MOJ
eISSN: 2475-5494


Research Article Volume 10 Issue 3
1Department of Internal Medicine and Gynecology/Obstetrics, Barentu Regional Referral Hospital, Eritrea
2Department of Internal Medicine and Gynecology/Obstetrics, Afabet Community Hospital, Eritrea
3Department of Population Health, University of Auckland, New Zealand
4Department of Community Medicine, Asmara College of Medicine and Health Sciences, Eritrea
Correspondence: Yohannes Mekonen, Department of Internal Medicine and Gynecology/Obstetrics, Barentu Regional Referral Hospital, Barentu, Eritrea, Tel 291-1-7155478
Received: May 27, 2021 | Published: June 16, 2021
Citation: Mekonen Y, Berhe H, Ghebreab L, et al. Factors associated with knowledge, attitude and practice of cervical cancer and its screening (Pap smear) among female students of Orotta College of medicine and health sciences in Eritrea: a cross-sectional study. MOJ Women’s Health. 2021;10(3):51-61. DOI: 10.15406/mojwh.2021.10.00288
Background: Cervical cancer is one of the leading causes of cancer-related deaths worldwide that affects developing countries and young women in particular. Out of many types of female cancers, cancer of the cervix could be prevented if appropriate medical interventions are taken on time. Pap smear is a means for early detection of premalignant stages and treatment before the disease advances to a late stage. However, its practice remains unsatisfactory in many countries including Eritrea.
Objective: The aim of the study was to illustrate knowledge, attitude and level of cervical cancer and Pap smear practice and associated factors among female students of Orotta College of Medicine and Health sciences (OCMHS).
Methods: A cross-sectional study was conducted among female undergraduate students in OCMHS enrolled during the academic year 2018-2019. A total of 252 students participated in the study. Piloted, structured questionnaire was used to collect data. Descriptive and inferential statistics were used to assess the distribution and to identify associations between independent and outcome variables respectively.
Results: Majority of the students, 171 (68.4%), were 18-21 years old and 159 (63.6%) were second and third year students. One hundred thirty six (54.4%) students had inadequate knowledge and one hundred twenty three (49.2%) had negative attitude towards cervical cancer screening. Only two (0.8%) participants had ever been screened with Pap smear test. Logistic regression analysis showed that age, level of education and year of study were significantly associated with knowledge of cervical cancer and its screening methods. Year of study and knowledge levels were significantly associated with attitude towards cervical cancer screening (Pap smear).
Conclusions: The study showed that there is a lack of knowledge of cervical cancer, unfavorable attitude towards screening methods and poor utilization of Pap smear. The study emphasized the importance of creating awareness and increasing knowledge of cervical cancer and Pap smear through numerous health education campaigns and mass media. Hence, it will be vital to integrate cervical cancer preventive measures with other reproductive health care services at all, if not at the highest, levels of health care delivery system.
Keywords: Knowledge, attitude, practice, cervical cancer, pap smear
The five main types of gynecologic cancer are cervical, ovarian, uterine, vaginal, and vulvar.1 Cervical cancer alone is the fourth most common cause of cancer-related deaths worldwide with 311,000 deaths in 2018.2 It was the second most common cause of cancer in women worldwide by the turn of the millennium.3 Comparing the year 2008 to 2000, the global number of cases have surge.1,3 In 2008, out of the total worldwide morbidity from cervical cancer, 85% of cases occurred in less developed countries and particularly in young women.1,2 Cervical cancer is largely preventable4 but inadequate implementation and accessibility to prevention, screening and treatment contribute to 90% of deaths, predominantly in low-income countries.5
The mortality rates of cervical cancer in developed countries have decreased over the past 30 years owing to extensive screening with cervical cytology.6 A Pap smear, also known as a Papanicoloau smear, is a microscopic study of cells taken from the cervix and is used to detect cancerous or pre-cancerous lesions of the uterine cervix (lesions primarily caused by chronic infection with oncogenic types of human papillomavirus).7 Early detection through Pap smear test during a regular screening process markedly reduces the incidence of invasive cervical malignancy.8 A woman should start Pap smear screening at the age of 21- regardless of age at sexual initiation or other behavior-related risk factors.6
