eISSN: 2572-8474


Review Article Volume 6 Issue 3
Department of Pharmacy, World University of Bangladesh, Bangladesh
Correspondence: Mohiuddin AK, Assistant Professor, Department of Pharmacy, World University of Bangladesh, 151/8, Green Road, Dhanmondi, Dhaka–1205, Bangladesh, Tel +8801716477485
Received: April 24, 2019 | Published: May 21, 2019
Citation: Mohiuddin AK. Patient behavior. Nurse Care Open Acces J. 2019;6(3):76-90. DOI: 10.15406/ncoaj.2019.06.00188
The most frequent causes of death in the United States and globally are chronic diseases, including heart disease, cancer, lung diseases, and diabetes. Behavioral factors, particularly tobacco use, diet and activity patterns, alcohol consumption, sexual behavior, and avoidable injuries are among the most prominent contributors to mortality. Projections of the global burden of disease for the next two decades include increases in noncommunicable diseases, high rates of tobacco-related deaths, and a dramatic rise in deaths from HIV/AIDS. Worldwide, the major causes of death by 2030 are expected to be HIV/AIDS, depressive disorders, and heart disease. At the same time, in many parts of the world, infectious diseases continue to pose grim threats, especially for the very young, the old, and those with compromised immune systems. Malaria, diarrheal diseases, and other infectious diseases, in addition to AIDS, are major health threats to the poorest people around the world. And, like chronic diseases, their trajectory may be influenced by the application of effective health behavior interventions. Substantial suffering, premature mortality, and medical costs can be avoided by positive changes in behavior at multiple levels. Most recently, there has been a renewed focus on public health infrastructure to plan for emergencies, including both human-made and natural disasters. During the past twenty years, there has been a dramatic increase in public, private, and professional interest in preventing disability and death through changes in lifestyle and participation in screening programs. Much of this interest in disease prevention and early detection has been stimulated by the epidemiological transition from infectious to chronic diseases as leading causes of death, the aging of the population, rapidly escalating health care costs, and data linking individual behaviors to increased risk of morbidity and mortality.
Keywords: health beliefs and perception, patient counseling, patient comprehension and recall, patient motivation, patient feedback, patient compliance
Patient behavior is often described as disruptive behavior as they have an altered mental stage of fear of being sick, anxious about out of the pocket cost, alteration of lifestyle if suffered from a chronic illness. And the outcomes often faced by providers are inappropriate language, make unreasonable demands, and may even resort to physical abuse. The article comprises a few of this unusual behavior and a simple comparison between patients from developed world with those of the under-developed east. Programs to influence health behavior, including health promotion and education programs and interventions, are most likely to benefit participants and communities when the program or intervention is guided by a theory of health behavior. Theories of health behavior identify the targets for change and the methods for accomplishing these changes. Theories also inform the evaluation of change efforts by helping to identify the outcomes to be measured, as well as the timing and methods of study to be used. Such theory-driven health promotion and education efforts stand in contrast to programs based primarily on precedent, tradition, intuition, or general principles. Theory-driven health behavior change interventions and programs require an understanding of the components of health behavior theory, as well as the operational or practical forms of the theory. The science and art of health behavior and health education are eclectic and rapidly evolving; they reflect an amalgamation of approaches, methods, and strategies from social and health sciences, drawing on the theoretical perspectives, research, and practice tools of such diverse disciplines as psychology, sociology, anthropology, communications, nursing, economics, and marketing. Health education is also dependent on epidemiology, statistics, and medicine. There is increasing emphasis on identifying evidence-based interventions and disseminating them widely. This often requires individual health education and health behavior professionals to synthesize large and diverse literatures. Evidence-based groups like the Cochrane Collaboration (http://www.cochrane.org) and the CDC’s (Centers for Disease Control and Prevention) Guide to Community Preventive Services (http://www.thecommunityguide.org) offer regular syntheses of behavioral interventions, some of which include theoretical constructs as variables in analyses of effectiveness.
Purpose of the study: Discussion and projection of behavior pattern, health seeking behavior and monitoring status in both developed and under-privileged countries. The pharmacists have a vital role to play which is discussed along with comparison.
Findings: Developed or under developed country, patients have a separate behavior pattern which develops and worsen with disease progression mostly. So many factors are behind but one thing clearly understood that the handling of such situation is a provider’s function, a challenge they have to face along with treatment intervention.
