eISSN: 2574-9927


Mini Review Volume 5 Issue 4
Department of Mechanical Engineering, Dhaka University of Engineering and Technology, Bangladesh
Correspondence: Md. Shahinoor Alam, PhD Research Student, Department of Mechanical Engineering, Dhaka University of Engineering and Technology, Gazipur, Gazipur-1707, Bangladesh, Tel +8801715009804
Received: June 02, 2021 | Published: July 14, 2021
Citation: Alam MS. Tribology in recent biomedical engineering: a review. Material Sci & Eng. 2021;5(4):103-109 DOI: 10.15406/mseij.2021.05.00165
Generally, tribology includes three key topics: friction, wear, and lubrication. As humanity progresses, tribology continues to make vital contributions in addressing the demands for advanced technological developments, resulting in increasing machine durability and improving the quality of life. At the point when organic systems particularly human joints for example knees, hips, and so forth which constantly move concerning each other, tribology moves toward becoming bio-tribology. Various essential bio-tribological testing phenomena can significantly influence the result of wear for the implant design and material selection. The study also found the different types of frictional losses in bio-tribology and prevention of these losses. The application of tribology in dentistry is also a growing and rapidly expanding field. In restorative dentistry, metals and alloys and ceramics and composites are generally applied to restorations and implants. The complex inter-oral environment and biomechanics, make the wear processes of artificial dental materials are very complicated and normally include abrasion, attrition, corrosion, fretting wear, and fatigue. These processes occur in various combinations to cause surface loss of materials in the mouth. Intensive research has been conducted to develop an understanding of bio tribology for the successful design and selection of implants and artificial dental materials. This study is carried out to improve the knowledge about bio-tribology and thereby guide the researchers to get their future research directives.
Keywords: bio-tribology, bio-materials, hip joints, dentistry, polymer in orthodontics, implant
Tribological losses mainly indicate the frictional and wear losses. In bio-tribological applications like hip joints, even though tribological marvels are across the board in regular day-to-day existence, the word tribology is not familiar to many people. As such to present the demanding significance of tribology, it is very much usual to explain tribology before talking about tribology to no knowledge. The term tribology originates from the Greek words tribes means rubbing/erosion and logos means science. So it is characterized as the science of rubbing surfaces. At the end of the day, it is known as the art of interfacing surfaces in relative movement and includes numerous ideas, for example, erosion, wear, and lubrication. As such, tribology is in the tire moving over the road, in the head-circle interface of a hard plate driver, in the flashing of the eye, and so on. Tribology plays a significant role in designing and in the creative world and our everyday life, similarly bio-tribology. Recently green tribology has additionally received critical consideration with special attention to our surroundings and energy consumption.1–5 Bio tribology is mainly discussed with entire parts/limbs related to the biological network. It is the most probable area to enrich the tribological concept with bio tribology.1,6–9 Many biological network or system depends on the tribological framework. In this regards bio tribology dealing system should be more emphasized to the use of mechanical parts to the human body and so on. In medical science, the application of bio-tribology is closely interconnected to the human body, and equipment used particularly in different types of joints is more important. Human joints functioning needs to improve when to damage these joints and also in older age situations. Against this backdrop, this paper primarily deals with building a tribology concept and finding the causes of materials used to the human body joints. Secondly, it discusses the mechanism and how to improve the performance of replaced materials. Finally, the future scope of the study is discussed.
In this study, some recent papers on bio-tribology are reviewed for finding their outputs, materials, and methods used. Gulsen, Merve, and Meltem et al., worked on bio tribology of ligament wear in the knee and hip joints survey of present improvements.10–21 This review article aimed to provide an overview of in-vitro studies at the theoretical and laboratory conditions that must be performed before clinical investigation. In the experiment, utilizing the essential standards of tribology and utilizing new techniques that would be utilized in the field of bio-tribology are investigated. Fake joints outlined utilizing different materials, for example, metals, earthenware production, polymers, and composites were considered. New examinations here influenced the improvement of embed innovation. Diverse amalgams or composites were being tried for new embed outlines. Moving inserts with a danger of wear were tried in research center conditions in test system gadgets before they were utilized in the human body. Rokaya, Srimaneepong, Sapkota, Qin, Siraleartmukul & Siriwongrungson et al., studied the article entitled 'Polymeric materials and films in dentistry: A review13,14 Mainly it discussed the use of polymeric materials and polymeric films in making medicine and dental purpose.23–25 The variety of polymeric applications in dentistry and its limitations as well as benefits are also included.15–22 In future guidelines of this review, polymeric usage for more studies was emphasized for better treatment activities.