Mortality and incidence rates of cervical cancer among women in Eastern, Western and Central Africa is significantly higher than in developed countries.2,7,9 Such marked differences can be explained by low preventive health-seeking behaviour and limited access to effective screening services due to cost, poor knowledge, lack of information and educational programs.10,11 Survival rate turns out to be better if cervical cancer is diagnosed and treated at earlier phases. Generally, developing countries have a lower Pap smear coverage (19%) as compared to developed countries (63%).12 Numerous factors have been implicated affecting the practice of Pap smear such as socio-demography (age, religion, level of education etc.), socio-economy (occupation, income etc.), reproduction (parity, sexual activity etc.), knowledge, information, attitude, beliefs and barriers such as embarrassment, fear and lack of encouragement from family.13,14
Non-communicable illnesses in general and gynecological cancers in particular have recently become a double burden for Eritrea.15 Between 2011 and 2017, 883 cases of cervical, ovarian and uterine tumours were reported in Eritrea and benign and malignant tumours comprised of 614 and 269, respectively.15 According to another study in Eritrea, secondary cervical cancer prevention (detection and treatment of precancerous lesions) is suggested an efficient strategy for low-income countries as the low cost of Pap test and availability of human resources could lower the incidence of cervical cancer and related deaths.10 Results of the study also showed a high prevalence of cervical cancer in population of Asmara, the capital city of Eritrea, though no dependable evidence has been yet attained on the incidence of the disease in Eritrea.10,16 The initiation and successful application of secondary prevention program hence needs a paved platform of well informed and educated female population. This study aimed to provide information on cervical cancer awareness and factors associated with knowledge, attitude and practice of screening particularly among female undergraduate students in Orotta College of Medicine and Health Sciences (OCMHS).
Study design and setting
This study was a college-based cross-sectional survey conducted among female students who were enrolled as full-time in the academic year 2018-2019 in OCMHS, Asmara, Eritrea. It's the only health college in Eritrea and one of the leading research colleges. It has seventeen departments and offers undergraduate and postgraduate courses. The survey was conducted from 24th September, 2019 to 22nd October, 2019.
Source and study population
The source population was all undergraduate female students who enrolled in OCMHS. There were a total of 693 female students in OCMHS enrolled as full-time in the academic year 2018-2019. The study population comprised of female undergraduates randomly selected from various departments of the college. Freshman students, students included during the pre-test and those on long leave and who were seriously ill or not present at the time of data collection were excluded from the study. Out of all, 189 were freshman students and hence 504 were eligible participants.
Sample size determination and sampling technique
The two-proportion formula was used to calculate the estimated sample size17 with 80% power, at 0.05 level of significance and standard Z-value of 1.96. The two-proportion sample size was calculated based on a cross-sectional study conducted to identify factors associated with the knowledge and attitude towards cervical cancer screening among female Hawassa University College of Medicine and Health Sciences student.18 After assuming 10% of non-response rate, 252 were selected from the 17 departments using a simple random sampling by random number generator from each department, proportionate to the number of students in each faculty.
Data collection method
A pretested, structured questionnaire prepared in English format was used to collect data. The questions were adopted from different sources during literature review with modifications made in line with this study.19–22 The questionnaire had five domains: socio-demographic information, sexual and reproductive history, knowledge of cervical cancer and its screening methods, attitude and practice of Pap smear. The knowledge assessment section had 27 questions with three response options, “yes”, “no”, and “don’t know” and multiple choices for the symptoms and risk factors. The cut-off point for scoring method was based on the mean since the total score was normally distributed.20 Based on this, those who scored less than the mean were considered to have inadequate knowledge and those who scored greater than or equal to the mean were considered to have adequate knowledge. The questions regarding attitude had six items and were measured with different responses. The total score was divided into two categories based on the median.19 Those who scored lower than the median were considered as students having a negative attitude, while those who scored above and equal to the median were considered as having a positive attitude. Missing data on three items on attitude were less than 4% and were considered as “don’t know”, or “negative response”. There were three questions regarding the practice of Pap smear; however almost all of the students responded ‘no’ to the question stating that “Have you ever had Pap smear test?”; hence they did not respond to the rest of the questions. The outcome measures were knowledge and attitude towards cervical cancer and Pap smear test.