Research limitations: Very few articles found in matters regarding along with a very less interest paid by general people to talk about healthcare matters. It was very difficult to bring out facts of irrational patient behavior, giving it a substantial figure to discuss in this article. However, the major limitation is the article could be a comparison of behaviors of developed and under-privileged countries which requires an enormous exposure and financial support. However, the sole focus was to detail mysterious patient behavior and a greater part is covered.
Practical implication: The soul of this article was to detail about patient behavior, both in Bangladesh and developed countries. Along with students, researchers and professionals of different background and disciplines, eg. Pharmacists, marketers, doctors, nurses, hospital authorities, public representatives, policy makers and regulatory authorities have to acquire much from this article.
Social implication: Patient behavior is the Sole of healing system and a scope for pharmacists and other healthcare providers to work with in both developed or under developed countries. The article should contribute an integrated guideline for patient compliance, demand rational behavior and last but not the least a silvery lining to better pharmacists’ dealings with them in near future.
Over the past two decades, research programs have been established to identify and test the most effective methods to achieve health behavior change. More precise quantification of personal health behaviors and improved health outcomes has grown from partnerships between behavioral scientists and biomedical experts. During this period, findings from some major health behavior intervention studies have become available and have provided important insights for the field. Professionals charged with responsibility for health education and health behavior are, by and large, interventionists. They are action-oriented. They use their knowledge to design and implement programs to improve health. This is true, whether they are working to encourage health-enhancing changes in individual or community behavior or conditions. It is equally true of most health education and health behavior research. Often, in the process of attempting to change behavior, environments, or policies, researchers must do precisely what practitioners do–develop and deliver interventions. At some level, both practitioners and researchers are accountable for results, whether these are measured in terms of participants’ satisfaction with programs, or changes in their awareness, knowledge, attitudes, beliefs, or health behaviors, or in their improved decision making; institutional norms; community integration; or more distal results, including morbidity, mortality, and quality of life. Health educators may assess these results anecdotally, complete in-depth qualitative assessments, or conduct rigorous empirical evaluations. The unusual patient behavior toward providers and towards themselves including medication taking is inevitable. An interesting fact is mostly patients avoid going to visit a doctor or pharmacists and when appeared for treatment their behaviors change dramatically which is still unexplained. A National Health Service survey reveals 30% patients never seek any care due to emotional distress of being ill and again nearly 60% fail to comply treatment guidelines as directed. Social phobia persists in women who need to go for an intervention for any gynecological disorder. Conversely, children have phobia with the doctors and hospital settings due to some unknown reason. When came late at an advanced disease state, the patient is already in a highly disturbed mental condition and a few situations raise, providers need to face another challenge to tolerate and mitigate them. Practitioners of health education at once benefit from and are challenged by the multitude of theoretical frameworks and models from the social sciences available for their use, because the best choices and direct translations may not be immediately evident. The inherent danger in a book like this is that one can begin to think that the links between theory, research, and health promotion practice are easily forged. They are not. For the unprepared, the choices can be overwhelming, but for those who understand the commonalities and differences among theories of health behavior and health education, the growing knowledge base can provide a firm foundation on which to build.
Research design and search strategy
The research is conducted through secondary data search from several sources from books, technical newsletters, newspapers, journals, and many other sources. The present study was started from the beginning of 2018. PubMed, ALTAVISTA, Embase, Scopus, Web of Science, and the Cochrane Central Register of was thoroughly searched. The keywords were used to search for different publishers’ journals like Elsevier, Springer, Willey Online Library, Wolters Kluwer were extensively followed.
Inclusion and exclusion criteria
Studies regarding psychological and social behaviors were given priorities. Several factors that influence medication taking behavior was collectively analyzed and added to the article. Issues regarding economic and cultural barriers were found to be different from subcontinents, countries and even states. A few interesting features of patient motivation and satisfaction through pharmacist’s intervention were added afterwards to maintain a logical sequence. Drug factors, environmental factors and provider-patient interaction followed by pharmacist’s role in handling patients and to change or correction of behavior were added to reveal their effect on patient compliance which is the ultimate goal of therapeutic guidelines. Many studies found regarding patient compliance of different health conditions in different countries found to be not within the scope of this article.
