MOJ
eISSN: 2374-6939


Case Report Volume 6 Issue 6
Largo Medical Center, USA
Correspondence: Michael Venezia, Largo Medical Center, Florida, USA
Received: August 12, 2016 | Published: December 19, 2016
Citation: Venezia M, Braunlich P, Marcotte A (2016) Stabilization Method for Hip Fracture Fixation in Patient with Below Knee Amputation. MOJ Orthop Rheumatol 6(6): 00243. DOI: 10.15406/mojor.2016.06.00243
Hip fractures are becoming ever more common with the aging population. With the expanding list of these patient’s co-morbidities, those will lower extremity amputations will continue to present unique challenges to orthopedic surgeons. Our case study examines an 81-year old male with a basicervical hip fracture and an ipsilateral below-knee amputation. The standard fracture table and reduction techniques offer very little assistance in achieving an anatomic reduction of the fracture. Our case offers an alternative technique using standard equipment.
Hip fractures are common injuries and can comprise up to 20% of the workload for an orthopedic trauma unit.1 An estimated 250,000 occur annually and that number is expected to double by 2040.2 The incidence of femoral neck fractures grows exponentially with increasing age and the mechanism of injury is often secondary to falls. The risk of a second hip fracture within 2 years is nearly 10% in women and 5% in men. And in those patients sustaining a second hip fracture, 70% will be of the same type. There is little debate when it comes to the management of hip fractures, which are consistently treated with fixation.1
Basicervical femoral neck fractures can be effectively treated by open reduction and internal fixation using an intramedullary nail device. Traditionally, reduction in the OR is attained through precise positioning of the patient on a fracture table using a traction boot to control the reduction. When encountering a patient with a below-knee amputation (BKA), this clinical scenario becomes more complicated and many times will require an alternative approach to obtain an accurate reduction. Absence of the lower extremity provides a challenging situation that necessitates further discussion on how to obtain an appropriate reduction, while still using the standard fracture table. Our case focuses on overcoming this difficulty and provides a novel approach for the positioning of open reduction and internal fixation of these fractures in patients that have a concomitant below knee amputation. We hypothesize; this technique will allow for an anatomic reduction while minimizing struggling during positive and will achieve a comparable outcome to standard practice.
An 81-year-old man presented to the emergency department with a history of a fall while trying to pivot on his prosthesis. He complained of left hip pain, radiating into his groin. Pain was also elicited with log roll. He had a history of a left below-knee amputation following a history of peripheral vascular disease with a failed bypass procedure. Radiographic evaluation revealed a displaced basicervical femoral neck fracture of his left lower extremity (Figure 1).
After medical clearance was obtained and discussion was had with the patient, decision was made to undergo operative intervention due to his prior ambulatory status and functional level. On pre-operative planning the decision was made to treat the patient with Intramedullary Nail fixation utilizing a long, statically locked nail. A literature search was then subsequently used to plan for the patient positioning on a fracture table, we felt none of the literature provided an exact technique that we felt would work best for the patient, the below technique was used as described.
The patient was positioned on the fracture table (OSI Modular Table System) with a perineal post present to stabilize the patient. Initially we attempted to position the patient using the reverse surgical boot method.1,4 but ultimately felt this position compromised the ability to control the reduction and due to the boot size did not enable us to utilize any of the distal locking screws within the nail itself. We proceeded to place a tibial traction pin through the stump of the patient’s ipsilateral tibia at the described insertion site 2.5cm posterior and distal to the tibial tubercle (Figure 2), under sterile conditions prior to operative preparation and draping. We then used the disposable tibial traction arm applied to the pin and hooked the arm onto the base of the traction boot with said boot removed (Figure 3). This technique allowed an assistant to control rotation, traction, and abduction/adduction of the ipsilateral leg into a position for acceptable reduction from the base of the fracture table as if the boot was in use and controlled within the limitations of the table. This setup allowed us to obtain and maintain an acceptable reduction and allowed for intraoperative freedom while inserting the IM device as well as interlock distally without any impedance or difficulty in maintaining or reduction (Figures 4 & 5).

Figure 2 A tibial traction pin is placed through the stump of the patient’s ipsilateral tibia 2.5cm posterior and distal to the tibial tubercle.

Figure 3 The disposable tibial traction arm applied to the pin and hooked the arm onto the base of the traction boot with surgical boot removed.

Figure 4 AP view of the left hip showing acceptable reduction and surgical fixation with an intramedullary nail.
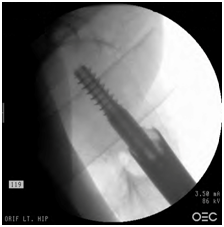
Figure 5 Lateral view of the left hip acceptable reduction and surgical fixation with an intramedullary nail.
On post-operative follow-up, the patient initially followed up 1 month following the surgery. He complained of mild left leg pain, and erythema, swelling and tenderness of the incision. He required a wheelchair for ambulation. Plain films demonstrated no change in alignment of the fracture since surgery. He was encouraged to engage in ROM exercises as the joint is not immobilized. On the 6-month follow-up, the patient had transitioned to using a walker to assist with ambulation. X-rays showed delayed healing of the fracture, but also revealed no change in alignment of the fracture.
Management of basicervical femoral neck fractures in the elderly usually requires operative intervention, with intramedullary fixation being a mainstay in treatment options. When encountering a patient who also has an ipsilateral BKA, an additional challenge presents itself for which solutions have been described.
Several other methods have been described in the literature that we felt were not appropriate for our patient but have proved useful in other patients. The reverse boot method utilizes the fracture table by inverted the fracture boot to accommodate and stabilize the patient’s stump while allowing for control of the reduction.4,5 These patients rehabbed better, were discharged home earlier and started ambulating with their prosthesis sooner than those positioned with traction pin.4 In addition, this technique uses standard equipment, takes less time, is non-invasive and avoids an additional source of infection.5 Manual traction method points to completely forgoing the surgical boot and using an assistant to control the reduction manually. The patient is transferred to the fracture table, the contralateral extremity is secured, and the assistant grasps the extremity and holds it in the best position for reduction.6 Skin traction is another method that could be attempted to the extremity while the patient is positioned on the fracture table to achieve an anatomic reduction.7
Although the standard fracture table can be used, use of the traction boot typically does not allow for access to the distal portion of the femur for interlocking the nail. Thus, the use of a single tibial traction pin in combination with the use of the traction arm attached to the fracture table as shown and described below allows for secure positioning of the patient, along with the best ability to achieve and anatomic reduction and stabilization in more unstable fracture patterns. While the technique described is certainly an adaptation of other methods used in the past, we believe that the attention to detail in the use of the traction boot base along with tibial traction allows for the surgeon to best address these fractures and increases the likelihood of obtaining an appropriate reduction with the least amount of intraoperative struggle. There are multiple described methods for appropriate setup of the affected extremity, which we believe all play an important role in the treatment of this patient population. Our goal was to provide an additional tool in the surgeon’s arsenal.
We believe that the techniques mentioned here to overcome this problem are reliable and give the surgeon another option in treating these fractures in this patient population.
None.
None.

©2016 Venezia, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.