MOJ
eISSN: 2374-6920


Nanoparticles (NPs) are particles between 1 and 100 nanometers in size. They are currently the most sought-after and studied field of science, and have become the materials of choice in various nanomedicine applications due to their uniqueness in interacting with a plethora of materials including polyethylene glycol (PEG) Figure 1.
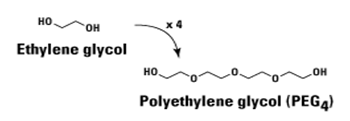
Figure 1 PEG is an FDA-approved polymer employed in several biomedical and nanomedical applications. It is a hydropilic chemical compound with repeating ethylene glycol units:
Currently, there are more than 35 US FDA-approved NPs utilizing PEG in their biomedical applications. PEGylation, which is the addition of PEG to the NP formulation, provides immunity from the hostile biological environment. The ‘stealth’ property, further confers on the PEG-NP formulation benefits that are not normally provided by other polymers. This mini-review briefly describes the mechanisms of action, as well as the benefits and challenges of PEG and PEGylation in cancer therapy.
Upon administration, NPs are recognized and cleared from circulation by the phagocytes from the reticuloendothelial system (RES). The circulation time of the NPs is largely determined by their surface structure and their hydrophilicity/hydrophobicity state that governs the amounts of opsonins absorbed. The process of opsonization (opsonin-NP binding) reduces the circulation time of the NPs. Reports indicate that the PEG polymer on the NP surface increases the circulation time by reducing this opsonization process, thereby preventing recognition by monocytes and macrophages, allowing the NPs to remain longer in the blood pool.1 In addition to NP–RES interactions, poor circulation times can also arise from NP–NP interactions, where NPs with a high surface energy have a greater tendency to aggregate as described by the Derjaguin-Landau- Verwey-Overbeek (DLVO) theory.2
PEGylation of small proteins, peptides, and oligonucleotides, has also become an increasingly common method of improving the half-life of biological products, mainly through reducing the urinary excretion of the molecule.3 Many other successful experimental assays depend on the ability to re-engineer the solubility, size, and other properties of drugs, peptides or proteins, in their interactions with PEG in an effort to increase the resident time in circulation. PEGylation, if empirically researched on, would become a very useful method of making these modifications.
The maor benefits from the use of PEG in NP formulations derives from its “stealth’ properties, as well as the increase in circulation times for the NP conjugates. Clearly, the addition of PEG to the NP formulation increases the retention and circulation time by reducing uptake by opsonins in the RES. It was reported previously that particles remained in rat circulation 40-times longer when coated than uncoated with PEG.4 Additionally, incorporation of dioleoyl N-(monomethoxy polyethylene glycol succinyl) phosphotidylethanolamine (PEG-PE) into posphatidylcholine: cholesterol liposomes (1:1) increased the retention time from thirty minutes to five.5 By virtue of the fact that PEG is hydrophilic, the serum and other solvent solubility also increases, further enhancing the circulation time. These merits also result in higher targeted and accumulated PEGylated NPs than non-PEGylated counterparts.
The acute or chronic administration of PEG of different molecular weights using varying routes has also not led to any major toxicities. Further, signs of toxicity that do occur are only apparent at high doses. In the light of this information, PEG can be considered to have a toxicological profile of very low concern in animals, and by extension, humans.6
Immunogenicity has also been reported, but generally less so than the immunogenicity of the NP.7 Furthermore, repeated injections of PEGylated material show markedly decreased circulation times. This `accelerated blood clearance' (or ABC effect), is thought to be a result of increased splenic production of IgM.8
One challenge with immunity is the extent to which the PEG size is modified in vivo in order to affect NP immunity. For instance, the degradation of PEG has been reported to increase with increasing NP size. This observation has led to the postulation that the degradation products of PEG diffuses out of the particles easily, whereas they are more likely to remain within the core of the polymer for longer periods to effect the degradation.9
There are however some fundamental challenges that hamper NP deployment to the clinic. These include residual uptake by the RES, in which NPs are transported from circulation to the liver or spleen, as well as nonspecific binding of NPs to non-targeted areas.10 Another challenge of PEG is degradation by natural or mechanical forces like heat and light, which can fragment the PEG, resulting in reduced cloaking ability.10
The principal challenges of PEGylating macromolecules are identifying the specific sites of PEGylation and characterizing the final product created when a high molecular weight PEG molecule is attached to a low molecular weight drug molecule. When properly designed by taking cognisance of these militating factors, a PEGylated drug exhibits increased half life, greater bioavailability, and reduced clearance, which more than compensate for its reduced target binding.11
The generalized use of PEG in various therapies which was initially dismissed as relevant in clinical trials, has now been superceded by the myriad of PEG-modified products that seem to meet the regulatory authority requirements. Some of the clinically used PEG conjugates either in the market or clinical development are listed in Table 1 below.
Product name |
Description |
Clinical use |
Oncaspar |
PEG-asparaginase |
Acute lymphocytic leukaemia |
Adagen syndrome |
PEG-adenosine deaminase |
Severe combined immune deficiency |
Somavert |
PEG-HGH antagonist |
Acromegaly |
PEGIntron |
PEG-Interferon alpha 2b |
Hepatitis C |
NeulastaTM |
PEG-rhGCSF Chemotherap |
Chemotherapy-induced neutropenia |
CimziaTM disease |
Mircera PEG-EPO |
Anaemia associated with chronic kidney |
Puricase |
PEG-uricase |
Gout |
Macugen |
PEG-aptamer |
Age-related macular degeneration |
Table 1 PEG-modified therapeutic conjugates.9
Due to its high biocompatibility, protection from the body’s immune system, as well as the low interactions with blood components, PEG is currently the only hydrophilic polymer accepted in various cancer therapeutic protocols. Some of the PEGylated drugs like peginterferon α and pegfilgrastim have proven to not only exhibit stealth property against the immune system but also cost-effective.to be not only stealth, but also cost-effective.
Proteins used in medicine, e.g. interferon, are immunogenic and they are quickly broken down by the body. Pegylation is a recognized way of preserving their integrity and reducing immune reactions, and works well with enzymes used to degrade amino acids, a recent focus of attention in cancer therapy.12 Several other products including pegvisomant and certolizumab pegol have also proven to be effective and they are in high demand.10
Overall, PEGylation of proteins has become an essential engineering strategy in the delivery of biopharmaceuticals. While touting all these potential biomedical advantages, the area in PEGylation research which undoubtedly needs critical attention is cell-specific targeting. Even though various design platforms for enhanced targeting are now being experimented for introduction into the market, it would be appropriate to first conduct specific and empirical investigations on the currently introduced peptide fragments of PEGylation, before the commencement of clinical trials.
None.
The author declares no conflict of interest.

© . This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.