Types of medication taking behavior
Types of patient behavior
The strands of health behavior are positive or negative health life styles and risk avoidance whereas the sub - concepts of illness behavior is health - seeking behavior, help-seeking behavior, healthcare seeking or treatment seeking behavior, the sick role behavior, and life experiences of living with acute or chronic conditions:
Preventive Health Behavior |
To keep oneself away from health hazards and prevent from possible ailment. This includes actions like immunization, exercise, intake of healthy foods and avoid smoking. Three factors converge to underscore the heightened importance of preventive health care services among United States adults. First, there is the rapidly aging population. Second, there is the rising cost of medical care: chronic illnesses and end-of-life issues that older adults face is expensive. Third, despite spending more on health care than any country in the world, United States adults generally have poorer health and lower life expectancies than those in other developed countries. |
Detective Health Behavior |
This kind of health behavior is manifested when individuals engage in active medical screening to detect or identify the real or potential risk of getting caught by any disease. Usually the detection is carried out before perceiving symptoms of any disease or in other words at the asymptomatic stage. Many hospitals or voluntary health organizations develop programs of detection of possible risk factors by engaging certain target populations into their mass screening programs. |
Health Promotion Behavior |
To undertake certain healthy activities and adopt healthy life styles to maintain and promote existing health conditions. The health promotion can also be achieved through preventive health behavior. According to the WHO, there will be 1.2 billion elderly people around the globe by 2025 and 2 billion by 2050. Performing health promotion behaviors is one of the best ways for people to control their health. |
Health Protective Behavior |
Health protective behaviors are receiving increasing attention for maintaining health and preventing disease. At least 60% of the burden of diseases around the world is due to unhealthy lifestyles, according to WHO reports. The harm of unhealthy lifestyle activities such as smoking, excess alcohol and fat consumption, lack of exercise, and chronic exposure to |
Exhibit 1 Types of health behavior5–11
The concept of sick role was proposed by an American Sociologist Talcott Parsons in his famous book ‘the social system’ which published in 1951.
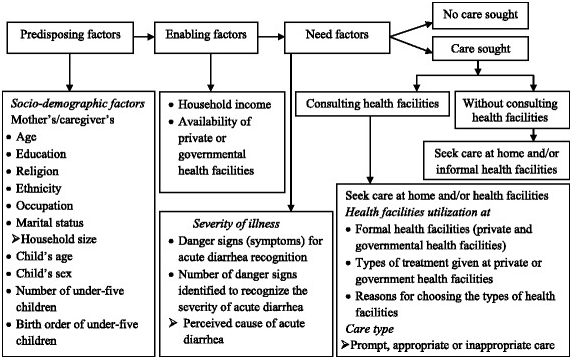
Figure 1 Conceptual framework for health-seeking behavior modified from Andersen’s behavioral model,6 which is widely accepted and used to study the predictors of health-seeking behavior and health facility utilization for various diseases, including childhood diarrhea in slums of Addis Ababa, Ethiopia.
Model of Health Services Utilization suggested that three main factors affect an individual’s use of health services:
Patient factors
Drug factors
Drug regimens can be complex. The complexity of a drug regimen often is measured in the:
Medications may require special behaviors, for example:
Environmental factors
Patients given more autonomy and opportunities for self-determination tend to show greater health and morale improvements. The structural layout of many community pharmacies does not include an area for private consultation and dialog between the patient and the pharmacist. In addition to this lack of privacy, pharmacists often experience other environmental barriers to meaningful interaction with their patients, including
Provider patient interaction
Patients can play an important role in improving patient safety by becoming actively involved in their health care. Patients can act as ‘safety buffers’ during their care but the responsibility for their safety must remain with the health care professionals.41 Clinical practice often fails to optimize patient participation in decisions about serious illness. Patients prefer that the physician have most of the control over decisions.42,43 Patients use three main sources of information when making decisions about their illness and treatment:
The patient-clinician relationship has both emotional and informational components – termed emotional care and cognitive care.44 Emotional care includes mutual trust, empathy, respect, genuineness, acceptance and warmth.45 Cognitive care includes information gathering, sharing medical information, patient education, and expectation management. Providers who adopt an autocratic approach assume a dominant or controlling role, speaking with an authoritarian tone and giving directions without seeking patient input. In contrast, providers who adopt a participatory approach collaborate with the patient to develop a mutually acceptable treatment plan, providing decisional support or guidance without ignoring patient views and demanding compliance with a certain therapeutic plan.46
It is estimated that close to half of the U.S. population has limited health literacy. |
According to the Center for Health Care Strategies (CHCS), LHL and insufficient patient education can cost up to $236 billion every year. |
LHL is associated with multiple adverse outcomes including rates of hospitalization and mortality. |
Patients with LHL are more likely to have poor health status, higher rates of hospitalization, and a nearly twofold higher mortality rate. |
They are also more likely to experience disparities in health and health care access, have lower rates of screening and preventive services, and obtain their care in the emergency department. |
§ Furthermore, patients with LHL are more likely to have poorer knowledge about their disease processes, medication regimens, and methods for managing their disease. LHL also has a negative effect on doctor-patient communication. |
The difficulty and length of informational materials can interfere with the patient’s ability to comprehend and recall advice. |
In general, patients have fewer difficulties if providers simplify instructions by avoiding medical jargon and using shorter words and sentences. |
