ALT 31U/L, Total Protein 6.2g/dL, BUN 11mg/dL, Cre 0.3mg/dL, T-Cho 225mg/dL, TG 209mg/dL, HDL-C 67mg/dL, complete blood count; RBC 458x104/μl, Hb 13.2g/dL, MCV 89fL, WBC 7,910/μl, Platelet 20.1x104/μl, Fe 74μg/dL, UIBC 460μg/dL, TIBC 534μg/dL, Ferritin 62.3ng/mL. Biomarkers concerning diabetes and ketone bodies were as follows: HbA1c 7.0%, blood glucose 145mg/dL, total ketone body 259μmol/L (-131), acetoacetic acid (AcAc) 56μmol/L (-55), 3-hydroxybutylic acid (3-OHBA) 203μmol/L (-85).
CR and LCD: Concerning the nutritional therapy, there have been two main diet therapies. One is CR and another is LCD. Formerly, CR was the basic meal for nutritional therapy in Japan. The PFC ratio of CR has been as 15: 25: 60. This has been the standard diabetic meal recommended by the Japan Diabetes Association (JDA).16
In contrast, authors and colleagues have proposed three kinds of LCD, which are super LCD with 12%, standard LCD with 26% and petite LCD with 40% of carbohydrate.17 These protocol have been in applied in our studies, which are standard method of JLCDPA. In this case, super LCD meal with 12% of carbohydrate and 1600kcal per day was adopted.
CGM: Daily profile of blood glucose was investigated by CGM. For detail study of CGM, we applied FreeStyle Libre which has been rather prevalent for practical study. It was produced by Abbott Diabetes Care Inc., Alameda, CA, USA.18 FreeStyle Libre has been evaluated to be simple and beneficial for detecting blood glucose variability. It is also so small size that each patient can manage it easily with precise continuous data of changing blood glucose.19
Progress course: After the detail explanation and lecture of CR and LCD, she has understood the difference between the both well. She has recognized the significance of LCD and the consent for changing from CR to LCD. Furthermore, she started to measure the daily profile of blood glucose by CGM using FreeStyle Libre.
Formerly, she was given CR meal for 1600kcal and insulin therapy in the university hospital. The CR meal and insulin was given until 28th weeks of pregnancy, which was the same treatment as before. The glucose variability in 28th week is shown in Figure 1. Average glucose is around 160mg/dL, but hyperglycemia is observed after meals. The glucose variability showed variation with different time of blood glucose peak during 28th week.
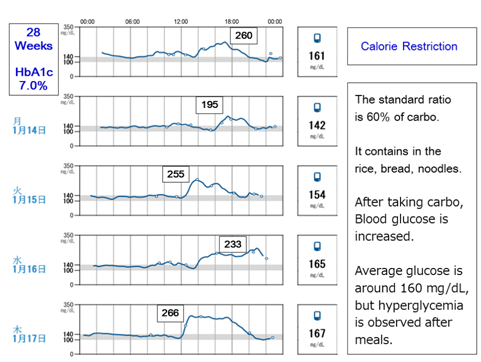
Figure 1 Glucose variability on 28th week by FreeStyle Libre. There are some episodes of hyperglycemia with HbA1c 7.0%.
After 29th week, she changed the meal from CR to LCD. Due to the decreasing blood glucose, insulin doses were reduced gradually day by day. The administration of insulin became unnecessary and was discontinued in 10 days. The glucose variability in 34th week is shown in Figure 2. The blood glucose variability was stable within normal range in preprandial and also postprandial period. She has continued to have various kinds of meal, such as egg, salmon, vegetables, meat winner, low carbo bread, and so on. Combined with the continuous advice of dietician nutritionists, she showed satisfactory clinical course after that with stable glucose variability and HbA1c level.
In this article, we presented a case of a pregnant woman with obesity and T2DM. She was given 48 units / day of insulin until 28 weeks. After that, she had further evaluation and treatment with CGM using FreeStyle Libre and LCD in our women’s clinic. Blood variability was remarkably improved in several days, and insulin administration was discontinued in 10 days. From these results, several medical aspects would be discussed.
