eISSN: 2377-4304


Case Report Volume 9 Issue 3
1Department of Obstetrics and Gynecology, Southern California Kaiser Permanente, USA
2St Georges University, School of Medicine, Grenada
3Maternal and Fetal Medicine, Department of Obstetrics and Gynecology, Lincoln Medical and Mental Health Center, USA
4Department of Pathology & Immunology, Baylor College of Medicine, USA
5Division of Minimally Invasive Gynecologic Surgery, Department of Obstetrics and Gynecology, Baylor College of Medicine, USA
Correspondence: Xiaoming Guan MD PhD, Section Chief and Fellowship Director, Division of Minimally Invasive Gynecologic Surgery, Department of Obstetrics and Gynecology, Baylor College of Medicine, 6651 Main Street, 10th Floor, Houston, Texas, 77030, USA, Tel (832) 826-7464, Fax (832) 825-9349
Received: April 22, 2018 | Published: May 24, 2018
Citation: Rezai S, Hughes HV, Patil NM et al. Single site robotic-assisted laparoscopic transperitoneal ligation of ovarian veins for treatment of pelvic congestion syndrome; a case report and review of literature. Obstet Gynecol Int J. 2018;9(3):191-194. DOI: 10.15406/ogij.2018.09.00329
Background: Pelvic congestion syndrome (PCS) is a condition which is not clearly understood but is associated with chronic pelvic pain. Pelvic congestion syndrome is most commonly seen in multiparous premenopausal women but may also be asymptomatic. PCS occurs when the veins of the pelvis are dilated leading to blood pooling in the pelvis and even causing reverse flow. Two anatomical findings are characteristic of PCS ovarian vein reflux and pelvic varicosities.
Case: The patient was a 32 year old female gravida 8, para 1-2-5-3, with pelvic congestion syndrome who was managed by single site robotic-assisted laparoscopic transperitoneal ligation of the left ovarian veins. The patient underwent robotic assisted single-incision (RASI) hysterectomy, with left ovarian vein ligation for pelvic congestion syndrome.
Conclusion: While robotics continue to have the benefits of excellent 3D visualization, the robotic-single site instruments have decreased range of motion and do not yet have the ability to articulate which requires minor changes to surgical technique. Despite minor technology limitation, single-site robotic technology is a useful tool to perform very fine dissections.
Keywords: endovascular embolization treatment, endovascular therapy, endovascular treatment, laparoendoscopic single-site surgery (LESS), magnetic resonance angiography (MRA), ovarian vein, ovarian vein embolization, ovarian vein ligation, ovarian vein syndrome, pelvic congestion syndrome, pelvic vein ligation, robotic-assisted laparoscopic transperitoneal ligation of ovarian veins, single-incision laparoscopic surgery (SILS), transperitoneal
LESS, laparoendoscopic single-site surgery; MRA, magnetic resonance angiography; SILS, single-incision laparoscopic surgery; CPP, chronic pelvic pain; PCS, pelvic congestion syndrome; RASI, robotic assisted single incision laparoscopic; AUB, abnormal uterine bleeding; IP, infundibulopelvic; ICG, indocyanine green; NSAIDs, non-steroidal anti-inflammatory drugs; GnRH, gonadotropin releasing hormone; CBT, cognitive behavioral therapy; MIGS, minimally invasive gynecological surgery
Pelvic congestion syndrome (PCS) is a condition which although not clearly understood is associated with chronic pelvic pain (CPP).1−3 Pelvic congestion syndrome (PCS) is most commonly seen in multiparous premenopausal women but may also be asymptomatic.4 This syndrome occurs when the veins of the pelvis become dilated leading to blood pooling in the pelvis and even causing reverse flow. Two anatomical findings are characteristic of pelvic congestion syndrome; ovarian vein reflux and pelvic varicosities.5,2