In fact, the patients who received the difficult leaflet made nearly the same number of medication errors as those who received no information. |
Amelioration of health literacy of the caregivers will have a direct effect on patient health and prevention of complications. |
Knowledge of potential barriers to understanding and completion may improve utilization of and accuracy of patient responses to PFDI-20 and PFIQ-7 (US grade level questionnaire) in women with LHL. |
LHL patients did not appear to derive a greater advantage from multimedia, computer-based approach to improve knowledge, attitudes, self-efficacy, and receptivity to cancer clinical trials. |
LHL is associated with challenges for those living with HIV including medication non-adherence and poorer health outcomes. AMSTAR checklist by Reynolds et.al., 2019 reveals all of the studies addressed the key significance of health literacy within the scope of living with HIV disease. |
Exhibit 2 Patient Low Health Literacy (LHL) and Healthcare49–57
Being ill and undergoing treatment can involve
Surveys suggest that patients experience a wide variety of subjective and objective problems and concerns that contribute to nonadherence, dissatisfaction with care, and treatment dropout. These barriers to treatment adherence include ~
At the same time, physicians and pharmacists do not always ask patients about their medication concerns, beliefs, understandings, and behaviors. While these patient concerns can have detrimental effects on the patient’s behavior, many patients are reluctant to complain or ask their providers about their medications. Providers who ask carefully designed, open-ended questions about patient concerns and adherence will be more likely to receive accurate patient feedback than those who wait for their patients to volunteer this information. community pharmacists should equip themselves with appropriate knowledge and competencies in order to tender efficient and outstanding pharmaceutical health care.61,62
As reported by the WHO, patient adherence to long-term therapies is alarmingly low in both developed and developing countries.63 Nearly 50% of antibiotics are purchased and consumed without any medical supervision in most parts of the world.64 Evil spirits are blamed for epilepsy in most part of the world. Healthcare providers’ understanding of their patients’ healthcare beliefs, values, and preferences is an important feature of patient-centered care. The use of herbal medicinal products and supplements has increased tremendously over the past three decades with not less than 80% of people worldwide relying on them for some part of primary healthcare.65 Medication nonadherence remains a substantial public health problem. Worldwide, between 25% to 50% of patients do not take their medications as recommended. In the USA, suboptimal adherence has been associated with 125,000 deaths, 10% of hospitalizations, and costs 300 billion USD annually.66 The economic impact was also in PubMed and Scopus in September 2017, which shows an increase in total healthcare cost (>80%), pharmacy costs (70%), inpatient and outpatient costs (50%), emergency department visit and medication costs (<30%), and hospitalization costs (<20%).67 Across South Asia, overall hypertension prevalence is estimated to be 27%. Prospective Urban Rural Epidemiology study has shown more than 50% are unaware of it and up to 80% of hypertensive patients have low adherence to medication.68 Uncontrolled BP was found more than 50% in Bangladesh, 70% in Pakistan and almost 60% in Sri Lanka.69 American Diabetes Association and the European Association for the Study of Diabetes guidelines in 10 developing countries from Africa (Egypt, South Africa), Middle East (Israel, Saudi Arabia, United Arab Emirates, Iran and Lebanon) and South Asia (Bangladesh, India and Pakistan) shows more than 25% and around 70% patients did not have any follow-up visit by a diabetologist or a GP, respectively. More than 35% patients did not receive any diabetes education.70. Lifestyle risk behaviors such as smoking, poor diet, lack of exercise and alcohol misuse contribute to a substantial burden of disease and disability worldwide. In the UK, around 70% of people engage in at least two of these behaviors.71 In the US, 78.6 million people, being obese and the estimated annual cost of obesity reaching approximately $147 billion.72 AUD was reported in nearly 30% in rural India73 and SLT followed by smoking and dual use of tobacco (paan, paan masala, khaini, zarda and gutka) in nearly 50%.74. In 2015, along with China, India recorded the highest number of obese children globally.75
Health expenditure and utilization in western countries
Misbeliefs, superstitions and poor compliance in south asian countries
In Pakistan, 10% ethnic respondents rely on arm bracelet for pressure control and neem (Azadirachta indica) for diabetes measure; nearly 30% rely neem chicken pox and measles cure; 16% went to maulvis for treatment of jaundice; for epilepsy management, 20% of patients were made to smell shoes and 11% were taken to peers and faqirs (folk healers).80 “Coining”, a similar belief in China, Indonesia and many South Asian countries that rubbing coin along with the skin will bring bad blood to surface. Culturally in many parts of India, menstruation is still considered to be dirty and impure. A nearly 90% of women in India sometimes resort to using ashes, newspapers, dried leaves and husk sand to aid absorption.81 The trend towards finding healers first and then doctors covers all fields of medicine in India and beyond. It cannot be wrong to show respect for cultural traditions and belief, but if pursued without heed to possible harms that arise from not seeking timely professional help the situation could change. Furthermore, the situation described is not unlike that which is commonly found in China, where the two different types of medicine (traditional and allopathic) generally work in parallel, and have done for many years. In Bangladesh, diarrhea and pneumonia cause death of more than ten lac children every year. Majority parents seek treatment from homeopaths, folk healers, retailers or non-qualified allopath.82 A recent study shows that half of the antibiotics are sold without prescription in most of the South Asian countries, people prefer self-medication rather than visiting a doctor.83