The first is the clinical effect of LCD on diabetes. Dietary therapy for diabetes has been formerly CR. Later, the author and colleagues have introduced and spread the LCD for the first time in Japan.9 We have also reported clinical studies of research for LCD in thousands of people.20
Furthermore, the author showed a diabetic woman who dramatically improved the glucose variability when changing from CR to LCD.21 In addition, we have introduced three types of LCDs, which are super, standard, and petite LCDs.22 Thus, the movement of LCD has been spreading by books, lectures and clinical studies through the activities of the JLCDPA.23
The second is new knowledge in the field of female medicine. In other words, it relates to pre- and postpartum studies of pregnant women, as well as treatments for diabetes and pregnant women. There is the main theme of our research. In the clinical practice of LCD, elevation of blood ketone bodies has been an important finding and a crucial subject of research.
The author reported the impressive data that high concentrations of ketone bodies continue in the blood at the pregnant woman-placenta-fetus-newborn axis. In this system, the significance role of physiological ketone bodies would be recognized.11 In addition, we have experienced diabetic pregnant female cases in which the diabetic state dramatically improved with LCD rather than conventional CR and insulin treatment.
Thirdly, among such patients, one of the cases is described in this report. She was previously administered insulin totally 48 units per day. Until 28th week, she had showed a little hypertensive states, but did not eclampsia or other problems clinically. The content of the meal was changed from CR to LCD, in which the daily calorie intake is the same as 1600kcal. For comparison of CR vs LCD, the percentage of carbohydrates is 60% vs 12%, respectively, then the calories from carbohydrates are 960kcal vs 192kcal.22,23 Since 1g of carbohydrate has 4kcal in calorie, the amount of carbohydrate per day would be calculated as 240g vs 48g.
Thus, the carbohydrate intake was drastically reduced, so that the increase in blood sugar was suppressed. Consequently, diabetic state could be eventually improved in a short time to rather normal level where insulin administration became unnecessary in only 10 days. This would be clinically a prominent effect.
Furthermore, when carbohydrate intake is reduced, fat can be burned and ketone bodies are produced. Ketone bodies play very important roles as energy sources.11 In recent years, clinical usefulness of ketone bodies has been reported, and it is possible to spend pregnancy period safely without an increase in blood glucose.24,25
From mentioned above, clinical usefulness of LCD was observed. In the cases of diabetes with pregnancy and gestational diabetes, further evaluation and research for LCD in practical use would be expected to be more important than conventional CR diet plus insulin therapy.
Fourthly, CGM has various research aspects for years. From the fundamental point of FreeStyle Libre, the enzyme electrode method was introduced long ago.26 After that, the method of electrode were developed and lots of experiments were continued for CGM.27 There was the guideline of CGM and the international standardization including precision absolute relative difference (PARD) and mean absolute relative deviation (MARD).28,29
It is indeed that FreeStyle Libre shows the benefit for easy and accurate measurement of blood glucose variability. However, there is some discrepancy of HbA1c value between laboratory measurement and the estimated HbA1c level calculated by FreeStyle Libre. This is probably from the characteristics of measurement in every 15 minutes.30 Furthermore, It cannot detect occasional glucose acute spike-like increase of glucose.31 Consequently, further evaluation with various data accumulation would be necessary in the future.
There is the description of recommendations for CGM in the guideline 2019.32 The beneficial points are found in the correlation with the adherence to continuous usage of this device FreeStyle Libre. It shows the level of evidence as the rank of A.32
The fifth would be the significant exchange communication between patients and registered dietitian nutritionists (RDNs) by using FreeStyle Libre.21 The details are as follows:
On the other hand, there were some problems obtained from patient feedback.15 They are
As mentioned above, FreeStyle Libre has been evaluated. In general, the patient's impression for this device has been beneficial.14 They include that
A diabetic female patient became pregnant with the treatment of CR and 48 units of insulin per day. Consecutively, due to application of LCD and Freestyle Libre, insulin treatment could be discontinued in 10 days. Consequently, the usefulness of LCD and FreeStyle Libre would be reported. Further development of this research will be expected in the future.
None.
None.
Authors disclose no conflict of interests in publication of this study.

©2019 Muneta, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.