eISSN: 2377-4304


Case Report Volume 10 Issue 2
Department of Anesthesia, Baylor College of Medicine, USA
Correspondence: Lerin Rutherford, Baylor College of Medicine, 1504 Ben Taub Loop, Houston, TX 77030, USA, Tel 713-829-1110
Received: May 26, 2017 | Published: March 5, 2019
Citation: Thompson B, Rutherford L, Suresh M, et al. Cesarean section in a 17yo with coarctation of suprarenal aorta from takayasu aortitis. Obstet Gynecol Int J. 2019;10(2):84-85. DOI: 10.15406/ogij.2019.10.00419
Background: Takayasu arteritis is an inflammatory disorder of large vessels that primarily affects women of reproductive age. During pregnancy, uterine vessels can be affected resulting in uteroplacental insufficiency and unique hemodynamic challenges during anesthesia.
Case report: A 17 year old, primigravid female with known suprarenal narrowing of the aorta presented for emergency cesarean section at 37 weeks. Patient underwent placement of epidural catheter with followed by surgical delivery, remaining HDS. Cesarean was complicated by uterine atony.
Conclusion: This case illustrates one approach to anesthetic management of this rare condition and demonstrates the benefits of slow onset, high-concentration local anesthetic epidural analgesia to minimize hemodynamic perturbations.
Keywords: takayasu arteritis, coarctation of the aorta, cesarean section, anesthesia
Takayasu arteritis is a chronic inflammatory disorder of large to medium size vessels. The etiology is thought to be autoimmune mechanisms that are antibody mediated. Symptoms include fever and fatigue with progression to signs and symptoms of heart failure. On physical exam bruits over the neck, supraclavicular areas and abdomen or blood pressure differentials between the extremities may be present.1
The inflammatory process most commonly targets the aorta and its branches, resulting in thickening of the vessel wall. As a result, there can be narrowing of the lumen with hemodynamic compromise similar to that seen in coarctation with distal after load dependence. In addition to vessel wall thickening, post-stenotic aneurysmal dilation can occur as a result of the destruction of the elastic intima and muscular media from inflammatory cells. As the disease progresses, other vessels can become involved such as the carotid, subclavian and pulmonary arteries. Worldwide, the estimated incidence of Takayasu arteritis is estimated to be 2.6 new cases per year per million people, most commonly affecting women of reproductive age.2
In pregnancy, the most common presenting signs of TA are severe hypertension (either mistaken for or combined with superimposed pre-eclampsia) and congestive heart failure. In one study TA was found to have a 40% frequency of obstetric complications.3 It has been associated with abortion, intrauterine death, intrauterine growth retardation, and premature delivery. Abdominal aortic involvement was associated with worse perinatal outcomes.4
A 17 year old primagravid female initially presented at 27 weeks gestation for follow up obstetrical care. Medical history was significant for a diagnosis of hypertension at age 11 during which time she described claudication symptoms of her lower extremities and easy fatigability. She was placed on antihypertensive medications at that time and followed by her physician in Honduras. In addition, she reported occasional tobacco and methamphetamine use.
At the time of this admission, she brought imaging records from an outside hospital demonstrating a suprarenal 8cm segment of abdominal aortic narrowing with a lumen of 5mm. Subsequent abdominal ultrasounds at our institution were unable to visualize the abdominal aorta due to the gravid uterus. Umbilical and common femoral arteries were visualized and showed adequate flow. MRA of the brain ruled out any aneurysmal segments of the carotid and cerebral circulation. In addition, an echocardiogram was performed showing normal ventricular size and systolic function with as estimated ejection fraction of 60% (Figure 1).
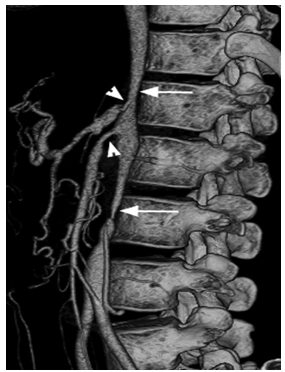
Figure 1 Patient image showing narrowing of abdominal aorta, suprarenal lumen approximately 5cm in diameter.
After a multidisciplinary conference with Obstetricians, Cardiologists, Vascular surgeons and Obstetric Anesthesiologists, the patient was scheduled for cesarean section under epidural regional anesthesia. However, prior to the scheduled date the patient went in to labor and the case was performed emergently.
The patient was taken to preoperative holding and 2 large bore IV’s were placed in addition to a right radial arterial line. She was then transferred to the operating room where a central venous catheter was placed in the left antecubital vein. The right femoral artery was cannulated as well under ultrasound guidance. The pressure gradient at that time was noted to be approximately 50mmHg between the upper extremity mean and the femoral artery mean pressures.
She was then placed in a sitting position for placement of the epidural catheter. The epidural space was located at 3.5cm and catheter was threaded to 8cm. The catheter was then bolused with 15cc of Bupivicaine 0.5% with Fentanyl 4mcg/cc in slow increments of 3cc every 5 minutes and then 6cc of Lidocaine 2% was given. The patient had a T6 level at this time and the decision was made to proceed with surgery.
The patient became very anxious at this time and was given low doses midazolam and remifentanil. After delivery of the baby and placenta, the blood pressure was maintained with boluses of colloid and lactated ringers with a low dose infusion of phenylephrine due to uterine atony. She was given Oxytocin 50 units, Hemabate IM and Cytotec per rectum.
The patient was hemodynamically stable throughout the procedure with MAP in the 120-140 range in the upper extremity and 65-80 in the lower extremities. In total 3500ml of Lactated ringers and 1000ml of colloid were given. The phenylephrine infusion was stopped after uterine tone and hemostasis was achieved. Blood loss was estimated to be 1200ml. At the conclusion of the procedure, the epidural catheter was bolused with Butorphanol 1mg and Duramorph 4mg. The epidural catheter was discontinued and the patient was transferred to the Surgery Intensive Care Unit for further monitoring.
Takayasu arteritis can involve any vessel in the arterial tree causing impaired perfusion to target organs. During pregnancy, the uterine vessels may be involved, resulting in uteroplacental insufficiency. The deleterious effects to the fetus could necessitate a surgical emergency. Therefore, it is of paramount importance that pressures be maintained high enough to ensure adequate perfusion distal to the point of obstruction and in this case, perfusion to key end organs such as the uterus and spinal cord. In contrast, uncontrolled hypertension proximal to the obstruction carries a risk of dissection. During the case, invasive blood pressure monitoring was utilized in both the upper and lower extremities allowing close monitoring of these parameters.
Likewise, it is important to tailor drug choice to the goal of maintaining hemodynamic stability. Patients with Takayasu arteritis may not tolerate acute decreases in preload since the diffuse inflammation can lead to stenotic vessels and interferes with normal compensatory mechanisms.5 Hypotension is a significant risk associated with both epidural anesthesia and cesarean section itself. Epidural anesthesia decreases systemic vascular resistance and manipulation of the uterus intraoperatively can trigger increased vagal tone. In this case, the anesthetic effects were minimized using a slow onset, high-concentration local anesthetic such as bupivacaine. Blood loss posed an additional challenge in this case, requiring aggressive management of uterine atony and volume replacement.
Complex cases such as this benefit from a multi-disciplinary approach and careful pre-anesthetic preparation. Thoughtful choice of appropriate monitors as well as drugs can assist in smoothing the intraoperative course.
None.
The authors declare no conflicts of interest.

©2019 Thompson, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.