eISSN: 2377-4304


We describe a case of a unique pregnancy of 27 weeks of gestational age, the ultrasound examination revealed a large abdominal-thoracic wall defect and short umbilical cord. These ultrasound findings were diagnosed as Body Stalk Anomaly. The patient begins contractions spontaneously and by hysterotomy an alive baby was born and posteriorly, died in few minutes due to extreme preterm birth and multiple congenital anomalies. The final anatomopathological evaluation confirmed the diagnosis.
Keywords: body stalk anomaly, ultrasound scan, congenital abnormalities, abdominal wall
It is a poliformative syndrome, the abdominal wall defect and / or chest in which the umbilical cord may be totally absent or extremely shortened. Severe kyphoscoliosis is often present. It is common to find defects of the central nervous system or mielomeningocele.1
Possible causes of body stalk anomaly include early amnion rupture with direct mechanical pressure and amniotic bands, vascular disruption of the early embryo, or an abnormality in the germinal disk. The germinal disk abnormality is thought to represent complete failure of body folding along all three axes (cephalic, caudal, and lateral) during the sixth postmenstrual week. Normal body folding results in separation of the intraembryonic coelom (future peritoneal cavity) from the extraembryonic coelom, formation of the body stalk, and development of the umbilical cord. Aberrant cephalic folding leads to a defect in the thoracic wall and epigastrium, which allows development of ectopiacordis. Aberrant lateral folding results in herniation of the midabdominal contents into a large wide-based amnioperitoneal sac, which inserts peripherally onto the placental chorionic plate in lieu of an umbilical cord or with a very short umbilical cord.2
This is a patient 38 years old, a native of Lima - Peru, multigesta, last menstruation period dated at 9/15/14- with a history of two previous cesareans both of them with preeclampsia. She was first seen at 16 weeks in our hospital, the ultrasound scan shows in continuity of the front wall which protrudes liver, intestine and cord. It determined an omphalocele and potentially placenta previa.
03/18/15- Ultrasound monitoring at 27 weeks of gestation where described the previous thoraco-abdominal wall protrusion 4cm with visceral and cardiac mass (Figure 1) with pericardial effusion and ventricular septal defect, umbilical cord with 6.4 cm in length (Figure 2), direct fetal placental implantation, it is assumed therefore decreased fetal movement, placenta posterior fundus grade II, face seen unchanged (Figure 3), no abnormalities in upper and lower limbs (Figure 4), amniotic fluid index 35cm concludes: Pregnancy of 27 weeks and body stalk anomaly.3,4
The next day patient arrives to the Emergency Room with painful contractions and decreased fetal movements. On examination fetal heart rate is 110-113 and sporadic uterine contractions, deciding hospitalization.
During her hospitalization begins uterine dynamic, however it presented a urinary tract infection so treated with ceftriaxone 2g IV c/24h, 4th day after admission had again uterine dynamic, given the presence of urinary infection site and the persistence of uterine contractions, suspecting subclinical chorioamnionitis and risk of uterine rupture (history of 2 previous cesareans) decided finishing the gestation in maternal benefit.
03/23/14 - Hysterotomy: the newborn had multiple malformations, increased amniotic fluid volume without odor. Basic support measures to the newborn, who died minutes later (Figure 5).
Pathological examination reports
Female newborn, 932 grams, 34 cm in length, extrusion of the intraabdominal and thoracyccontents, defect in the wall where bowel loops protruding liver, heart, severe scoliosis and syndactyly of the 3rd and 4th finger of his right hand, no other abnormalities in extremities. Evidence of an umbilical cord 8cm in length with two arteries/one vein, Permeable anus (Figure 6-8).
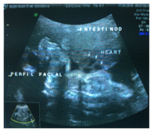
Figure 1 Ultrasound monitoring at 27 weeks of gestation where described the previous thoraco-abdominal wall protrusion 4cm with visceral and cardiac mass.
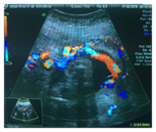
Figure 2 Ultrasound monitoring at 27 weeks of gestation with pericardial effusion and ventricular septal defect, umbilical cord with 6.4 cm in length.

Figure 3 Ultrasound monitoring at 27 weeks of gestation direct fetal placental implantation, it is assumed therefore decreased fetal movement, placenta posterior fundus grade II, face seen unchanged.
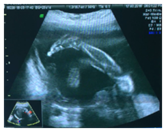
Figure 4 Ultrasound monitoring at 27 weeks of gestation with no abnormalities in upper and lower limbs.
Body Stalk Anomaly is rare; prevalence ranges from 0.4 to 3.2 per 100,000 live births and stillbirths. However, this range probably under-represent the true prevalence because it does not consider fetal loss due to miscarriage and pregnancy termination. For example, four cases among 6,952 ultrasound examinations of the nucal translucency performed at 11 to 14 weeks of gestation were observed in just one institution.5
Prenatal diagnosis of body stalk anomaly is usually done in a second ultrasound trimester. Although, the precocious diagnosis has improved thanks to ultrasound screening at 11-13 + 6 weeks.6,7 Criteria for diagnosis include ultrasound demonstration of internal organs in the extraembryonic coelom and a short or absent umbilical cord.8 In the second trimester, the diagnosis can be difficult because of coexisting oligohydramnios. The peritoneal cavity retains its extracelomic communication with the cavity, which extends to the margins of the placenta. This amnioperitoneal sac may contain portions of the lungs, heart, liver, spleen, intestine, kidney and bladder; among female fetuses may have herniation of the ovaries, fallopian tubes and uterus.9 There are no successful therapeutic interventions available to fetuses or newborns who suffer Body Stalk Anomaly.10,11 It`s known that it may have complications at birth when the mother decides to continue the pregnancy. Given that is a lethal anomaly and its potential implications for the safety of the mother, abortion is recommended when the diagnosis is fully established.12
In the case reported we were unable to perform abortion because it’s illegal, however, given the presence of urinary infection site and the persistence of uterine contractions, suspecting subclinical chorioamnionitis and risk of uterine rupture (history of two previous cesarean sections) we decided to finish gestation by maternal benefit.
In conclusion, it is important to distinguish a body stalk anomaly from other types of anterior abdominal wall defects because of their prognosis and an appropriate medical management. A body stalk anomaly is a sporadic defect and not associated with chromosomal abnormalities. This congenital defect is invariably lethal.

© . This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.