Data collectors were three nurses, Bachelor in Science graduates, who had experience in data collection in previous similar studies. A two-days training was given to the data collectors before the pretest on the objectives of the survey, contents of the questionnaire, issues related to the confidentiality and the right of the respondents. Department heads organized data collection days and gathered the selected students to free rooms on the days of data collection. The data were collected after informed consent obtained from the respondents. The completed questionnaires were checked for consistency and completeness by the principal investigator. The questionnaire was piloted on 14 students who did not take part in the actual study to ensure face and content validity. This was determined using comments of two gynecologists/obstetricians and two midwifery faculty members. Based on the experience gained through the pilot, amendments were made to the questionnaire.
Data analysis procedure
Data were entered first into CSpro version 7.2 and then analyzed using the SPSS version.23 Collected data was cleaned and checked for consistency and completeness. Mean, median, frequency tables and graphs (histograms) were used to describe the data. Chi-square test was used to determine the relationship between independent and outcome variables. Bivariate and multivariate logistic regression models were used to examine association between independent and outcome variables. Odds ratio with 95% confidence interval and p-value <0.05 were used to determine significant associations.
Ethical considerations
This study was reviewed and approved by the institutional review board of the OCMHS. Ethical clearance was then granted by the institutional review board of the college. Approvals were also obtained from each faculty which took part in the study. In addition, an informed written consent was obtained from each study participant.
There were 252 respondents in the study and 2 participants had inconsistent answers for almost all of the questions asked and hence were excluded from the study. The analysis was performed on the remaining participants, making an overall response rate of 99.2%.
Sociodemographic characteristics
Most of the respondents (68.4%) were younger than 22 years old with a median age of 21 (25th quartiles = 20 and 75th quartiles=22). There were 43.6% diploma level students and 56.4% degree level students (Table 1). Thirteen responders reported that they were sexually active in their lifetime and all of them had one sexual partner. As depicted in Figure 1, most of the respondents were from diploma Nursing department (34%) followed by Medicine (12.8%), degree Pharmacy (10. 4%), Clinical Laboratory Science (7.6%), Public Health (7.2%) and degree Nursing (6. 8%).
|
Variable |
Frequency |
Percentage |
|
Age (in years) (Median (IQR*) = 21(2)) |
||
|
18- 21 |
171 |
68.4 |
|
22- 45 |
79 |
31.6 |
|
Education level |
||
|
Diploma |
109 |
43.6 |
|
Degree |
141 |
56.4 |
|
Religion |
||
|
Orthodox |
186 |
74.4 |
|
Catholic |
31 |
12.4 |
|
Moslem |
17 |
6.8 |
|
Protestant |
7 |
2.8 |
|
Others |
9 |
3.6 |
|
Current year of study |
||
|
2nd |
63 |
25.2 |
|
3rd |
96 |
38.4 |
|
4th |
55 |
22 |
|
5th |
28 |
11.2 |
|
6th |
8 |
3.2 |
|
Sexually active |
||
|
Yes |
13 |
5.2 |
|
No |
237 |
94.8 |
Table 1 Sociodemographic characteristics of participants (N= 250)
*IQR (Inter-quartile range)
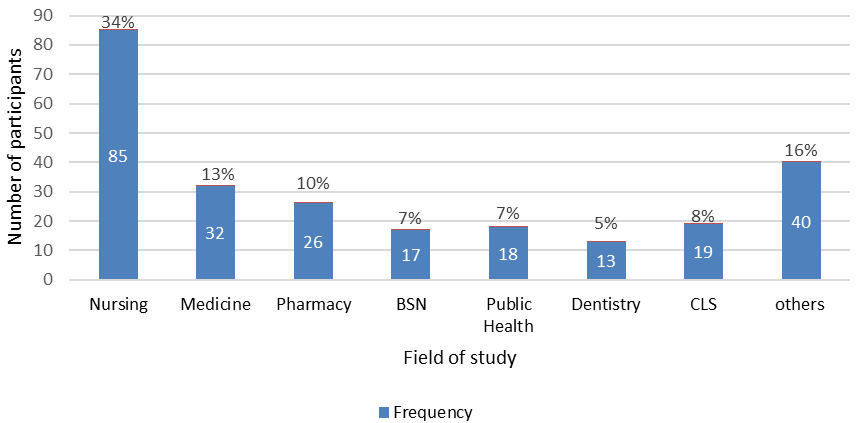
Figure 1 Field of study of participants (N= 250).