Women affected by PCS most commonly present with pain, which may vary from being acute to chronic, unilateral to bilateral, or sharp to dull.4,5 The pain associated with PCS occurs when the intima of pelvic vessels are stretched releasing inflammatory mediators such as substance P.4Patients often describe PCS as a postcoital ache rather than pain which is exacerbated by standing, and relieved when lying down.6 PCS may also be associated with non-pain symptoms such as bladder or bowel irritability, and leg fullness or varicosities.6
Unfortunately, most underlying causes of pelvic pain syndrome go undiagnosed and make up a large proportion of gynecological visits.4 Differential diagnosis for chronic pelvic pain (CPP) includes endometriosis, pelvic inflammatory syndrome, fibroids and adenomyosis.7
The etiology of PCS remains unclear but is thought to be multivariable including physical and hormonal factors.5,8 These factors cause pelvic veins to become incompetent leading to congestion and retrograde flow.7 Congenital or acquired valvular insufficiency, and venous obstruction are the mechanical causes of PCS.9 Hormones, specifically those which result in venodilation or decrease in vasomotor tone, play a role in PCS. This correlates with the increased incidence seen in multiparous women and the decrease in incidence after menopause.6
Investigations for PCS include pelvic ultrasound, venography and laparoscopy.4 These investigations will reveal pelvic venous congestion or atypical flow.4 Treatment of PCS can be medical, surgical or endovascular.4 When medical management fails, surgical treatment has been shown to be effective in the majority of patients.10 We present a case of robotic assisted single-incision (RASI) hysterectomy, with left ovarian vein ligation for a patient with PCS.11
The patient was a 32 year old female gravida 8, para 1-2-5-3, with a past medical history of anxiety, depression, and post-partum depression, as well as 3 cesarean deliveries and 5 spontaneous abortions. She had undergone elective bilateral tubal ligation as well as hysteroscopy and endometrial ablation for abnormal uterine bleeding one year prior and had tried oral contraceptive pills and an intrauterine device without relief. The patient presented to our clinic with constant bloating, pelvic discomfort, pelvic pressure, dyspareunia and vaginal soreness for the previous 2-3 weeks. She also reported hot flashes, night sweats and difficulty sleeping that started about 2 months prior.
Laboratory work up for prolactin, testosterone, vitamin D, vitamin B12, vitamin B6, hemoglobin A1C and Lyme disease as well as sleep studies were all unremarkable. Vaginal exam and bimanual exam were normal.
Pelvic ultrasound was unremarkable but Magnetic resonance angiography (MRA) pelvis revealed engorged bilateral paravaginal vessels and enlarged bilateral pelvic varices (Figure 1) (Figure 2). Post-contrast images with Valsalva demonstrated reflux into the left gonadal vein with left pelvic varices. The left pelvic varix measured 0.9cm and the right pelvic varix measured 0.7cm. The left gonadal vein measured 0.5cm in the short axis. There was antegrade filling of the right paravaginal vessels with Valsalva. These findings were compatible with PCS with reflux into the left gonadal vein.
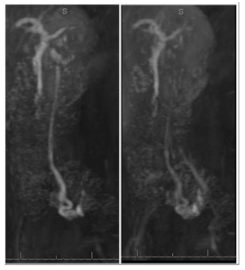
Figure 2 Sagittal Posts MRA of Pelvis. Vessels: Engorged bilateral paravaginal vessels and enlarged bilateral pelvic varices noted. Post contrast images with Valsalva demonstrate reflux into the left gonadal vein with left pelvic varices. The left pelvic varix measures 0.9cm. A right pelvic varix measures 0.7cm. The left gonadal vein measures 0.5cm in short axis. There is antegrade filling of the right paravaginal vessels with Valsalva. The findings are compatible with pelvic congestion syndrome with reflux into the left gonadal vein.