Pharmacists role in improving patient behavior
Importance of patient counseling
Patient counseling is necessary to reduce medication errors and improve patient healthcare (Figure 2). This leads to several potential benefits:
Potential for decreased health care costs due to appropriate use of medications and prevention of adverse events. The pharmacist also benefits in this process. Potential benefits to the pharmacist in this process include:
In short, it ensures positive outcomes on the management of disease, including improved drug compliance, better treatment endpoints, and patient satisfaction.2 Approaches aimed at promoting patient and family engagement in treatment share the over-arching goal of changing behaviors of patients, families, and healthcare providers and possibly administrators. Patient engagement interventions are complex by nature and involve interacting components intended to produce changes in outcomes and behavior.86,87 Michie et al.86 have generated a taxonomy of 93 BCTs in 16 categories (Table 1) that can be used to specify, interpret, and implement specific techniques used in patient and family engagement approaches.
BCT category |
Example and definition |
Goals and planning |
Problem solving: analyze or prompt the person to analyze factors influencing the behavior and generate or select strategies that include overcoming barriers and/or increasing facilitators |
Feedback and monitoring |
Feedback on behavior: monitor and provide information on evaluative feedback |
Social support |
Social support (practical): advise on, arrange, or provide practical help for the performance of the behavior |
Shaping knowledge |
Instruction on how to perform the behavior: advise or agree on how to perform the behavior |
Natural consequences |
Information about health consequences: provide information (written, verbal, visual) about health consequences of performing the behavior |
Comparison of behavior |
Information about others’ approval: provide information about what other people think about the behavior |
Associations |
Prompts/cues: introduce or define environmental or social stimulus with the purpose of prompting or cueing the behavior. |
Repetition and substitution |
Behavioral practice/rehearsal: prompt practice or rehearsal of the behavior one or more times in a context or at a time when the performance may not be necessary in order to increase habit and skill |
Comparison of outcomes |
Pros and cons: advise the person to identify and compare reasons for wanting and not wanting to change the behavior |
Reward and threat |
Social incentive: inform that a verbal or non-verbal reward will be delivered if and only if there has been effort and/or progress in performing the behavior |
Regulation |
Conserving mental resources: advise on ways of minimizing demands on mental resources to facilitate behavior change |
Antecedents |
Restructuring the social environment: change or advise to change the social environment in order to facilitate performance of the wanted behavior or create barriers to the unwanted behavior |
Identity |
Framing/re-framing: suggest the deliberate adoption of a perspective or new perspective on behavior (e.g., its purpose) in order to change cognitions or emotions about performing the behavior |
Scheduled consequences |
Situation-specific award: arrange for reward following the behavior on one situation but not in another |
Self-belief |
Verbal persuasion about capability: tell the person that they can successfully perform the wanted behavior, arguing against self-doubts and asserting that they can and will succeed |
Covert learning |
Vicarious consequences: prompt observations of the consequences (including rewards and punishments) for others when they perform the behavior |
Table 1 Overview of patient behavior change techniques103
Benefits of patient compliance
The improvement of compliance (Figure 3) will result in a situation in which all parties benefit. Most importantly patients benefit from the enhancement of the efficacy and safety of their drug therapy.88 Pharmacists benefit because there is an increased recognition and respect for the value of the advice and service that they provide. Pharmaceutical manufacturers benefit from the favorable recognition that accompanies the effective and safe use of their drugs as well as from the increased sales resulting from the larger number of prescriptions being dispensed. Finally, society and the health care system benefit as a result of fewer problems associated with noncompliance. Although an increase in compliance will result in more prescriptions being dispensed and a higher level of expenditures for prescription medications, this increase in costs will be more than offset by a reduction in costs (e.g., physician visits, hospitalizations) attributable to problems due to noncompliance.89,90

Figure 3 Compliance monitoring.88 An increase in the accessibility of health system data and advancements in electronic information of medication use has permitted new insight into patients’ medication behavior. The increased availability of big data in health has enabled the utilization of quality performance measurement across various aspects. Specially, in pharmacy, large data sets of prescription dispensing information, also known as pharmacy claims or prescription refill data, have become more readily available from the ease of electronic information, making it useful for analyzing medication adherence and providing a viable and economical approach for its estimation in real time. Frequently revealed in long-term monitoring are declining trends in adherence, indicating the issue of maintaining adherence over time as crucial as improving adherence at a cross-sectional time point. Instant feedback during the dispensing process can allow the monitoring of patient adherence in real-time, especially by community pharmacists, and therefore, trigger adherence interventions when suboptimal adherence levels are identified. Interventions to improve medication adherence in research projects delivered by community pharmacists have been shown to be more effective.