Note “Others”: Less than 3% in each department (Ophthalmic Nursing, Mental Health, Optometry, Anesthesia, Midwifery, Medical Laboratory Technician, Radiology, Physiotherapy, Dental Technician and Pharmacy Technician).
Knowledge about cervical cancer and pap smear
The main source of information was from course lectures, followed by books, media (TV, radio, internet etc.), hospital and friends (Figure 2).

Figure 2 Sources of information of cervical cancer of participants (N= 250).
Note “Others”: Less than 3% in each department (Ophthalmic Nursing, Mental Health, Optometry, Anesthesia, Midwifery, Medical Laboratory Technician, Radiology, Physiotherapy, Dental Technician and Pharmacy Technician).
Majority of the responders (92.8%) had heard about cervical cancer. More than half (58%) stated that cervical cancer is preventable, 40.8% believed that cervical cancer is commonly caused by a virus and 27.2% think that cervical cancer is treatable when diagnosed early. Large percentage (92.8%) of the students were aware of screening tests for cervical cancer, of whom the majority (86.8%) think Pap smear is the method of choice for screening. Only 8% of participants identified all the signs of cervical cancer and only 3.2% were aware of all the risk factors of cervical cancer. Moreover, more than half (67.6%) were not aware of the existence of Pap smear screening and further 10% believed there is no screening program in Eritrea (Table 2). The total knowledge adequacy towards cervical cancer score was 27 (with minimum 5 and maximum 25), and then categorized based on the average score (mean = 15). A total of 114 (45.6%) students had adequate knowledge and 136 (54.4%) had inadequate knowledge.
|
Variables |
Frequency (n) |
Percentage (%) |
|
Have you ever heard about cervical cancer? |
||
|
Yes |
232 |
92.8 |
|
No |
18 |
7.2 |
|
Cervical cancer is preventable |
||
|
Yes |
145 |
58 |
|
No |
105 |
42 |
|
Cervical cancer is treatable when diagnosed early |
||
|
Yes |
68 |
27.2 |
|
No |
182 |
72.8 |
|
Cervical cancer is commonly caused by a virus |
||
|
Yes |
102 |
40.8 |
|
No |
148 |
59.2 |
|
Is there a screening method for cervical cancer? |
||
|
Yes |
232 |
92.8 |
|
No |
18 |
7.2 |
|
Most common screening types for cervical cancer * |
||
|
Blood sample |
26 |
10.4 |
|
Urine Sample |
15 |
6 |
|
Imaging |
36 |
14.4 |
|
Pap smear |
217 |
86.8 |
|
Risk factors of cervical cancer * |
||
|
Infection with human Papillomavirus |
147 |
58.8 |
|
Smoking |
113 |
45.2 |
|
Weakened immune system |
111 |
44.4 |
|
Sexually transmitted infection |
174 |
69.6 |
|
Many sexual partners |
160 |
64 |
|
Sex at a young age (before age 19) |
93 |
37.2 |
|
Giving birth to many children (>5) |
36 |
14.4 |
|
Not going for regular smear (Pap) tests |
96 |
38.4 |
|
Signs of cervical cancer * |
||
|
Vaginal bleeding between periods |
131 |
52.4 |
|
Persistent lower back pain |
83 |
33.2 |
|
Discomfort or pain during sex |
147 |
58.8 |
|
Vaginal bleeding during or after sex |
145 |
58 |
|
Vaginal bleeding after menopause |
117 |
46.8 |
|
Persistent pelvic pain |
128 |
51.2 |
|
Persistent vaginal discharge |
141 |
56.4 |
|
Unexplained weight loss |
85 |
34 |
|
Are you aware that there is a cervical cancer screening program in Eritrea? |
||
|
Yes |
56 |
22.4 |
|
No |
25 |
10 |
|
Don’t know |
169 |
67.6 |
|
Knowledge (mean = 14.8) |
Total =27 |
|
|
Inadequate (<14.8) |
136 |
54.4 |
|
Adequate (>=14.8) |
114 |
45.6 |
Table 2 Knowledge of participants on cervical cancer and Pap smear (N= 250)
*There were multiple answers for the question
Attitude about cervical cancer and pap smear
Participants’ confidence on recognizing symptoms of cervical cancer was assessed and showed that 7.2 % responded as ‘very confident’, 52% as ‘fairly confident’ and 40% as ‘not at all confident’. Pap smear was labeled ‘helpful’ by the majority of participants (92.9%) and less than half (42%) considered themselves as candidates for screening (Table 3). In an open-ended question regarding the recommended age to start Pap smear, participants gave broad responses from ages 15-46. Ages 15, 20 and 21 were the most reported ages- by 8.4%, 10.4% and 16.4% of respondents, respectively. The total attitude score was divided into two categories based on the median and 50.8% of the participants had a positive attitude while the rest had negative attitude.