The patient underwent RASI laparoscopic surgery, consisting of total hysterectomy with bilateral salpingectomy, left ovarian vein ligation and cystoscopy (Figure 3A). Intraoperative findings included: normal uterus, fallopian tubes and ovaries. Omental and bowel adhesions to the left infundibulopelvic (IP) ligament were visualized and lysed (Figure 3B). An enlarged left ovarian vein as well as significant amount of bladder adhesions were also noted (Figure 3C).
After the left infundibulopelvic (IP) ligament was dissected out to identify the ovarian vessels, the left ovarian artery was identified with the assistance of Indocyanine green (ICG) administration (Figure 3D). The left ovarian vein was then ligated with Ethibond suture 0. Pathologic examination demonstrated congestion of large vessels and capillaries, including ectatic capillaries compatible with increased pressure (Figure 4).

Figure 3 Intraoperative laparoscopic images:
3A (top left): Single-Site Wristed Needle Driver was used. Survey after ovarian vein ligation showing hemostasis and tied sutures in place.
3B (top right): Adhesions of left ovary and the bowel
3C (bottom Left): Indocyanine Green (ICG) was used to identify the left ovarian artery
3D (bottom Right): left ovary with enlarged, engorged ovarian vessels
The patient had an uncomplicated recovery course. On postoperative follow up visit, she reported that the symptoms had resolved.
PCS can be a complicated and debilitating syndrome affecting many women. Medical management of PCS12 includes non-steroidal anti-inflammatory drugs (NSAIDs),13 medroxyprogesterone acetate and gonadotropin releasing hormone (GnRH), which are effective, but only for a short period of time.7 As in the case described above our patient attempted medical management which failed and she opted for surgical treatment. Because she had already undergone a sterilization procedure, fertility was no longer an issue; therefore a total hysterectomy and salpingectomy were performed. In patients desiring to preserve fertility, pelvic vein ligation alone has been shown to be effective.14
Left ovarian artery and left ovarian vein ligation was done in this case. Left sided congestion is more common (for anatomical reasons) as it is with male varices.7,15,16
Occasionally, bilateral ovarian embolization can be done for management of PCS. Hysterectomy and oophorectomy have been shown to be effective in most patients.6
Our goal for surgical management was to reduce blood flow to the pelvis and thereby reduce congestion and pain. This can be accomplished by ligating large vessels (ovarian) with or without removal of the uterus and fallopian tubes. Ligation of the ovarian vein effectively cuts off circulation to the pelvis and can be done laparoscopically or by interventional radiology.7 In our case because surgery was performed endoscopically, we sutured to achieve ligation. ICG was used to assist in identification of the pelvic vasculature (Figure 3).
Robotic assisted single-incision (RASI) was used in this case, and has some limitations compared to multi-port robotic surgery.11 However, the use of robotics, by an experienced surgeon, has shown improved outcomes with reduced surgical time, reducing hospital stays and improving pain management.17,18 The single incision endoscopic approach has the potential to produce a ‘no scar’ surgical site as the incision can be hidden in the navel.19
PCS has been associated with a host of psychiatric conditions such as anxiety, depression and postpartum depression.20,21 Previous miscarriage or childhood trauma have also been shown to be associated with PCS.22 The connection between PCS and a complicated obstetrical/ gynecological or psychiatric history adds to the complexity of this syndrome, as seen in the case presented. Although not applied to our patient, studies have shown some benefit from cognitive behavioral therapy (CBT) in the treatment of PCS.4
Two minimally invasive gynecological surgery (MIGS) techniques were used in combination for this case. While robotics continue to have the benefits of excellent 3D visualization, the robotic-single site instruments have decreased range of motion and do not yet have the ability to articulate which requires minor changes to surgical technique. Despite minor technology limitation, single-site robotic technology is a useful tool to preform very fine dissections.11 The use of RA-SILS for dissection and ligation of pelvic vessels proved beneficial with complete resolution of the patientsin this case after symptoms.
None.
Dr. Xiaoming Guan is a speaker for Applied Medical, Rancho Santa Margarita, California. Other authors did not report any potential conflicts of interests.

©2018 Rezai, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.