MOJ
eISSN: 2374-6939


Research Article Volume 10 Issue 2
Said Ait Messaoud?ne Military Hospital, University of Algiers, Algeria
Correspondence: YacineTalbi, Said Ait Messaoudene Military Hospital, University of Algiers, Cite 445 Lgt, Bt 25, Sidi Menif. Zeralda, Algeria, Tel 214000000000
Received: March 13, 2018 | Published: April 11, 2018
Citation: Talbi Y, Yacine N, Amer O. Video thumb mobility assessment. MOJ Orthop Rheumatol. 2018;10(2):135-137. DOI: 10.15406/mojor.2018.10.00401
Thumb mobility represents 40% to 50% of hand function.1,2 The thumb is able to make simultaneously or separately several movements, thus it can carry out the retropulsion, abduction, adduction, antepulsion, opposition, flexion, extension and the pronation-supination. The combination of these various movements led to circumduction which is a combined movement that starts with the maximum abduction retropulsion to antepulsion, continuing by the opposition and ending by the flexion.
Thus the trapezeus-metacarpal, metacarpophalangeal and interphalangeal joints give to thumb a large degree of mobility, with two degrees of freedom3–5 and a negligible rotation degree.4,6
The complexity of these movements makes it difficult to assess thumb mobility; that is why, several studies were carried out to evaluate thumb mobility and some assessed this mobility in only one plan,5,7 others assessed it in two plans4,8-11 and others assessed it in three plans,12,1,13 but no consensus has been used so far for the quantification of thumb mobility especially in clinical practice.
In this study, we suggest a method of thumb mobility assessment in only one plan, simple execution, within the reach of any surgeon in a consulting-room; this method is able to calculate the thumb circumduction surface, thus, including all combined movements of the thumb, giving an overall assessment of the thumb mobility.
We assessed 30 participants (11 women and 19 men); we excluded all participants who had a thumb injury, a paralysis or after-effect of paralysis of one of the three nerves of the upper limb. The average age was 37 years (50-20 years); we assessed the thumb mobility by asking the participants to make a full circumduction movement. We assessed the mobility of the two thumbs in order to compare the results.
Circumduction is a movement which starts by maximum abduction retropulsion of the thumb in the same plan as the palm of the hand, through the antepulsion where the thumb becomes perpendicular to the palm of the hand with a maximum metacarpophalangeal and interphalangeal extension and a maximum opening angle between the first and the second metacarpal, then the opposition which combines 15° to 20° of metacarpophalangeal flexion with a thumb pronation and finally the movement finishes by a flexion which combines a maximum flexion of metacarpophalangeal and interphalangeal, putting the pulp of the thumb in contact with the head of the fifth metacarpal.
Our method measures the surface of thumb circumduction in its maximum amplitude, for that we used a standard digital camera for the video and two software which are available in any hardware store. The first is vector graphic manipulation software called Adobe Macromedia Flash to plot the curve including the thumb movement, the second is computer-assisted design software called Autocad for the calculation of the surface.
Video footage captures
Patient is placed in front of the camera; the slight shoulder adduction allows a maximum supination of the forearm, the elbow in a certain degree of flexion, the wrist and metacarpophalangeal joints are maintained by a splint with Velcro strips, avoiding all parasitic movement at the level of these two joints that can distort measurements. The splint should be thick enough to allow a maximum retropulsion of the thumb compared to the work plan (Figure 1). The camera is positioned on the same work plan as the patient’s hand, in the axis of the third finger. A centimetric measurement support is positioned in the same plan as the tip of the thumb in order to be used as a measurement scale for later calculation of the surface. In this case the distance separating the camera with the patient’s hand does not affect the result, since we have a fixed centimetric scale.

Figure 1 Video footage captures. Patient is front of the camera allows maximum supination and retropulsion of thumb.
Then, you ask the patient to make the thumb circumduction movement, taking video footage from the beginning to the end of the movement.
The video recording of the movement is transferred to Adobe Macromedia Flash, which marks a point on the tip of the thumb pulp every ten pictures from the beginning to the end of the movement, then, the points are connected to each other from of the first to the last closing the loop (Figure 2).