|
Variables |
Frequency (n) |
Percentage (%) |
|
Do you consider yourself confident in recognizing symptoms of cervical cancer? |
||
|
Not at all confident |
100 |
40 |
|
Fairly confident |
132 |
52 |
|
Very confident |
18 |
7.2 |
|
Pap test is not important for women at any age |
||
|
Agree |
43 |
17.2 |
|
Disagree |
195 |
78 |
|
Not sure |
12 |
4.8 |
|
Pap smear screening is: |
Missing= 10 |
|
|
Harmful |
3 |
1.2 |
|
Not Helpful |
14 |
5.8 |
|
Helpful |
223 |
92.9 |
|
Do you consider yourself a candidate for Pap smear after |
||
|
the age of 21? |
||
|
Agree |
105 |
42 |
|
Disagree |
145 |
58 |
|
Do you think all women aged 25-64 should undergo Pap |
Missing = 8 |
|
|
smear test? |
||
|
Agree |
161 |
64.4 |
|
Disagree |
81 |
32.4 |
|
Do you encourage your friend, daughter or |
Missing = 8 |
|
|
mother to get screened? |
||
|
Agree |
210 |
84 |
|
Disagree |
32 |
13.2 |
|
Attitude (median= 5) |
||
|
Negative (<5) |
123 |
49.2 |
|
Positive (> = 5) |
127 |
50.8 |
Table 3 Attitude of participants on cervical cancer and Pap smear (N= 250)
Practice of pap smear
Only two (0.8%) participants had ever been screened with Pap smear test. As to the question “why not screened so far”, the most prominent reasons were “Never had sex before” (55.2%) and “Confident over my health” (40.4%) (Table 4).
|
Variables |
Frequency (n) |
Percentage (%) |
|
Have you ever had Pap smear test? |
||
|
Yes |
2 |
0.8 |
|
No |
248 |
99.2 |
|
Reasons for not practicing Pap smear* |
||
|
Embarrassment |
18 |
7.2 |
|
Fear of bad result |
15 |
6 |
|
Never had sex before |
138 |
55.2 |
|
Too young to get screened |
47 |
18.8 |
|
Confidence over my health |
101 |
40.4 |
|
Religious reasons |
11 |
4.4 |
|
Pap smear is useless |
15 |
6 |
Table 4 Practice of Pap smear among participants (N= 250)
*There were multiple answers for the question
Factors associated with knowledge of cervical cancer and pap smear
The association between socio-demography, attitude towards cervical cancer and respondents’ knowledge of cervical cancer and its screening methods were analyzed using bi-variable logistic regression. Younger age groups, diploma students and second and third year students had inadequate knowledge levels (Table 5). More than half within the age group 18-21 (60.8%) were less knowledgeable than students older than 21 years of age (Table 6). They had 2 times (Crude Odds Ratio (COR) =2.3; 95% CI 1.3-3.9) higher odds of having inadequate knowledge than students over 21 years (Table 7). About 60.3% degree program students had adequate knowledge while only 26.6% diploma students had adequate knowledge. Diploma students were at odds of 4 times (COR=4.2; 95% CI 2.4-7.2) higher to have less knowledge than degree students. Majority of year-2 and year-3 students had inadequate knowledge (64.2%) and they were 3 times (COR=3; 95% CI 1.8-5.1) at higher odds to have inadequate knowledge than year-4 and above students. Adequate knowledge scores were significantly associated with positive attitude towards cervical cancer and Pap smear (63.8%) while most participants who had negative attitude (73.2%) had inadequate knowledge.
