MOJ
eISSN: 2475-5494


Review Article Volume 7 Issue 3
Federal State Autonomous Educational Institution of Higher Education “M. K. Ammosov North-Eastern Federal University” Medical Institute, Russia
Correspondence: Yakovlev Anton Antonovich, Federal State Autonomous Educational Institution of Higher Education “M. K. Ammosov North-Eastern Federal University” Medical Institute, 677000, Russian Federation, Republic of Sakha (Yakutia), g. Yakutsk, ul. Khalturina, d. 34/2, kv. 55, Russia, Tel +7 914 233-11-57
Received: March 17, 2018 | Published: May 3, 2018
Citation: Yakovlev AA, Vinokurov MM. Regional thrombolysis with massive thromboembolism of the pulmonary artery of women in the first first trimester of pregnancy. MOJ Womens Health. 2018;7(3):76-78. DOI: 10.15406/mojwh.2018.07.00173
The article describes a clinical example of successful regional thrombolysis with massive pulmonary arterial thromboembolism of the pulmonary artery of women in the first first trimester of pregnancy. Conducted local thrombolytic therapy saved not only the life of a woman, but also the life of a conceived child.
Keywords: Thromboembolism of the pulmonary artery, regional thombolytic therapy, pulmonary artery, posterior tibial vein, international normalized ratio, prothrombin index, inferior vena cava, left ventricle, CT scan, peptic ulcer
The frequency of thromboembolism of the pulmonary artery: during pregnancy - 0.05-0.1%; in the postoperative period - 3%.Mortality in this pathology ranges from 8 to 30% and depends on the quality of diagnosis, treatment, pregnancy and delivery.1–4 The main causes of maternal death of thromboembolism of the pulmonary artery are a reflex drop in cardiac output, ventricular fibrillation and acute respiratory failure.1,2,4,5 Accepted obstetric tactics in pregnant women with thromboembolism of the pulmonary artery at the present time depends on the severity of the patient's consciousness, gestation period, fetal condition, joining of other obstetric and extragenital complications. With the development of thromboembolism of the pulmonary artery in the first trimester of pregnancy after arresting cardiopulmonary shock, the elimination of thrombosis and stabilization of the woman's condition, pregnancy should be interrupted due to the severity of the disease, fetal radiation in the early stages of pregnancy, the need for prolonged anticoagulant and antithrombotic therapy. With the development of thromboembolism of the pulmonary artery in the second and third trimesters, the issue of maintaining pregnancy should be addressed individually, depending on the condition of the woman and the viability of the fetus. With successful treatment of pulmonary embolism, satisfactory patient condition and absence of pathology in the fetus, pregnancy can be carried (but not preserved!).1,4
Conditions for bearing pregnancy after pulmonary embolism: integrated management of pregnancy together with related specialists (obstetrician-gynecologists, hematologists, anesthesiologists-resuscitators, vascular surgeons and cardiosurgeons); continuous anticoagulant therapy throughout pregnancy; quality laboratory control of anticoagulant therapy; regular control of echocardiography of pulmonary-cardiac hemodynamics and compression two-dimensional echocardiography of the veins of lower extremities; continuous monitoring of the fetus.Pregnancy should be interrupted in case of a serious condition of a woman (an increase in pulmonary hypertension or the development of severe pulmonary hypertension), a progressive deterioration in the functional state of the fetus, and the addition of other obstetric and extragenital complications. When treating thromboembolism of the pulmonary artery in pregnant women, the primary task is to eliminate the obstruction of the pulmonary artery and restore its patency. To date, thrombectomy from the pulmonary artery and thrombolytic therapy have been used for this purpose.6 Surgical treatment can save the life of a patient with massive pulmonary artery obstruction, but only a very small number of specialized vascular clinics are actually available. At present, the most accessible and most frequently used method of recanalization of the pulmonary artery in pulmonary embolism, despite obvious shortcomings, is the method of selective, regional thrombolysis. Due to simplicity, systemic thrombolysis is often used in almost all vascular centers.1,2,4,5 With the appearance of an X-ray surgical operation in our clinic, endovascular mini-invasive methods of surgical treatment for patients became possible for everyday practical activities.