Conflict resolution and problem solving
Because providers and patients are likely to have different viewpoints and agendas, some interpersonal conflict or disagreement is inevitable during their interaction. This conflict is especially likely after patients have gained more experience with their illness and recommended treatments. For example, providers may want patients to comply as fully and rapidly as possible with their ideal treatment plan, whereas patients may prefer a slower or less aggressive approach or even request alternative therapies that providers would consider ineffective, inappropriate, or unnecessary. Providers also may consider certain side effects or drug-taking problems to be clinically insignificant or trivial, while patients consider the same side effects or problems to be intolerable. As a result, providers often are confronted with both explicit and subtle forms of negative feedback from their patients (Figure 4) (eg, complaints about the drug or dosage schedule, admissions of nonadherence, reported difficulties administering or paying for medication, expressions of fear and uncertainty about drug efficacy or safety). In contrast, the participatory/collaborative approach involves acknowledging the legitimacy of patient concerns, assessing patient concerns in a more thorough and respectful manner, tailoring or adjusting drug regimens to fit patient routines and preferences, and negotiating mutually acceptable solutions. Patient adherence is significantly improved if the dosage schedule has been tailored to the patient’s daily routine, if the patient is allowed to change the regimen within a preapproved protocol, and if the patient identifies the areas in which he or she would like assistance.91,92
Managing disruptive patient behavior
Patient aggression/disruptive behavior toward healthcare professionals is common and worldwide. These include continual pacing, increasingly agitated appearance, abusive behavior (physical or verbal), obstructing the provision of care, refusing to comply with physicians’ orders or caregivers’ efforts to provide care, providing erroneous information on purpose, talking loudly or in an intimidating, confrontational, or disrespectful way, making unreasonable demands or using inappropriate language, taking unauthorized drugs or drinking alcohol while on hospital property, leaving the facility without proper authorization, purposely missing treatments or not following through on tests ordered etc.93 In 2010, Warren Davis shot his mother’s orthopedic surgeon before killing his mother and himself after he learned that back surgery had left his mother paralyzed. In 2014, a strikingly similar situation occurred at Sacred Heart Hospital in Cebu City, Philippines, when a wheelchair-bound patient, who was upset about not being able to walk after spinal surgery, shot and killed his orthopedic surgeon before killing himself.94 These behaviors have been linked to adverse events, medical errors, compromises in patient safety, and even patient mortality.95 For example, among trainees in seven Canadian residencies, Cook et. al found that 50% of participants reported psychological abuse by patients, with 10 to 15% reporting physical assaults by either patients or family members.96 In the June 2013 American Nurse Today, 5.6% of Emergency Department (ED) nurses are victims of violence daily, and over 28% of ED nurses experience verbal abuse.97 One study conducted by researchers at the Portland, Oregon Veterans Administration (VA) Hospital found that 30% of disruptive patients filed formal complaints about their care to outside third parties. Also, psychiatrists there found that 25% of patients who were disruptive caused 38% of the incidents that had been reported. In addition, they noted that disruptive behavior often escalated into more violent behavior.98 (Exhibit 3,4)
Consistent enforcement of the Code of Conduct, regardless of status or seniority (i.e. zero tolerance for violations) |
Monitoring patients’ perceptions of ongoing communications |
Assessment of any reports of patients’ disruptive behavior or violence, unprofessional staff behaviors, and any actual abuse or allegations of abuse and/or physical harm that may have resulted from altercations |