|
Variable |
Knowledge |
Chi-squared test |
|||
|
Inadequate n(%) |
Adequate n(%) |
χ2 |
Df |
P-value |
|
|
Age (year) |
|||||
|
18- 21 |
104 (60.8) |
67 (39.2) |
8.99 |
1 |
0.03 |
|
22- 45 |
32 (40.5) |
47 (59.5) |
|||
|
Education level |
|||||
|
Degree |
56(39.7) |
85(60.3) |
28.109 |
1 |
<0.001 |
|
Diploma |
80 (73.4) |
29 (26.6) |
|||
|
Year of study |
|||||
|
2nd and 3rd |
102 (64.2) |
57 (35.8) |
16.743 |
1 |
<0.001 |
|
≥ 4th |
34 (37.4) |
57 (62.6) |
|||
|
Religion |
|||||
|
Christian |
121 (54) |
103 (46) |
0.127 |
1 |
0.722 |
|
Others |
15 (57.7) |
11 (42.3) |
|||
|
Sexual activity |
|||||
|
Yes |
7 (38.5) |
6 (61.5) |
0.002 |
1 |
0.968 |
|
No |
129 (54.4) |
108 (45.6) |
|||
|
Attitude |
|||||
|
Negative |
90(73.2) |
33(26.8) |
34.39 |
1 |
<0.001 |
|
Positive |
46(36.2) |
81(63.8) |
|
|
|
Table 5 Factors associated with knowledge adequacy of cervical cancer and Pap smear (N= 250)
|
Variable |
Attitude |
Chi-squared test |
|||
|
Negative n(%) |
Positive n(%) |
χ2 |
Df |
P-value |
|
|
Age (year) |
|||||
|
18- 21 |
94(55.0) |
77 (45.0) |
7.21 |
1 |
0.007 |
|
22- 45 |
29 (36.7) |
50(63.3) |
|||
|
Education Level |
|||||
|
Degree |
55 (39.0) |
86 (61.0) |
13.443 |
1 |
<0.001 |
|
Diploma |
68 (62.4) |
41 (37.6) |
|||
|
Religion |
|||||
|
Christian |
110(49.1) |
114 (50.9) |
0.007 |
1 |
0.931 |
|
Others |
13 (50.0) |
13 (50.0) |
|||
|
Year of study |
|||||
|
2nd and 3rd |
93(58.5) |
66(41.5) |
15.085 |
1 |
<0.001 |
|
≥ 4th |
30(33.0) |
61(67.0) |
|||
|
Sexual activity |
Fisher’s |
||||
|
Yes |
5 (38.5) |
8 (61.5) |
0.633 |
1 |
0.426 |
|
No |
118(49.8) |
119 (50.2) |
|
|
|
Table 6 Factors associated with attitude of participants on cervical cancer and Pap smear (N= 250)
Note: chi square (χ2); degree of freedom (Df)
|
|
Inadequate knowledge |
Negative Attitude |
||
|
OR (95% CI) |
AOR (95% CI) |
OR (95% CI) |
AOR (95% CI) |
|
|
Age (year) |
||||
|
18- 21 |
2.3(1.3-3.9)** |
1.3(0.6-2.8) |
2.1(1.2-3.6) |
1 (0.4-2.2) |
|
22- 45 (REF) |
||||
|
Education Program |
||||
|
Diploma |
4.2(2.4-7.2***) |
3.6(1.8-7.3)*** |
2.6(1.6-4.3) |
1.2(0.5-2.3) |
|
Degree (REF) |
||||
|
Religion |
||||
|
Christian/(REF) |
||||
|
Others |
0.9(0.4-1.9) |
- |
1(0.4-2.2) |
- |
|
Year of Study |
||||
|
2nd and 3rd |
3(1.8-5.1)*** |
1.1(0.4-2.7) |
2.87(1.67-4.9)*** |
2.7(1.2-3.8)** |
|
≥ 4th (REF) |
||||
|
Knowledge |
||||
|
Inadequate |
- |
- |
4.8(2.8-8.2)*** |
4.2(2.4-7.2)*** |
|
Adequate (REF) |
||||
|
Model fit of goodness: |
||||
|
Hosmer and Lemenshow |
χ2=3.03, df=4, p=0.8 |
χ2=2.96, df=4, p=0.23 |
||
|
Nagelkerke |
R2 =26.3% |
R2 =21% |
||
|
correctly predicted |
68.80% |
|
68.40% |
|
Table 7 Predictors of inadequate knowledge and negative attitude of the study population
Note: Significant at p value of *< 0.05, **<0.01, ***<0.00; COR: crude odds ratio; aOR: adjusted odds
ratio; REF: reference group
Factors associated with attitude on cervical cancer and pap smear
Bi-variable logistic regression analysis showed that there were significant associations between age, level of study and year of study and attitude towards cervical cancer screening. Majority of participants who were 22 years of age or older had favorable attitude (63.3%) than the youngest groups. Degree program students had superior positive attitude (61%) than diploma students (37.6%). Most of the students who were above year-3 had significant (at p-value <0.001) better attitude (67%) than year-2 and year-3 students (41.5%) (Table 6). Second and third year participants were almost 3 times (COR=2.87; 95% CI 1.67-4.9) at higher odds of possessing negative attitudes than year four and above students (Table 7).