We give an example of the successful treatment of a patient during the first trimester of pregnancy with pulmonary artery thromboembolism that took place up to a day-old prescription in the first surgical department of the republican hospital No. 2 of the center for emergency medical care, where regional thrombolytic therapy using endovascular mini- invasive methods of surgical intervention was used. A patient of 38 years old complained of severe suffocation, lack of air, chest pain. From anamnesis: According to the patient, she came from the village of Khandygi in the morning (she was 12 hours by car), and when she climbed the stairs at 06:00 am, abdominal pain, a feeling of lack of air, the patient fell and hit her head. Before that, for two weeks, the pains and swelling of both lower limbs were disturbed. She did not apply for medical help. The condition is extremely difficult. Consciousness is clear. Skin covers and visible mucous membranes are clean, pale with cyanosis of the face. Breathing is carried out in all the pulmonary fields, there are no wheezing, weakened in the lower parts. Heart tones are rhythmical. Blood pressure 100/50 mm Hg. Pulse is 160 per minute. The abdomen is soft, painless. Intestinal peristalsis is heard. The gases are moving away. Diuresis is normal.
08.07.2016 Electrocardiography. Severe sinus tachycardia with a heart rate of 162 beats per minute. Electronic Heart Axis SI QIII. Peaks QS in V1-V4 (V5) with (-) peak T in combination with the clinic, anamnesis. Do not exclude thromboembolism of the pulmonary artery. Electrocardiography in dynamics. General blood analysis. WBC=13 10^9/L; HGB=121 g/L; RBC=4.28 10^12/L; HCT=39.6%; PLT=135 10^9/L; basophils=1%, segment neutrophils=77%; lymphocytes=20%; monocytes=2%; erythrocyte sedimentation rate=34 millimeters per hour. D-dimer=>5000; 08.07.2016 Antithrombin=103%. 08.07.2016 Blood chemistry. Total protein=61.4 g/L; Albumins=31.8%; Total bilirubin=8.4; Blood glucose=5.8; Urea=2.2; Creatinine of blood=87; Amylase of blood=57; Alanine aminotransferase=16; Aspartate aminotransferase=18. 08.07.2016. Ultrasound examination of the heart and blood vessels: Complications in the study: forced position in orthopnea, non-optimal visualization. The maximum anterior-posterior size of the left atrium is 3.3 centimeters. The maximum opening of the valves of the aortic valve is 1.6 centimeters. The diameter of the root of the aorta is -1.8 centimeters. The diameter of the aorta in the bulb area is 2.9 centimeters. The thickness of the interventricular septum in diastole is 1.1 centimeters. The thickness of the back wall of the left ventricle in the diastole is 1.1 centimeters. The maximum antero-posterior size of the outflow tract of the right ventricle is 3.8 centimeters. The diameter of the pulmonary artery trunk is 2.3 centimeters. Blood flow in the trunk of the pulmonary artery: the maximum speed is 50 centimeters per second. The maximum velocity of blood flow on the mitral valve is 83 centimeters per second. Parameters of the aortic blood flow: the maximum speed is 101 centimeters per second. Blood flow in the tricuspid valve is 41 centimeters per second. The diastolic volume of the left ventricle is 84 milliliters. The systolic volume of the left ventricle is 33 milliliters. Fraction of ejection of the left ventricle - 60%. The maximum volume of the left atrium is 55 milliliters, not enlarged. The maximum volume of the right atrium is 42 milliliters, not enlarged. The study was conducted against a background of severe tachycardia. Visualization of the structures of the saddle is difficult, the patient in forced position orthopnea, all dimensions are given approximate, some of the structures could not be visualized. The systolic function of the left ventricle is normal.ejection fraction 60%. Moderate expansion of the right ventricle. Rough, distinct zones of disturbed local contractility of the left ventricular myocardium were not revealed. The lower vena cava could not be visualized. Indirect signs of pulmonary hypertension. Additional echostructures in the heart cavity are not reliably detected.
08.07.2016 Ultrasound examination of veins of lower extremities. Complication in the study - the forced position in the orthopnea. On left: The large subcutaneous vein, the proximal segment of the common femoral vein, the deep femoral vein are passable, the lumens compression is a complete, pronounced effect of spontaneous contrasting.In the tibial veins, blood flow is not recorded. Subcutaneous vein - it was not possible to visualize. In the lumen of the superficial femoral vein, along the entire length, thrombotic masses of various echogenicity are visualized, completely obturating the lumen.The end of the thrombus is visualized in the distal segment of the common femoral vein (at a distance of about 1.0 to 1.5 centimeters from the bifurcation). No signs of flotation have been identified. Minor edema of surrounding tissues, mainly on the shin level. Right: large saphenous vein, common femoral vein, deep femoral vein, tibial veins - passable, compression of lumens full, pronounced effect of spontaneous contrasting. The total femoral vein is expanded to 1.9 centimeters, the lumen compression is complete. In the lumen of the superficial femoral vein, the parietal thrombotic masses are visualized without signs of flotation, the blood flow is recorded weakly phase. Subcutaneous vein - it was not possible to visualize. Minor edema of surrounding tissues, mainly at the level of the shin. Echographic features of occlusive thrombosis of the superficial vein vein, left without flotation symptoms, near-wall thrombosis of the superficial femoral vein of the spas without flotation symptoms. The pronounced effect of spontaneous contrasting. Edema of both shins.