Sekuła and Zuba‐Surma reviewed 'Biomaterials and Stem Cells: Promising Tools in Tissue Engineering and Biomedical Applications.31–33 Recently biomaterials are used in different parts replacements and also to increase the functional ability of the human body. Cell-based therapy included for clinical improvements. But biomaterials and cell-based therapy weren’t discussed in a better solution, where it needed more accuracy and advanced precaution. Groves, Fisher, and Williams et al., worked on an in vitro reenactment technique for the tribological evaluation of full natural hip joints.34–39 The fundamental point of this paper was to build up an entire system in the vitro simulation model utilizing common porcine hip joints and a pendulum erosion test system with a specific end goal to analyze the tribology of the total regular hip joint. The strategy was to produce hips with various morphologies and to be effectively modifiable for use with human tissue and distinctive simulation systems, e.g. a physiological hip joint test system. The philosophy was surveyed by leading in vitro simulations on a gathering of complete, anatomically coordinated porcine hip joints and a gathering of porcine hip hemiarthroplasty joints, and with the plan of testing hip joints situated with various ace tabular and femoral introductions in future investigations. Casesnoves, and Suzenkov et al., studied Mathematical Models in Biotribology with 2D-3D Erosion Integral-Differential Model and Computational- Optimization / Simulation.40–50 Mainly they found the 2D or 3D model creation and its applications to the biotribology to improve the performance and estimation of biomaterials’ use to the human body parts replacement and its functional performance increase non-linear programming simulation model which can be improved for further recommendation. Huang, Wang, Liu, Wan, and Xue et al., carried out research on vitro assessment of the tribological reaction of Mo-doped graphite-like carbon film in various organic media.8,9,25 Taking everything into account, this work uncovered that Mo-doped graphite-like carbon (Mo-GLC) film enhanced antifriction and antiwear properties and the soundness in organic situations. The discoveries showed that the friction coefficient of Mo-GLC film under every exploratory condition was lower than that of pure GLC film. Under the dry sliding condition, in view of the nonappearance of organic oils and the arrangement of covalent bonds between tribopair, all the films have both a high wear rate and friction coefficient. In physiological saline (PS) and simulated body fluid (SBF) arrangement, the movement has a lower friction coefficient and a lower wear rate than that noticeable all around due to the nearness of the tribochemical responses items and the oil of natural media. In the fetal bovine serum (FBS) arrangement, the movement have the most minimal rubbing coefficient and wear rate, which is achieved by methods for the boundary lubrication impact of the thick protein solid-like films.
Puccio and Mattei worked on the bio-tribology of counterfeit hip joints.16,28,36,38 The aim of this paper was to describe the biotribology of hip replacements both qualitatively and quantitatively. The essential ideas of tribology gave in the initial segment especially for non-pros, are connected to fake hip joints, ultimately permitting an understanding of the genuine patterns in hip arthroplasty. The enthusiasm for bigger head sizes, the expanding utilization of CoC inserts, the squeaking of hard-on-hard couples, and even the high disappointment rates of resting heart rate (RHR) inserts are considered and clarified from a tribological perspective. Singh and Sreedhar worked on 'Bio-tribology and its Applications in Medical Sciences - A Review.51 In this study, few papers were evaluated which were identified having the discussion of tribo-system in the medicinal world. It was seen that for the prosthesis, a couple of high-quality paste-like things could be used for post-operation, and determination of the bio-materials can be made thinking about a couple of factors.52 A few tribological engineered materials and common tissues are associated with the bio-medical frameworks that work in the mind-boggling condition. So to design any prosthetic gadget for a lifetime and its execution particulars for the purpose should be considered. McGonagle L et al. observed that some anti-adhesive agents can be applied during surgery to prevent adhesion formation, whilst reportedly providing some reduction in friction during in vitro tendon-bony pulley investigations. This bio-tribological study evaluates whether the application of these agents can improve the lubrication between the tendon and surrounding tissue, thus potentially reducing the risk of re-rupturing the tendon at the repair site.18 Mainly they