eISSN: 2377-4304


Case Report Volume 13 Issue 6
1Department of gynecology obstetric surgery, at Mohammed VI University Hospital center, Morocco
2Department of clinical hematology at Mohammed VI University Hospital center, Morocco
3Department of biological hematology at Mohammed VI University Hospital center, Morocco
4Department of Pathology, at Mohammed VI University Hospital center, Morocco
Correspondence: Boutaibi F, The department of genecology obstetric surgery, at Mohammed VI University Hospital center, Morocco, Tel 00212668590703
Received: November 16, 2022 | Published: December 05, 2022
Citation: DOI: 10.15406/ogij.2022.13.00679
metastases is a rare occurrence in patients with metastatic breast cancer.
For the specialists, managing patients with bone marrow metastases presents significant challenges. Therefore it is important to carefully balance the risks and benefits of a course of treatment.
We present a case study of a 56-year-old female patient with pancytopenia who showed no signs of breast cancer. However the breast carcinoma were discovered in the bone marrow by a biopsy.
Chemotherapy and hormonal therapy were administered to this patient, and the outcomes were encouraging
Keywords: Breast cancer, bone marrow, metastasis
Breast cancer is the most common cancer in females worldwide and also in Morocco, According to the Moroccan National Cancer Registry the breast cancer is estimated to account for 35.8% of all female cancer patients. Each year, 4839 new case of breast cancer are diagnosed in morocco.1
Only 0.17 % of the 12970 breast cancer patients had symptomatic bone marrow metastases, making it an exceptional manifestation of metastatic breast cancer.
These cases have a poor prognosis. The only method for treating hematologic crisis' life-threatening situations is with cytotoxic chemotherapy regimens.2
However, symptomatic bone marrow metastasis from breast cancer tends to have a longer median life, possibly as a result of its characteristics that can be treated. We would like share a case of marrow carcinomatosis that, due to immunohistochemical labeling and a significant response to tamoxifen treatment, was shown to result from a challenging breast cancer.
It is about a 56-year-old patient, married and mother of 4 children, followed for arterial hypertension controlled by monotherapy. The patient had her menarche at the age of 14, her cycles were regular, she had her menopause 4 years ago and during her period of genital activity she was on oral hormonal contraception.
The family investigation has objectified no history of cancer in the family. The symptomatology dates back to September 2020 with the installation of thrombocytopenic purpura revealing pancytopenia Breast examination has objectified no palpable nodule no adenopathy no inflammatory sign opposite. The rest of the exam is unremarkable.
Initial blood test has showed Hb 6.5g/dl WBC 3000/µl platelet count 11000/µl Reticulocyte count 14220/µl Ca 15-3: 33UI/ml.
Myelogram showed the presence of extra hematopoietic cells. Subsequently the diagnosis of poorly differentiated breast carcinoma was made by osteo-medullary biopsy, followed by an immunohistochemical study which objectified: ER 90% P r10% Ki67 60% Her2 negative: Luminal B (Figure 1).
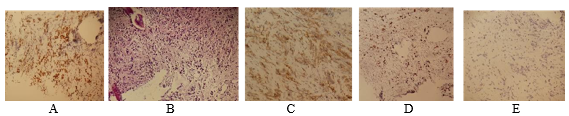
Figure 1 Immunohistochemical stain of adenocarcinoma in bone marrow A (ER) B (HE) C (HER2) D (Ki67) E (PR).
Subsequently the patient benefited from a mammography which showed a nodule at the level of the right superio-external quadrant measuring 6mm*2mm (Figure 2). Afterwards an ultrasound-guided biopsy was performed which showed poorly differentiated breast carcinoma grade II of SBR
As part of the extension assessment CT Thoracic-abdominal-pelvic has showed Non-specific intraparenchymal and sub pleural micro nodules with suspicious-looking right iliac condensing lesions. Finally a bone Scintigraphy was clear of any fixation anomaly.
In total: it is a right breast carcinoma luminal profile B at the TisN0M1 stage, revealed by an invasion of the bone marrow without visceral metastases.
The therapeutic approach: The patient received Neo adjuvant chemotherapy under protocol; Adriamycin 20 mg/m2 on D1 D8 D15 and Cyclophosphamide 200mg/m2 D1 D 21.Associated with tamoxifen as an hormonal treatment
The progress was tagged by complete clinical response. Radiologically we noted a disappearance of breast nodule and stabilization of bone lesions.
On a biological level the progress was marked by: Hb 11g/dl, platelet count 228000/mm3, ANC: 2920/mm3, Ca 15-3: 23UI/ml
Afterward, the patient underwent a right mastectomy with homolateral Axillary lymph node dissection the post-operative follow-up went without complications and during quarterly monitoring the patient showed no signs of recurrence during all years of surveillance.