Predictors of inadequate knowledge and negative attitude
Multivariable regression analysis was employed to identify the predictors of inadequate knowledge and negative attitude towards cervical cancer and Pap smear test among the students (Table 7). Students in diploma programs were more than 3 and half times (Adjusted Odds Ratio (AOR) =3.6; 95% CI 1.8-7.3) more likely to have inadequate knowledge compared to degree students. Year-2 and year-3 participants were more than more than 2 and half times (AOR=2.7; 95% CI 1.2-3.8) more likely to possess negative attitudes than year-4 and above students. Additionally, attitude was significantly associated with respondents’ knowledge level. Participants who had inadequate level of knowledge were 4 times (AOR=4.2; 95% CI 2.4-7.2) more likely to have a negative attitude towards cervical cancer and its screening. Measures of goodness of fit of both models were tested using Hosmer and Lemeshow and Nagelkerke R2 and showed acceptable levels.
Knowledge, attitude and practice of cervical cancer and its screening (Pap smear) and associated factors offer vital prospect for wide-ranging prevention and control strategies of the disease. Hence, this study addressed the knowledge, attitude and practice as entry points for the prevention and control of cervical cancer and its associated factors among female undergraduates in OCMHS.
Majority of the students were younger than 22 years of age as more than 60% were second and third year undergraduate students. Most (92.8%) of the respondents had heard about cervical cancer, greater than the result of a similar study in Ethiopia where 76.8% of college students had heard about cervical cancer18 and in Dominica.23 This is not surprising as the respondents were health professionals exposed to extensive sensitization on the dangers of cervical cancer. The findings of our study showed that 54.4% of participants had an inadequate knowledge, more than the result of an Ethiopian study where 43.2% were not knowledgeable18 but lesser than a Nepalese study finding, which showed poor knowledge adequacy of participants (65.6%).24
The main sources of information, in descending order, were course lectures, books, media, hospitals, friends and others (including families). This result portrayed that the media, health workers in hospitals and the society were not equipped with ideas to contribute on health education and promotion of cervical cancer and its screening. This was consistent with the study conducted in India where 47% had obtained their knowledge from books.25 Regarding the knowledge of symptoms of cervical cancer, participants were aware that vaginal bleeding between periods, painful coitus and bleeding after intercourse were some of the symptoms as reported by 52.4%, 58.8% and 58% respectively and these findings were similar to other studies.26,27 As observed from our study, only 58% reported that cervical cancer is a preventable disease. This result alarms the lack of awareness about cervical cancer in educated women. A far better result was observed in another study where 81.5% were aware that cervical cancer was preventable.28
Only two participants in this study had ever been screened with Pap smear while the rest restrained for many reasons, primarily because they never had sexual intercourse before, were confident over their health and were too young to be screened. Level of practice was grossly low in others studies as well.29–31 This depicts elimination of certain barriers that negatively affect screening like socio-cultural taboos and rarity of open sexual discussions, and strengthening health promotion integration in the curricula, media, and society will aid in increasing the number of women participating for screening. The recommended Pap screen testing should begin at the age of 21 and routine screening is recommended every three years until the age of 65.6 Thus, it should also be noted that most of the participants in this study were less than the age of 22 years of age and almost all were unmarried.