performed in this paper bone synovial fluid characteristics and its utilization of thin film to produce the separate surfaces. Zivic, Babić, Grujović, and Mitrović et al., performed an investigation on material tribometry for bioengineering applications.1–5 In their research work, they concluded with frictional power estimation and coefficient of erosion count was an important issues. It was a common phenomenon to human joints that were regulated by rubbing power. For different types of material used in human body joints, it was examined to the current materials and new materials for critical exercise also. Suri, Harun, and Syahrom et al., took a title on the Lubrication Impact of Metal-on-Metal in Hip Joint Replacement.36,53–58 Metal was used for dry and lubrication purposes. But in these implants, the metal ion can release from the used metal that can enter the blood vessel and create a hamper. In the future, the metal replacement or implant to the human body will be considered the chemical reaction with each other. Tipnis and Burgess made a title on the topic of 'Sterilization of implantable polymer-based medical devices: A review.59–64 Implantable polymer-based material is very sensitive for use in the human body. So, considering the issue is needed to sterilize for removing or freshen or bacteria-free and also the long-term use of polymer implant to the body. Different types of sterilize methods were discussed and suggested to the ethylene oxide method more suited for it. Niculescu, Antonia, Vasile, Semenescu, Trent, Sohaciu, and Musetescu et al., studied the subject entitled 'Assessment of Biodegradability of Careful Engineered Absorbable Suture Materials: An In Vitro Study.65–67 From this study, the suture material is used in the body for reducing the weight of polymer material and create more flexibility for the patients. Biodegradable suture materials degrade in the immersion time and pH values. Faster degradation occurs in the high alkaline medium. Bourquin, Milosevic, Hauser, Lehner, Blank, Petri-Fink, and Rothen-Rutishauser et al., found on the topic of Bio-distribution, Clearance, and Long haul Destiny of Clinically Important Nanomaterials.68–70 Nanomaterial application in bio-engineering, its long-lasting use, and the bio-distribution process was discussed elaborately. Since in different body sections clearance is needed for clinical purposes, as such bio-distribution processes are discussed in blood mixing medicinal purposes.71
The hip may be a genuine ball and attachment joint as shown in Figure 1. This course of action gives the hip the expansive sum of movement required for everyday exercises like strolling, hunching down, and stair climbing. How the distinctive layers of the hip are orchestrated and associated can assist to get how the hip works, how it can be harmed, and how challenging recuperation can be when this joint is harmed or harmed by joint pain. The most profound layer of the hip incorporates the bones and the joints. The other layer is made up of the tendons of the joint capsule and at long last, these tendons are secured by the imperative ligaments and the muscles that offer assistance to move the leg. The imperative structures of the hip can be partitioned into a few categories: these incorporate bones and joints, tendons and ligaments, muscles, nerves, blood vessels, and Bursae. Articular cartilage is the fabric that covers the closes of the bones of any joint. It is almost around 1/4 inch thick within the large weight-bearing joints like the hip. It looks like a white and glossy thing and encompasses a rubbery consistency. It is elusive which permits the joint administrations to slide against one another without causing any harm. The work of articular cartilage is to assimilate stun and give a greatly smooth surface to create movement simpler. This is very much asymmetric with the tribological behavior of mechanical engineering.
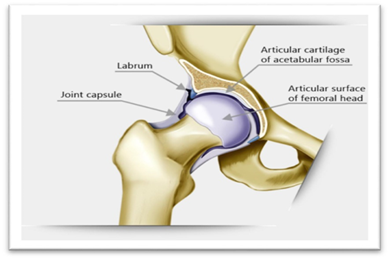
Figure 1 Hip joint and cartilage.13
Knee joint
The knee is a modified hinge joint, a type of synovial joint, which is composed of three functional compartments: the patellofemoral articulation, consisting of the patella, or "kneecap", and the patellar groove on the front of the femur through which it slides; and the medial and lateral tibiofemoral articulations. Knee cartilage as shown in Figure 2 is usually bedded in two ways, from cartilage to cartilage and cartilage to artificial bio-materials. Cartilage to Cartilage is related to mechanical and biochemical erosion. If a person is totally destroyed in cartilage, then the bone is more prone to bone and the person feels more pain. The wear and damage which are evident in mechanical joints or in the moving parts due to friction and loading/stress of engineering tribology exhibits similar frictions and wear in the bio-tribology.
