eISSN: 2377-4304


A retroperitoneal hematoma secondary to rupture of an ovarian artery pseudo aneurysm after an uncomplicated vaginal delivery is a rare, but life-threatening entity. We present a case of a 39-year-old multipara who developed hemorrhagic shock hours after an uncomplicated vaginal delivery, and was found to have a retroperitoneal hematoma on computed tomography (CT) scan. The patient was successfully treated with percutaneous arterial embolization within twenty-four hours of delivery, and discharged home on postpartum day seven. After discharge, patient developed pulmonary embolism which was treated medically. A high index of suspicion is required to make the accurate diagnosis of a ruptured ovarian artery pseudo-aneurysm after vaginal delivery. Contrast-enhanced CT scan is an excellent diagnostic tool, and percutaneous angiographic embolization is an effective management strategy even in hemodynamically unstable patient.
Keywords: Retroperitoneal hematoma; Ovarian artery pseudo aneurysm; Postpartum; Vaginal delivery
CT: Computed Tomography, FAST: Focused Assessment with Sonography in Trauma, IR: Interventional Radiology
Rupture of an ovarian artery pseudo-aneurysm after spontaneous vaginal delivery is a rare cause of retroperitoneal hematoma. It has been reported to occur immediately or days after delivery, as well as in non-peripartum women.1 The typical presentation includes severe flank pain with hemodynamic instability.2 It can also present as a worsening retroperitoneal or vaginal hematoma.3 Accurate diagnosis can be made by contrast-enhanced computed tomography (CT), and is crucial for the definitive management that includes either conservative interventions with percutaneous artery embolization or operative artery ligation.
A 39-year-old gravida 8 and para 7 delivered a 3,460 g healthy boy by spontaneous normal vaginal delivery at 39 weeks of gestation with Apgar score of 9/9 at 1 and 5 minutes. The patient did not require an episiotomy, and did not have any lacerations or repairs. The estimated blood loss was 300 ml at delivery. Approximately fourteen hours later, she complained of the acute onset of severe left lower abdominal pain and dizziness. The physical examination revealed pallor, a well-contracted uterus with minimal lochia, and tenderness in the left lower quadrant. Her vital signs were significant for a blood pressure of 70/40 mm Hg and heart rate of 81/min. Immediate resuscitation was initiated by securing a second intravenous access and administering a one-liter bolus of Lactated Ringer’s.
Laboratory tests including complete blood count and coagulation profile were sent. There was a suspicion of retroperitoneal fluid collection on Focused Assessment with Sonography in Trauma (FAST) ultrasound examination of the abdomen. The endometrial thickness was noted to be 0.7 cm. The hemoglobin and hematocrit obtained were 8.6 gm/dl and 26%, which were significantly decreased from 11.9 gm/dl and 36.3% at the time of admission. The coagulation profile was normal with an INR of 1.0. Transfusion of two units of packed red blood cells was started, and a contrast-enhanced computed tomography (CT) scan of the abdomen and pelvis was obtained. The CT showed a large amount of complex fluid in the pelvis extending caudally along the left retroperitoneum to the level of the upper left renal pole with a mass effect on the uterus and left kidney (Figure 1 & 2). The collection contained a prominent, tortuous left ovarian artery coursing through the hematoma with a contrast-filled outpouching measuring 1.6 cm in the mid-portion of the artery which was suspicious for pseudo-aneurysm.

Figure 1 Coronal image of CT abdomen and pelvis demonstrates a large left pelvic and retroperitoneal hematoma extending up to the level of the kidney with mass effect on surrounding structures.

Figure 2 Axial CT image of abdomen and pelvis demonstrates a large left pelvic and retroperitoneal hematoma.
Interventional Radiology (IR) consultation was obtained and CT-guided angiography of the abdomen and pelvis was performed which demonstrated a markedly dilated, tortuous left ovarian artery with a 2.5 cm pseudo-aneurysm at the proximal to mid portion, and adjacent contrast extravasation into the retroperitoneum. At the same time, percutaneous embolization was performed using 6, 8, and 10 mm nester embolization coils as well as Gelfoam slurry (Figure 3A & 3B). Gynecologic oncology consultation was also obtained, and the decision was made not to perform a laparotomy, but to observe for further evidence of ongoing bleeding.