Figure 2 Movement contour tracing. Marks a point on the tip of the thumb pulp every ten pictures from the beginning to the end of the movement and we trace one centimetre on the centimetric support.
On the same video, you trace on the centimetric support the length of 01 centimetre, this one will serve as scale for the later calculation of surface; in this way, the calculation will be accurate with no risk of error since centimetric measurement is unchangeable. In this case, the distance which separates the camera from the hand will not affect the results of calculations since the scale is fixed (01cm).
The movement contour tracing and the marking of centimetric measurement are then transferred on Autocad for the surface calculation (Figure 3). The measurement scale of will be the centimetre taken with the curve, on which Autocad is based for the calculation of the circumduction surface. Thus, you obtain a surface in square centimetre with a millimetre-length precision.
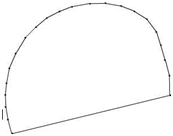
Figure 3 Calculation of the area. We transfer the measurement scale and the curve on Autocad for calculation of the surface.
In our study, the two hands were assessed; we started with the dominant hand, then the controlateral hand in the same way.
The obtained results on the dominant hand were compared with the controlateral hand. You noticed that the obtained surfaces between the two hands are almost identical; in this case, during the assessment of a pathological thumb the results will be compared with the healthy thumb to quantify the exact deficit of the thumb mobility (Table 1).
|
Left thumb |
Right thumb |
1st patient |
110,98 cm² |
111,22 cm² |
2nd patient |
138,11 cm² |
138,39 cm² |
3thd patient |
63,84 cm² |
64,12 cm² |
4th patient |
137,21 cm² |
137,30 cm² |
5th patient |
82,56 cm² |
82,78 cm² |
6th patient |
96,78cm² |
96,91 cm² |
7th patient |
108,63 cm² |
108,88 cm² |
8th patient |
95,88cm² |
96,00 cm² |
9th patient |
126,46 cm² |
126,52 cm² |
10th patient |
138,58 cm² |
138,43 cm² |
11th patient |
104,66 cm² |
104,78 cm² |
12th patient |
122,03cm² |
121,87 cm² |
13th patient |
113,08 cm² |
113,21 cm² |
14th patient |
99,41 cm² |
99,60 cm² |
15th patient |
128,00 cm² |
128,05 cm² |
16th patient |
130,23 cm² |
130,34 cm² |
17th patient |
114, 80cm² |
114,82 cm² |
18th patient |
89,04 cm² |
89,11 cm² |
19th patient |
123,12 cm² |
123,31 cm² |
20th patient |
112,61 cm² |
112,54 cm² |
21th patient |
135,77 cm² |
135,54 cm² |
22th patient |
88,02 cm² |
87,93 cm² |
23th patient |
129,00 cm² |
129,28 cm² |
24th patient |
110,84 cm² |
110,77 cm² |
25th patient |
132,21 cm² |
132,33 cm² |
26th patient |
89,98 cm² |
90,03 cm² |
27th patient |
129,74 cm² |
129,59 cm² |
28th patient |
79,49 cm² |
79,64 cm² |
29th patient |
93,88 cm² |
93,69 cm² |
30th patient |
101,79 cm² |
101,62 cm² |
Table 1 Assessment of a pathological thumb the results will be compared with the healthy thumb to quantify the exact deficit of the thumb mobility
Consequently, you can assess the pathological thumb preoperatively then postoperatively to evaluate the mobility gain and compare results with the healthy side to assess residual postoperative deficit.
Most suggested methods to evaluate thumb mobility were carried out in laboratories with sophisticated material;12–14 we developed an easy evaluation method of thumb mobility, doable by any hand surgeon in consultation.
The obtained results did not show any difference between both hands, enabling the clinician to have a reference (healthy thumb) to use for the pre and post operative assessment of the pathological thumb. Using a centimetric support in the same plan that the thumb enables to have an unchangeable scale for the calculation of the surface; in this case, regardless the distance which separates the camera from the hand.The obtained results will be real and accurate.
The limitation of this method is the thumb mobility assessment in only one plan of space compared to other methods,12–14 but which seems sufficient for clinical practice since this method assesses the overall surface of circumduction, which gathers several thumb movements and which can be used by all hand surgeons in consultation.
The only risks of miscalculations are due to the fact that patients do not carry out the same mobility amplitudes during circumduction. Several methods assessed thumb rotation during circumduction, Sartorius used a goniometer for the calculation of thumb mobility amplitudes,7 Duparc et al.15 used metal pins on thumb and second finger and used an anthropostereometer to measure thumb circumduction. Jakobs & Thompson10 suggested a classification to score thumb opposition, angle of the nail plan compared to palm of the hand.
Bunnel16 used toothpicks attached on the thumb to show thumb rotation at 90° during circumduction, Boys compared the angle thumbnail compared to the hand palm and tested the distance between the thumb pulp compared to the third finger.17 Cooney et al.4 attached markers on phalange and metacarpals of the thumb and third finger to study space relation between trapezius and the third finger.
Foucher used a special device to measure Van Wetter's Apogee and Duparc opposition angle circumduction was measured according to Kapandji quotation.18 Coert13 described a technique to assess thumb rotation during the circumduction using a camera which emits an infra-red light and sensors attached on the thumb. Tang14 calculate thumb functional space during circumduction and concluded that the thumb moves to 60% of its total mobility in the abduction/adduction and flexion/extension during its functional mobility.
Zhang12 used 5 cameras, with markers placed on the thumb and long fingers and calculated the rotation centre and the thumb activity sphere in 3d. The trapezoid-metacarpal, metacarpophalangeal and interphalangeal joints are very complex, the thumb mobility is ensured by several intrinsic and extrinsic muscles, innervated by three different nerves. Each nerve injury can generate a different functional deficit of the thumb mobility. It seems that no method so far can assess in a comprehensive way this complex mobility of the thumb.
In most cases, these assessments are carried out in laboratories impossible to reproduce in consultation. The strength of our method is that it requires no specific material; it is simple to perform, reproducible, reliable and can be used for the assessment of any thumb pathology, whatever is paralytic, traumatic or osteoarthritis.19-21
None.
Authors declare there is no conflict of interest in publishing the article.

©2018 Talbi, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.