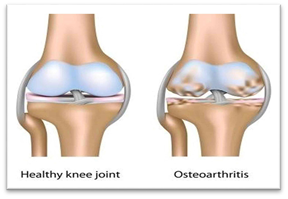
Figure 2 Knee joint and cartilage.13
Dentistry
The contact between teeth requires investigation into their tribological behavior focusing on the enamel wear process against natural teeth and/or artificial teeth, allowing us to obtain useful information on the tribological behavior of restorative materials. Considering the complex inter-oral environment and biomechanics, the wear processes of artificial dental materials are very complicated and normally include abrasion, attrition, corrosion, fretting wear, and fatigue. These processes occur in various combinations to cause surface loss of materials in the mouth. Tooth surface loss most often results from the natural tooth-to-natural tooth and/or natural tooth-to-restoration contact (Figure 3). It is often accelerated by restorations—this is especially true with opposing ceramic restorations. The reduction of the surface might lead to a variety of problems. These include loss of enamel, loss of dentine, teeth fracture, hypersensitivity, compromised aesthetics, misshapen teeth, loss of tooth vitality and problems in chewing, and possible jaw problems as a result of reduced facial vertical dimension in patients with generalized tooth surface loss (Figure 4). These types of bio-tribological behaviors are very much significant in human dentistry.
Artificial implants in human joints and dentistry
Figure 1 & Figure 2 are indicated artificial hip and knee joints implanted in humans. In hip joint acetabular metal, in Liner ceramic, Femoral Head ceramic, and Femoral Stem metal are used. Cartilage works mostly between Femur and Tibia, mainly on slippery, friction, and wear. Cartilage is connected to Femur and tibia by cross-linked joint. Due to movement of the body i.e. Tibia and Femur, there is a lot of pressure on the cartilage. The main reason for being wasted in cartilage is because of a road accident, sports accidents, carrying heavy things, and getting older. If a bone contacted to cartilage is lost due to accidental or other reasons, it may cause pain when it turns fracture with cartilage after some time, by replacing the bone with bio-materials or materials. Most of the bones next to cartilage are changed with different types of materials such as alumina, cobalt-chromium, titanium alloy, stainless steel, and ultra-high polyethylene, etc. This material is much more of the hardness and strangulation which is very much needed. These materials are very easy to find, and they are quite cheap at prices. The hip joint consists of the cross-linked of the femoral head and acetabulum cup. Figure 5 shows that metal ions are emerging and entering the joint space. These ions are interrupted with side tissues and capsules in Figure 6. Those who have to fall in front of the damage to the body, in addition to their hip substitution (also called add up to hip arthroplasty), the harmed bone and cartilage is evacuated and supplanted with prosthetic components. The harmed femoral head is evacuated and supplanted with a metal stem that's set into the empty center of the femur. The femoral stem may be either cemented or "press-fit" into the bone. A metal or ceramic ball is put on the upper portion of the stem. This ball replaces the harmed femoral head that was removed. The harmed cartilage surface of the attachment (acetabulum) is evacuated and supplanted with a metal attachment. Screws or cement are in some cases utilized to hold the attachment in place. A plastic, ceramic, or metal spacer is embedded between the unused ball and the attachment to permit a smooth floating surface. Currently, there are many types of design and metal used in artificial hip joints. Two types of common components are seen: (1) Ball component (2) Socket component. Ball component is usually highly polished metal or ceramic material. And socket component is sturdy plastics or ceramic, metal. The impacts of mental flotsam and jetsam discharged from prosthetic hips incorporate component releasing, component misalignment, contamination, bone breaks, disengagement, metal affectability, and noteworthy torment. Other issues incorporate delicate tissue devastation which may compromise corrections and amendment surgery. In mal arrangement, specific surfaces are pounding despicably which causes metal parts and particles to discharge and enter into encompassing tissues and joint spaces. These wear flotsam and jetsam may moreover contribute to aggravation in adjoining tissues and systemically all through the body. The main reason for using cobalt-chromium is a good surface finish, availability, and lower friction. Dental bio-tribology is a developing and promptly expanding research field that develops an understanding for designing dental implants and a better selection of artificial dental material. The importance of tribology in modern restorative dentistry is significantly reviewed including synthetic teeth and dental implants. In dentistry, filler materials are used like metal, alloy, and ceramic also. Crown materials mainly ceramic, metal, and composites are recommended. Polymer materials are mainly used as adhesive. These are also used in other prostheses and retainer. These figures' mechanisms mainly help the baby's tooth straighten out in a time of toothache (Figure 7).