Figure 3A Abdominal aortogram and selective left ovarian artery angiogram demonstrating 2.5 cm pseudo-aneurysm of proximal to mid portion of the ovarian artery with adjacent contrast extravasation/hematoma.
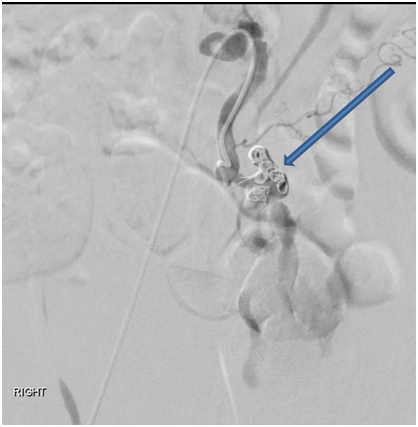
Figure 3B Pseudo-aneurysm was successfully embolized using 6, 8, and 10 mm nester embolization coils as well as Gelfoam slurry.
The patient remained hemodynamically stable after receiving a total of five units of packed red blood cells. A repeat contrast-enhanced CT abdomen and pelvis on postpartum day six showed a successful embolization of the left ovarian artery, and a persistent, large pelvic/retroperitoneal hematoma, without significant interval change in size. The patient was discharge home with a stable hemoglobin and hematocrit of 10.4 gm/dl and 31.4%. Five days after the discharge from hospital, the patient developed pulmonary embolism which was managed medically with rivaroxaban. She remained stable with the medical management of pulmonary embolism.
Postpartum retroperitoneal hematoma secondary to rupture of an ovarian vessel pseudo-aneurysm is a rare, life-threatening event.1 Its incidence is speculative because of the rarity of the condition with only 18 previously reported cases occurring in the perinatal period.1 The cases of retroperitoneal hemorrhage after vaginal delivery that have been reported in the literature include: uterine artery rupture on postpartum day three, right ovarian artery rupture on the second day after delivery and a splenic vein rupture on postpartum day one.2 This is the first ever case reported of postpartum retroperitoneal hematoma secondary to rupture of left ovarian artery pseudo-aneurysm after an uncomplicated spontaneous vaginal delivery that was treated with CT-guided percutaneous embolization and was further complicated by pulmonary embolism.
Postpartum retroperitoneal hematoma is characterized by bleeding from the injury to branches of the internal iliac artery into the retroperitoneal space resulting in severe hemorrhage and immediate hemodynamic instability. The maternal mortality rate has been reported as 49% and perinatal mortality as 31%; however, the rate may be lower with the improvement of blood banking and surgical techniques.3
The exact mechanism of rupture has not been established; however, there are several possible causes and associated factors cited in the literature. A pseudo-aneurysm is characterized by vessel dilatation and disruption of its wall leading to perivascular hematoma formation which may maintain communication with the parent vessel.4 Causes of pseudo-aneurysm rupture during/after delivery include: traumatic delivery, use of anticoagulation, manual removal of the placenta or extension of a vaginal hematoma.2 Hemodynamic and endocrine changes associated with pregnancy have been suggested to be contributing factors by causing alterations in the vessel wall, and forming new aneurysms or worsening existing aneurysms.5 Blood volume increases in pregnancy, which may lead to increased mechanical forces on the vessel wall. In regards to the hormonal changes, the increased levels of estrogen and progesterone can influence arterial wall remodeling, which predisposes to formation of aneurysms.6 Among all reported cases of rupture of ovarian artery aneurysm, 72% were associated with pregnancy and among these, 78% occurred in postpartum period. All of these patients were multigravida with the maternal age ranging between 23 to 39 years and rupture of the right side was more common.1
The diagnosis of retroperitoneal hematoma due to ruptured pseudo-aneurysm of an ovarian artery after normal delivery is often missed due to both the rarity of this condition and the fact that it usually presents with nonspecific signs and symptoms.7 Although the presence of small hematomas may be asymptomatic, most large hematomas present with pain, mass effects and hemodynamic instability. The diagnosis should be considered in a patient with persistent and acute-onset, severe abdominal, back or pelvic pain accompanied with a sudden drop in hematocrit. Ultrasonography is the first-line diagnostic test to rule out intraperitoneal or intrauterine bleeding. However, contrast-enhanced CT scan of abdominal and pelvis is the best imaging technique which can effectively reveal the diagnosis and aid in the management.8
Due to paucity of literature, the management guidelines are based on small cohort series or case reports. Fluid resuscitation, blood transfusion, correction of coagulopathy and intensive care monitoring are the mainstays of treatment. The definitive treatment of retroperitoneal hematomas is surgical intervention. However, for the hemodynamically stable patient, focus has recently shifted towards an endovascular approach by interventional radiology with percutaneous intra-arterial embolization or stent-grafting.8 Diagnostic aortography can be used to localize an actively bleeding vessel by visualization of extravasation of contrast and treatment is performed by creating a mechanical obstruction by using an embolic agent such as gelatin foam.8 Our patient was managed with transfusion of five units of packed red blood cells, serial hemoglobin and hematocrit measurements, and CT-guided percutaneous embolization of the left ovarian artery. Later on, she developed pulmonary embolism that was treated successfully with medical management. Possible factors in this case that could have contributed to pulmonary embolism might have been the large pelvic hematoma pressing on the pelvic vessels and stasis of blood in the hematoma.
Based on the presented case here, the diagnosis of retroperitoneal hematoma can be made by contrast-enhanced abdominal and pelvic CT and location can be identified by angiography. Even when the patient is hemodynamically unstable, close monitoring of the vital signs and serial measurements of laboratory parameters along with the percutaneous embolization of the identified vessel can be used as a management option.
We want to thank the patient for giving us the permission to write this case report and also Dr. Shafali Dumeer, MD for providing us the images of the patient.
None.

© . This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.