Development of an interdisciplinary process for addressing adverse events/trends related to unacceptable communication and/or disruptive behavior |
Medical staff members need to be included |
Representatives from key clinical and nonclinical departments should participate, including human resources and educators |
Executive leadership involvement is important |
Implementation of additional strategies to promote further improvements in communication styles and to reduce future patient/family/caregiver misunderstandings and frustrations |
Recognizing patient anger increases safety for both physicians and patients. |
Anger, in itself, has a differential diagnosis that physicians should keep in mind. |
B |
Believe |
Patients expect to be believed, and belief conveys understanding, support, and empathy. Empathy, the ability to comprehend and communicate understanding of another’s emotions and their attached meanings, is highly beneficial in complaint resolution and is fundamental to good doctor-patient relationships. |
L |
Listen |
Active listening requires that the clinician silence his/her inner voice and calmly and patiently attend to the patient without reacting or preparing a rebuttal. Within limits, tolerate anger, rudeness, obscenities, fabrications, exaggerations, personal criticism, histrionics, and repetition. Calmly give the patient his/her uninterrupted “magic minute” to describe, explain, criticize, and vent while conveying a sincere interest in hearing the patient. This is facilitated by sitting and facing the patient with an open, relaxed posture; making eye contact, and offering expressions of understanding. Maintaining a quiet mind, emotional control, and attentive posture demonstrates that the clinician is unrushed and empathetic. |
A |
Apologize |
The doctor then offers an apology for what the patient is experiencing and for his/her unmet expectations. This apology need not be an expression or acceptance of responsibility. Patients with legitimate complaints deserve an apology, those without legitimate complaints still expect one, and a well-worded apology further defuses the situation. This is why restating patients’ complaints in terms of unmet expectations is useful. The apology is an avenue for providing explanations without appearing defensive or accusatory. |
S |
Safety |
The clinician then strives to satisfy the patient. If the patient’s suggestions are reasonable, the clinician can simply accede to them. Otherwise, calmly explain why they may not be the best choice,13 propose two or three options (any more is potentially confusing), and let the patient choose. This gives the patient a sense of involvement and control. When the patient has chosen and the details explained, be certain to verify that the patient is satisfied with the solution. |
T |
Thank |
Finally, thank the patient for expressing his/her complaints and concerns and providing a second chance to satisfy him/her. Then follow up either by telephone or at the next visit to further demonstrate concern for what upset the patient and ensure satisfaction with the outcome. |
Exhibit 4 BLAST Approaches to Complain Resolution99
The health collaboration model
Health Collaboration Model highlights the central role of patient feedback and collaborative problem solving in health care. Each box represents a different set of provider behaviors or background factors affecting the collaboration process; whereas, each circle represents a different set of patient cognitions, beliefs, behaviors, or clinical outcomes affected by collaboration and background factors.100 Health Collaboration Model highlights the central role of patient feedback and collaborative problem solving in health care. The diagram is best understood by beginning at the left side of the diagram and following each arrow in numerical order. Each box represents a different set of provider behaviors or background factors affecting the collaboration process; whereas, each circle represents a different set of patient cognitions, beliefs, behaviors, or clinical outcomes affected by collaboration and background factors101 (Figure 5).