Figure 5 Metal ions are released and entering the joint space and surrounding tissues.55
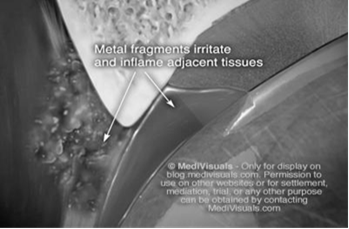
Figure 6 Metal ions are interrupting the joint capsule and surrounding tissues.55
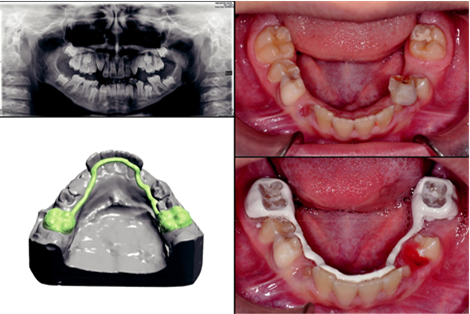
Figure 7 Polymer in orthodontics.63
Comparative study
From the comparative study, it can be declared that the use of metal on human body joints faces some difficulties compared to natural joints. Because, they need to replace after certain times due to chemical reactions, mechanical erosion, frictional losses, and also create blood vessel problems. Again the use of ceramic materials has some limitations mainly because of the weightiness and perfection of manufacturing. Polymer materials are recommended nowadays by specialists in these types of tribological applications (Table 1). Materials used in the human body joints need the analysis of different characteristics of materials and also body parts. For making it smoother, it demands to consider the biological concept of wear, friction, and erosion. This means material that can be suited for human body parts and blood reactions to be selected. From the table, knowledge about the use of material for replacement or adding additives may be gathered. Using of material, natural parts can be damaged, and also the frictional losses of metal ion can hamper the blood purity for toxicity of its ion. In the time of using different types of material to the human body, its chemical & mechanical properties should be considered with respect to the body effect.
|
Ser |
Positions |
Materials used |
Reaction to the body due to biotribological efffect |
Reasons of tribological effect |
|
1 |
Hip Joint: · Aceptabular · Liner · Femoral Head · Femoral Stem |
· Metal or Polyethylene (Cementless or cemented) · Ceramic or Polyethylene or Co-Cr alloy, Ti alloy · Ceramic or Metal · Metal( Cement less or cemented), Ti alloy |
· Using of metal and alloy man can trigger inflammation and discomfort in surrounding area. · Damage creation & deterioration in bone & tissue over time.72 · Non-toxic Ceramic Material is better but over time can show its brittleness.73 |
Weighted materials are not good for easy movement and comfortability. Metal and ceramic are weighty materials. |
|
2 |
Knee Joint: · Femoral Component · Tibial Component · Tibial Insert |
· Metal or Co-Cr alloy · Metal or Co-Cr alloy · Polyethylene |
· Metal and alloy can show the same effect as hip replacement. Cross linked polyethylene is recommended to use in tibial insert.74 |
Same as to the hip replacement. But polyethylene more light. |
|
3 |
Dentistry: · Filler · Crown
|
· Metal, Alloy ( Cr-Co) · Composites, Metal, Cements, Adhesives |
· Injectable filler material creates problem in adequate filling and proper positioning of it. Solid & semisolid can also create problem for long run uses.75 |
Weighty material affect the dentistry applications. |
Table 1 Tribological effect of recent materials used in human body joints and dentistry
Bio-tribology is mainly related to bio-engineering that is used in human body joints and dentistry for lubricating and also as the contact parts of the body. Friction and wear are the essential considering issues to improve the materials used in the body joints with respect to that of the reaction of human anatomy. Before using the material to the human body joints and dentistry their properties, responses, and chemical reaction must need to study. Different types of analysis assisted this study to gain knowledge about the bio-tribological material used in the system. The human body adjusted replacement parts or implants can be designed considering the chemical and mechanical erosion control characteristics of materials. Finally, it has been concluded by recommending the use of composite materials for different joints to the human body and dentistry.
None.
The author declare that there is no conflict of interest.

©2021 Alam. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.