The study demonstrated that 50.8% of respondents had a positive attitude towards screening for cervical cancer, which is comparable to other African studies.30,32 The scoring method used in these studies was, however, different. Pap smear was regarded as helpful by 92.9% participants and 84% claimed that they would encourage their friends, daughters or mother to get screened. However, majority (67.6%) of the respondents did not know that there exists a Pap smear program in Eritrea. Additional 10% believed that there is no screening program in Eritrea and 58% did not believe that they were candidates of the screening service after the of age 21. The incognizance of Pap smear existence and the aforementioned low health-seeking behavior for screening could be explained by the inability to bring a behavioral change. Behavioral interventions for prevention and control of cervical cancer have been given low attention that the level of awareness about screening behavior among women is low.
There was a significant association between age, year of study, level of education and knowledge of the respondents towards cervical cancer and Pap smear. Participants in younger ages (18-21), diploma students and earlier years of level of education (second and third year) were more likely to have inadequate knowledge levels. This could be due to the students’ level of exposure to different medical courses that may affect their knowledge. According to the results of this study, the discrepancy of knowledge between age, level of study and year of study requires attention as the nature of the disease basically necessitates females of young age to have an adequate awareness and knowledge, and more importantly, be introduced to every department’s curricula.
The study showed that there were significant associations between year of study, knowledge levels and the attitude towards cervical cancer screening. Year-2 and 3 students were more likely to have significant negative attitude. It is also shown that participants who had knowledge inadequacy were more likely to have negative attitude towards cervical cancer and Pap smear. The willingness for Pap smear exam was poor despite the levels of education of the students and even considering the proximity of the college to the screening service- which is located less than one kilometer away. Similar results were demonstrated in Ethiopia and India33,34 and such a paradox requires a paradigm shift because these health professionals are at equal risk of the disease they educate their clients to. Strong interplay between the domains of knowledge and attitude for prevention and control of cervical cancer was also consistent with an Ethiopian study.35
The strength of the study is that it has a very high response rate (99.2%) when compared to other similar studies and it caught most of the selected respondents. Secondly, it was the first study to assess knowledge, attitude and practice about cervical cancer and Pap smear among students in Eritrea, where the incidence of the diseases remains unknown.10 Finally, the study used validated questionnaire with pretest and experts’ advice. Limitations of the study were that
The study showed that a vast majority of respondents had heard about cervical cancer. Less than half had adequate knowledge about cervical cancer and its screening and most of the respondents did not know the existence of Pap smear program in Eritrea. Half of the total participants had a favorable attitude towards cervical cancer screening, but the practice of Pap smear was tremendously low. The study also elucidated on awareness of the students as an indirect measure of screening advocacy, public education and information dissemination on the availability of the screening test (Pap smear).
On the basis of the results of the study, we recommend increased efforts from the government to increase the awareness of women on cervical cancer and its screening through various health education, barrier-specific counseling and mass media. We also recommend a strong emphasis be given on informing and advertising the ongoing Pap smear screening program in Eritrea, as its existence remains unknown to the majority. The college itself has to be able to launch campaigns and distribute educational pamphlets and posters to raise the knowledge and perception of Pap test. In line with the previous population-based study done in Eritrea,10 we recommend training of more health care workers on Pap smear testing and expansion of Pap smear test in various referral hospitals despite the ever competing health care priorities. Moreover, a further community-based study that integrates qualitative study design is suggested at a national level to increase the representation of all female population.
This research received no specific grant from any funding agency in the college, public, commercial, or not-for-profit sectors
All the authors made substantial contributions to the conceptualization of the study and supervision of the design of study, acquisition of data, and analysis of the data; contributed to writing of the manuscript and revising it critically for intellectual content; approved the submitted version of the manuscript and agreed to be accountable for all aspects of the work.
The authors would like to thank OCMHS for its approval, clearance, follow up and decision on dissemination of findings. Much appreciation to Mr. Daniel Abraham, Mr. Awet Tesfahanis and Mr. Yonas Habte (BSc Nurses) who assisted during data collection and Mr. Medhanie Asrat who assisted during data entry and cleaning process. We are also grateful for the college’s pupils who participated in the study.
The authors of this study declare that there was no conflict of interest.

©2021 Mekonen, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.