Figure 5Health collaboration model.102
The top part of the model (arrows 1–5) emphasizes the various factors that can impact the patient’s initial reactions after receiving a new prescription or other new regimen; whereas, the bottom part of the model (arrows 6–13) emphasizes the various factors that can impact the patient’s behavior after he/she has experienced the drug and barriers to adherence. First, we see that patient, provider, drug, and environmental factors (arrow 1) can impact both provider and patient behavior during the initial stages of collaboration and treatment, including the quality of provider instruction and support, patient comprehension/ recall and motivation, and initial patient adherence and barriers to adherence. During the initial stages of collaboration, the provider plays a critical role in facilitating and verifying patient comprehension/recall of the regimen (arrow 2). The provider also plays a critical role in facilitating and verifying the patient’s initial motivation and satisfaction with the regimen (arrow 3). It is not enough to give drug information. Rather, the provider must assess the individual’s initial understandings and beliefs and make adjustments as necessary. In some cases, he/she will need to provide additional instruction or reinforcement to make sure the patient will understand and remember the dosage schedule. In other cases, he/she will need to provide additional informational, social, or technical support to address the individual’s initial doubts or concerns about the drug and its short-term or long-term effects. If effective collaboration occurs at this stage, then the patient will have greater comprehension/recall and greater motivation which, in turn, lead to greater initial adherence and fewer barriers to adherence (arrows 4–5). The bottom part of the model draws attention to the fact that patients actively monitor their reactions to drug therapy and experience a variety of barriers to adherence after initiating therapy. They may find it difficult to remember each dose or simply question whether the drug is still needed or working for them. They also may experience unwanted effects or have concerns about high drug costs, possible dependence, or unknown long-term effects. Since these patient-perceived barriers seriously undermine the patient’s willingness and ability to continue therapy as prescribed, patient feedback plays a central role in follow-up visits with the provider (Figure 1). Soliciting accurate patient feedback is a complex process that depends on: the patient’s personal experience with the drug (arrow 6); background characteristics and expectations of the patient and provider, characteristics of the drug and environment, and past patient-provider interactions (arrow 7); and quality of provider monitoring. Providers who regularly ask carefully designed, open-ended questions in a supportive, non-accusatory manner can be very successful in soliciting negative patient feedback even among patients who initially appear reluctant or hesitant to share their personal doubts, difficulties, and concerns. The provider who is able to solicit accurate patient feedback is then able to resolve patient-specific problems and provide appropriate reinforcement as necessary (arrows 9–10). This type of two-way communication and collaborative problem-solving leads to greater patient satisfaction and adherence (arrow 11) and enhanced treatment outcomes (arrow 12). The final arrow (14) illustrates the importance of past interactions and treatment experiences in establishing and maintaining a trusting relationship that is the cornerstone of effective health and pharmaceutical care.
Health collaboration model can play an important role in pharmacy practice and research:
The comparative study shows different perspective of patient behavior in modern world and in Bangladesh. Reasons are found to cultural and economic differences. Pharmacists and other healthcare providers also have different strategies to promote patient behavior change, spent times with patients. High patient activity change support system should validate their efficiency and professionalism. But reality is that no graduate pharmacist is working in retail pharmacies or Government hospitals of Bangladesh except very few tertiary private hospitals. To attain the ideal healthcare service doctor, pharmacist, nurse and other healthcare professionals must work together. It is noteworthy to mention that any interruption in the team work will disrupt the whole health system and patient care service will never be achieved. At the same time, physicians and pharmacists do not always ask patients about their medication concerns, beliefs, understandings, and behaviors. While these patient concerns can have detrimental effects on the patient’s behavior, many patients are reluctant to complain or ask their providers about their medications. Providers who ask carefully designed, open-ended questions about patient concerns and adherence will be more likely to receive accurate patient feedback than those who wait for their patients to volunteer this information.
Patients today are considered to be thinking, able decision makers who can play an important role in the treatment process. Because patients are now recognized as active individuals, more attention is being paid to ways of restoring health or slowing illness progression through improved provider-patient communication and patients’ involvement in their own treatment. Emphasis therefore is placed on a range of patient treatment behaviors including sharing beliefs and expectations, asking questions, adhering to regimens, using home monitoring devices, keeping appointments, identifying and reporting side effects and drug-taking problems, and other valuable forms of communication that are necessary in contemporary health care.
It’s a great honor and gratitude to be pharmacists in research and education process. All pharmacists, officials, journalists, magazine analysts and associates that I met in this purpose, were very kind and helpful. I’m thankful to Dr. Mamun Rashid, Assistant Professor of Pharmaceutics, Appalachian College of Pharmacy Oakwood, Virginia for his precious time to review my article and for his thoughtful suggestions. I’m also grateful to seminar library of Faculty of Pharmacy, University of Dhaka and BANSDOC Library, Bangladesh for providing me books, journal and newsletters. The greatest help was from students and colleagues who continually supported me in collection and data extraction from books, journals, newsletters and precious time in discussion followed by providing information on different types of cosmetics in use. A portion of this article is long been lectured as course material. So, it is very much helpful for me to deliver better than before as many more things are studied.
Ethics approval and consent to participate: Animal and Human experiment: N/A, Human Data Submission Approval: N/A
Consent for publication: Consent to publish Individual Person’s data: N/A
Availability of data and materials: Data sharing: Data will be provided on request.
Funding: Funding from individual/Organization: No fund received from any individual/organization.
Authors’ contributions: The individual contributions of authors: N/A.
The author declares that he has no conflict of interest.

©2019 Mohiuddin. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.