The patient was urgently transported to the X-ray room, accompanied by an anesthesiologist. The patient is warned about possible complications of medical procedures and termination of pregnancy. The woman categorically refused to stop pregnancy, motivating about the desired pregnancy.Before us there was a question on preservation of two lives: a life of mother and the child. In the rengen-operativeinstallation of the pigtail catheter for regional thrombolysis therapy through the jugular vein on the right, cavitation of the inferior vena cava, a detachable cava filter is installed in the lower hollow vein below the renal vein bifurcation, angiopulmonogrophy (Figure 1). After the catheter was inserted into the pulmonary bifurcation, the patient was transferred to the intensive care unit for regional thrombolysis.The drug of choice for the thrombolytic therapy was chosen Aktelize 100 mg. The first dose of the 10 mg Aktelize solution was introduced into the bolus bolus catheter for 2 minutes. The remaining solution of 90 mg of Actilele is connected to a syringe pump. The drug was administered for 2 hours under the control of a coagulogram. After carrying out thrombolysis therapy, the patient continues therapy with low molecular weight heparins.
| Parameter | 16.03.16 |
16.03.16 |
16.03.16 |
16.03.16 |
INR |
1.62 |
3.16 |
2.78 |
1.55 |
PTI |
60.1 |
22.7 |
25.7 |
48.7 |
APTT |
57 |
75.4 |
64.4 |
33.4 |
As can be seen from the table of significant changes in the pattern of coagulogram in a four-hour dynamic observation did not occur, which corresponds to the data of literature sources in the periodical publications on angiology.1,4,5
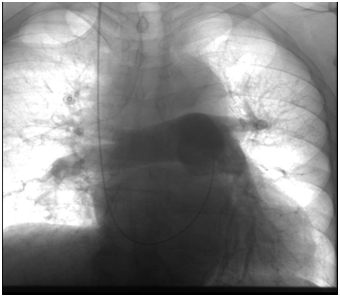
12 hours after thrombolytic therapy, control angiopulmonography was performed (Figure 2):
The patient continued therapy with low molecular weight heparins Clexane 0.8 mgg x 2 rach subcutaneously per day. Conclusion of control computed tomography of chest cavity organs with contrast before discharge in comparison with 16.03.16. positive dynamics in the form of the absence of contrast defects in the left pulmonary artery. The installed cava filter was removed on the 14th day after the monitoring of the cava. Ultrasound examination of the veins of the lower extremities from 07/28/2016. Complications in the study are absent. Conclusion: Echographic signs of occlusive thrombosis of the superficial femoral vein on the left without flotation symptoms in the stage of moderate recanalization, near-wall thrombosis of the superficial femoral vein on the right without flotation symptoms. The pronounced effect of spontaneous contrasting. Edema of both shins. When compared with the study of 22.07.2016 - positive dynamics in the form of recanalization. Later the patient was transferred to the Perinatal Center of the Republican Hospital No. 1 for further dynamic observation, treatment and maintenance of pregnancy. Continued to study the course of anticoagulant therapy, during pregnancy. Childbirth operative on time. He was a healthy, full-blooded child, without deviations from his health. Thus, the regional thrombolytic therapy saved the lives of the mother and child in the first trimester of pregnancy. Successfully ended with operative labor with the birth of a full-term healthy child.
Parameter |
16.03.16 |
16.03.16 |
16.03.16 |
16.03.16 |
INR |
0.99 |
1.1 |
1.04 |
1.04 |
PTI |
102.1 |
81.7 |
90.7 |
90.7 |
APTT |
22 |
28.4 |
22.4 |
22.4 |
As can be seen from the table of significant changes in the pattern of coagulogram in the dynamic observation didn’t occur, which corresponds to the data of the literature sources in the periodic publications on angiologists.
None.
Author declare that there is no conflict of interest.

©2018 Yakovlev, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.