eISSN: 2377-4304


Gynecological fistulas that are familiar are vesicovaginal, rectovaginal and ureterovaginal fistulas, which may be due to childbirth, operative injury, tumour or radiation. Tubocutaneous fistula, is as a very rare condition secondary to tuberculosis, endometriosis, and complications of child birth and gynecological surgeries. We report a 30 year old woman with a tuberculous tubocutaneous fistula, arising from the right salphingeal tube and discharging in the lower abdomen cutaneously, who underwent laparoscopic right salpingo oophorectomy, and excision of the tract upto the skin, and the abdominal wall, with open excision of the distal part. The case is being published for its rarity, and to remind gynecologists to consider this possibility in a non-healing sinus in the lower abdomen. The authors believe this to be the first such case in literature.
A 30 year old woman was presented to us with a history of her recurrent discharging sinus in the lower abdomen just lateral to the right end of her pfannensteil scar and intermittent lower abdominal pain for one year. There was no history of dysuria or white discharge per vagina. She gave history of recurrent fever followed by discharge from the sinus. The discharge was purulent, and had not yielded any bacteriological growth. The patient had two Caesarean sections; the last child birth was six years ago. She had undergone multiple explorations of the sinus, and polypropylene suture was removed from the depth of the sinus, showing some granulation tissue in histopathology. Despite three excisions, the sinus recurred. She was a known Diabetic and hypertensive for four years on regular medications.
On examination, her general condition and vitals were normal. Abdominal examination revealed a 2* 3 cm induration in the right iliac fossa with tenderness and a discharging sinus from the right end of the pfannensteil scar (Figure 1) from which a pus culture was taken. On per speculum examination, her cervix was hypertrophied with erosion and mild discharge. On per vaginal examination, uterus was bulky with right forniceal tenderness. An ultrasonogram was taken which showed a 4*5 cm right ovarian cyst with multiple small fibroids. MRI screening had shown a tract that extended from the right tubo ovarian area upto the skin. Other investigations like blood count and chest x-ray revealed no evidence of tuberculosis. In view of the radiographic findings, possible tubocutaneous fistula was diagnosed, and we decided to take up for diagnostic laparoscopy.
On laparoscopy the findings were:
Small bowel and omentum were adherent to the right ovary, same separated and small bowel and omentum freed. The uterus was adherent to anterior abdominal wall with adhesions but separate from the fistula. By using the vessel sealer and bipolar cautery, the medial aspect of the tube and the broad ligament were separated from the uterus. The infundibulo-pelvic ligament was taken as well. The tube, ovary, inflammatory mass and the tract going up to the anterior abdominal wall were excised in-toto laparoscopically (Figures 3a, 3b) and the distal part of the tract on the abdominal wall was excised externally and closed with 1-0 vicryl (Figures 4,5). The blood loss was negligible. Closure was done in layers after washing out the abdominal wall thoroughly. The specimen was sent for histopathology.
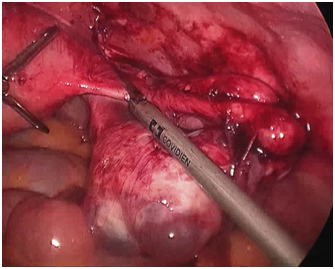
Figure 3a Medial part of dissection of the tube, inflammatory mass and the tract going upto the anterior abdominal wall.
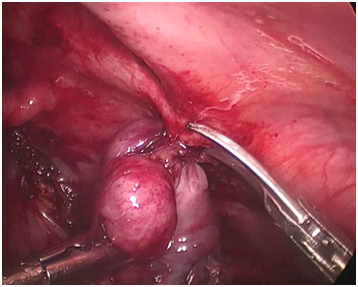
Figure 3b Dissection of distal portion of ovary, inflammatory mass and the tract upto anterior abdominal wall.
Post-operatively, the patient was put on antibiotics and analgesics. She had no infection of the wound and was back to normal in a few days. Histopathology revealed simple serous ovarian cyst with fistulous tract running from the inner lining of the right fallopian tube up to the skin, and this was surrounded by granulation tissue with epithelioid cells, Langhans giant cells, lymphocytes, highly suggestive of tuberculosis. Pus cultures were negative for growth of mycobacterium, but the PCR of the fluid was positive for Mycobacterium tuberculosis. The patient was subsequently started on anti-tuberculous therapy, and at follow up was asymptomatic.
Wittich et al in 1982 first reported a tubocutaneous fistula.1 This case on retrospect is a tuberculous tuboctaneous fistula, commencing in a tuberculous tubo- ovarian abscess, and finding its way to the skin.
Is it a fistula?
Yes, because both epithelial surfaces were clearly connected, the tubal and the cutaneous.
Where did the infection begin?
Tubo- ovarian tuberculosis is well known, although its presentation as a fistula is extremely rare.
A pathological communication between the fallopian tube and skin is quite rare. Causes described in literature are pelvic inflammatory disease, Crohn’s disease, tuberculosis, endometriosis, inflammatory bowel disease and pelvic surgeries.2–5 The current literature advocates salpingectomy or salpingo-oophorectomy and complete excision of the tract as definitive treatment.6 Nayini et al reported a case without any specific disease process. The best imaging modality recommended is MRI or CT scan.7 A high index of suspicion in a persistently discharging sinus of the lower abdomen is required. Belli et al reported a persistent ischiorectal fistula of tubo-ovarian origin.8
All the available reports, intra-operative details are of open surgery only.2–11 In our case, we used the ‘medial to lateral’ approach. As the medial end of the fallopian tube and broad ligament were unaffected in the inflammatory process, we disconnected the medial attachments first. The next step was to devascularise the inflammatory phlegmon completely, and the ovarian vessels were sealed and cut. The rest of the dissection consisted of removing the entire fistula up to the peritoneum. Perhaps a PCR testing in the early stages of her disease might have yielded results for aggressive antitubercular therapy.
A small number of cases have been reported of fistulas between the fallopian tube and the neighbouring colon, small bowel, or bladder, all these fistulas managed by laparotomies. To our knowledge, this is the first ever case report of a Total Laparoscopic excision of a tuberculous tubocutaneous fistula.
This article highlights the need to consider the possibility of an underlying Tubocutaneous or Uterocutaneous fistula as a cause for a non-healing lower abdominal sinus, especially after multiple explorations. Early diagnosis and adequate surgical clearance will serve to prevent complications in the long term. This case, a Totally Laparoscopic excision of a Tubocutaneous Tuberculous fistula, is being published, as it is the first of its kind in literature, to our knowledge.
None.
The authors declare that they have no conflict of interest.

© . This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.