MOJ
eISSN: 2374-6939


Case Series Volume 13 Issue 2
Orland Park Orthopedics, USA
Correspondence: Blair A Rhode MD, Orland Park Orthopedics, 16450 S 104th AV, Orland Park, IL 60467, Tel 708- 364-8441, Fax 708-364-8443
Received: March 19, 2021 | Published: April 8, 2021
Citation: Rhode BA, Rhode WS. Return to work after arthroscopic rotator cuff repair in a worker’s compensation population. MOJ Orthop Rheumatol. 2021;13(2):21-24. DOI: 10.15406/mojor.2021.13.00541
By focusing on arthroscopic rotator cuff repair in a worker’s compensation patient population that are without personal injuries, previous ipsi-lateral shoulder injury, any concomitant pathologies or being federal employees, the rate of return-to-work (RTW) can be better isolated as an outcome of the surgery. RTW rate for a consecutive 50 patient cohort was 98% with 58% achieving full duty. A single patient with a frozen shoulder was unable to return to work at any level. These RTW rates contrast with several previous studies that reported significantly lower RTW rates for workers with compensation than workers without compensation. All but three patients improved their UCLA scores after the repair.
Keywords: arthroscopic shoulder repair, worker’s comp, time to Maximum medical improvement
WC, Worker’s comp; DOL, Department of Labor; DOI, Date of Injury; MMI, Maximum Medical Improvement; tMMI, time to MMI; WS, worker status; UCLA, University of California score; ARCR, arthroscopic rotator cuff repair; RTW, return-to-work
Failure rates for arthroscopic rotator cuff repair (ARCR) have been reported between 7-14% for tears less than 1cm1–3 and high as 94% for massive tears.4–8 Failure rates have been correlated primarily with tear size, patient age, and tissue quality. Varying repair techniques have offered differing results with newer studies pointing to minimal differences in success rates when employing modern repair techniques (double row, complex simple, modified mason Allen) and newer technology (lateral row and triple loaded anchors).9
While many studies support the efficacy of ARCR, most studies often report that the level of success in the workers compensation (WC) population is inferior to that of the general population.10–13 In a study of success rates as defined by patient satisfaction and return-to-work (RTW), WC patient RTW rates often appear to lag the general population. For example, in patient population of 107 (24 WC and 83 non-WC) 41.6% of WC patients and 89.2 % of non-WC patients returned to full duty.9 Reasons given for the different outcomes include legal representation, stigmatization, power imbalance, higher stress14 and perceived blame by the worker.15
Workers’ Compensation is a state mandated no-fault system form of insurance that ensured that workers injured at work would receive compensation without delay and without regard to fault.16,17 It is a benefit provided in exchange for mandatory relinquishment of the employee’s right to sue his or her employer under the common civil law of negligence. The primary stakeholder in workers compensation is the injured worker seeking timely access to care and the employer/insurer tasked with providing this access. Unfortunately, there often exists a severe power imbalance between the injured worker and the insurance company that is responsible for allowing timely access to appropriate treatment. This can result in mental stress during the ongoing pursuit of compensation.
Patient perceived outcomes are often tempered by numerous previously discussed factors. While the patient as a biopsychosocial construct is important when assessing outcomes, the worker- compensation patient should be evaluated based on the most important outcome measure, RTW.
This is a retrospective case series to evaluate RTW rates and work levels in 50 consecutive patients that sustained a work-related rotator cuff tear. All patients were treated by a single fellowship trained sports medicine orthopedic surgeon. Patients underwent an arthroscopic rotator cuff repair with surgical technique determined by tear size and pattern. All patients underwent a standard post-operative course with gradual advancement to RTW as determined by the treating surgeon.