Cases of breast cancer initially diagnosed by hematologic disorders due to disseminated carcinomatosis in the bone are rare. Some patients with metastatic cancers have no primary location despite the more sophisticated diagnostic workup. Because it is aggressive and frequently extensive when it first manifests, treating cancer with an unknown primary is challenging.
There are few data on the prevalence, diagnosis, treatment plan, and prognosis of breast cancer patients with diffuse bone marrow metastases. They typically had invasive lobular histology and HR-positive, multicentric, moderately to poorly differentiated tumors when they were diagnosed, like the patient described in our clinical case.3
Around 3% of patients with early-stage breast cancer reported occult micrometastasis to the bone marrow, which was thought to be a poor prognostic predictor.
On the other hand, anemia is the most common symptom at presentation, and symptomatic diffuse bone marrow metastases is thought to occur in just 0.17% of individuals with breast cancer.4 In parallel to the previously stated symptoms, our patient also presented with pancytopenia.
Cytopenia will occur from hematopoiesis abnormalities brought on by the invasion of cancer cells in the bone marrow. Tumor cell invasion would typically occur in pancytopenia or severe marrow failure. In this situation, the peripheral blood result that revealed pancytopenia raised suspicions regarding the bone marrow. Going to follow that, a bone marrow biopsy was performed to confirm the diagnosis.
However a bone marrow metastasis typically progresses to an advanced stage of cancer, effective treatment with endocrine therapies, chemotherapy, and targeted therapy could still be able to extend survival in cases when the origin is the breast.
The absence of HER2 and the significant ER/PR expression in our patient's tumor cells allowed us to predict that her tamoxifen treatment would be extremely successful. Hematologic abnormalities in cancer patients are thought to have unclear pathogenic mechanisms. Diffuse bone marrow metastases may result in anomalies of the coagulation-fibrinolytic system due to damage to vascular endothelial cells, excessive thromboplastic activity, and the presence of tissue thromboplastin-like substances.
From a clinical perspective, patients with gastric and breast cancer have been documented in the majority of cases of cancer-associated hematologic abnormalities.5
The primary treatment for extended survival time at this time is the administration of potent anti-cancer therapies; however, the diseases are not totally curable.
Cytopenia makes it difficult to treat patients with disseminated carcinomatosis of the bone marrow. For diffuse carcinomatosis of the bone marrow due by breast cancer, systemic chemotherapy is usually applied and recommended.
The requirement for supportive therapy, such as blood transfusions and granulocyte colony-stimulating factor support, can arise from the fact that chemotherapy can exacerbate pretreatment hematologic abnormalities from disseminated carcinomatosis of the bone marrow.6
In the current case, the weekly initial treatment of the AC protocol (ADRIAMYCIN/ Cyclophosphamide) was successful in treating the bone marrow lesion. All through remaining of the treatment, hematologic disorders remained absent.
From a clinical perspective, we determined that the most effective regimen for treating this kind of disease involved weekly injection of AC (ADRIAMYCIN/ Cyclophosphamide).6
The literature contains few published studies on the effectiveness of hormone therapy in the treatment of luminal breast cancer with disseminated bone marrow carcinomatosis.7 In our example, a 56-year-old woman was diagnosed with diffuse bone marrow metastases from an occult HR-positive, HER2-negative breast cancer; tamoxifen treatment led to a prolonged response and the restoration of hematological markers.
Pursuing a rather aggressive approach is also supported by the prognosis, the median survival time after bone morrow metastasis 19 months in Kopp’s study.8 Since the median overall survival was 31 months, the diagnosis of breast metastatic cancer should not be viewed as a sign of poor prognosis. Our findings are consistent with previously published case reports in maximal tolerated dose chemotherapy regimens produced prolonged remissions of breast metastatic cancer.9
Currently, imaging, tumor markers, and clinical evaluation are being used to determine treatment response. However, in asymptomatic "disease-free" patients, standard restaging assays could not be sufficient to predict relapse/progression.
Many patients who get adjuvant therapy have no symptoms of the cancer, yet they will still experience future metastatic years.
Following the end of the treatment. Thus, until a clear recurrence, the efficacy of the selected treatment plan remains unknown. After the initial tumor has been removed, the only measure for evaluation is minimal residual disease. Circulating Tumor Cells measures in peripheral blood are used in the majority of research on therapy monitoring since assays based on bone marrow punctures are less widely available due to their invasiveness and expense.10,11
Currently, imaging, tumor markers, and clinical evaluation are being used to determine treatment response. However, in asymptomatic "disease-free" patients, standard restaging assays could not be sufficient to predict relapse/progression.
Following the end of the treatment. Thus, until a clear recurrence, the efficacy of the selected treatment plan remains unknown. After the initial tumor has been removed, the only measure for evaluation is minimal residual disease.
None.
None.
Authors declares that there are no conflicts of interest.

©2022 , et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.