This is a retrospective case series of 50 consecutive worker’s compensation (WC) patients. Patients excluded were non-WC, personal injury, federal employees, previous ipsi-lateral shoulder injury, and any concomitant pathologies. 50 patients satisfying the selection criteria include 13 females average age 52.2yrs and 37 males with average age of 49yrs. Patients were assigned a Department of Labor (DOL) category of medium to heavy effort. Data analysis included an initial numeric score based on the job demands of 1 for light duty to 5 for heavy duty. Final work status numeric assignment was based on ability to perform work at one of eight levels: 0-off, 1-no use, 2-sedentary, 3-light, 4-light medium, 5-medium, 6-medium heavy, and 7-heavy = full overhead work. Initial and final UCLA scores were recorded.
Dates recorded included: date of injury, date of 1st physician visit, date of surgery, and Maximum Medical Improvement (MMI) date. Thirty-four patients were given physical therapy, 30 had injections, and 14 had neither.
Rotator cuff tears were documented in centimeters (cm) in the AP (anterior/posterior) direction, cm in ML (medial/lateral) direction, and the tear area in cm2 (= AP*ML). The rational for using tear area is that it provides a single number that encompasses tear-severity based on both AP and ML lengths. ML length relates to the number of tendons torn.
All patients underwent an arthroscopic rotator cuff repair by a single, fellowship trained, sports medicine orthopedic surgeon. Repair technique was dictated by tear pattern, tear size and tissue quality. Modern repair techniques were used including simple repair with triple loaded anchors, modified Mason-Allen repair and double row repair. All patients received iliac crest bone marrow aspirate. Outcomes were not analyzed by repair technique due to potential selection bias for a particular repair technique relative to a specific tear pattern.
The DOL category for this cohort classified 32 males and 3 females as ‘heavy’ duty, 14 patients were medium or medium/heavy and one at light duty. The average DOL scores were: 4.76 for males (Light-medium to Medium), 3.46 for females (Light to Light-medium), and 4.42 (Light-medium to Medium) for all. The important outcome of ARCR for workers is their ability to return to fruitful employment and the level of effort they can perform at. 29 patients attained full work status, 6 at medium/heavy, 4 at medium, 5 at light/medium, 5 at light duty and one individual at sedentary status. Overall, 39 of 50 patients were able to RTW at a medium or higher level of activity. Of the patients that did not achieve full work status, 13 could lift 10 to 35-lbs overhead, 6 were limited to 5 lbs overhead and one to 0 lbs.
UCLA scores after ARCR improved on average by 13 points with a maximum improvement of 24 points (Table 1). The top final UCLA score was 35. Individual score improvements are illustrated in Figure 1 where the solid line indicates the final score is unchanged from the index score. Repair of two massive tears (below the solid line) showed no improvement along with one RC repair that experienced post-operative adhesive capsulitis.
|
Statistic |
Index UCLA score |
Final UCLA score |
Final - index UCLA |
|
Average |
13 |
25.64 |
13 |
|
Std dev |
3.41 |
6.49 |
7.23 |
|
Minimum |
6 |
9 |
-4 |
|
Maximum |
8 |
36 |
24 |
Table 1 UCLA scores before (Index) and after ARCR
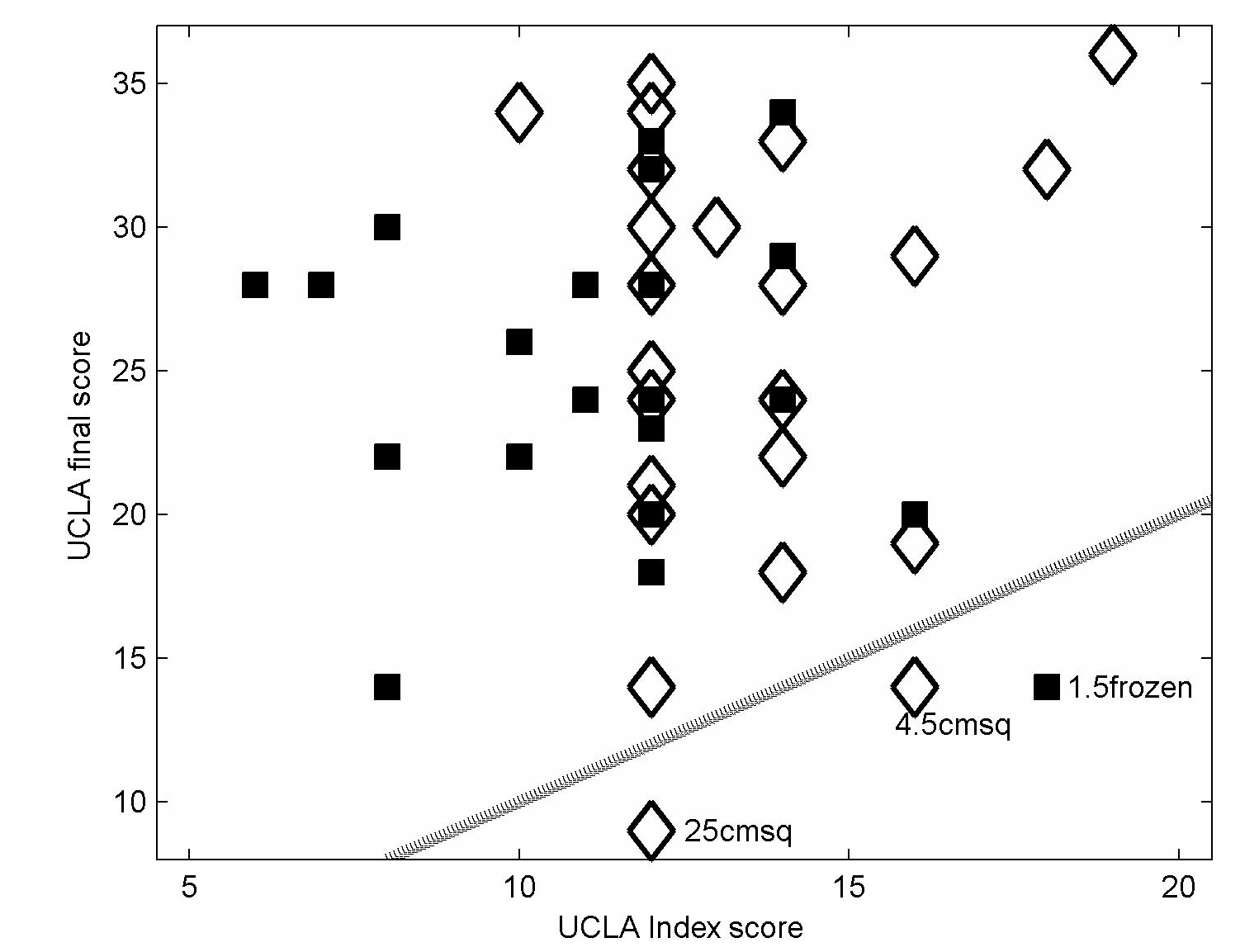
Figure 1 Comparison of UCLA final scores and UCLA index score for each patient. Filled symbols correspond to repairs of RC tears <=3cm2 and diamond symbols indicate results for RC tears >3 cm2. The solid line indicates final UCLA score = index UCLA score, i.e. no change in the UCLA score after repair. Tear sizes for the three cases that lie below the no-change line are listed by each symbol.
RC tear size has been identified as a major factor in RTW outcome after ARCR. As such, the patient population was divided into two groups based on the area measurement of the tear with area >3 cm2 considered a large/massive tear size shown as ‘diamond’ symbols in Figure 1 along with smaller tears indicated by filled square symbols. Patients with smaller tears had a UCLA average index score of 12 versus 14 for large tears. A two-tailed ttest18 yielded a P-value of 0.0321. The difference was significant though unexplained. However, the UCLA final average for patients in both tear size groups was 26 with a test P-value =1.0, indicating no difference.
The work status outcome based on this categorization indicated that 29 out of 50 patients achieved full work status irrespective of tear size (Table 2). 33% of patients with large tears were restricted to light or light/medium WS versus 7.7% of patients with tears < 3 cm2.
|
WS_number |
Tear <=3 cm2 |
tear>3 cm2 |
|
2-sedentary |
1 |
|
|
3-light |
1 |
4 |
|
4-light_medium |
1 |
4 |
|
5-medium |
3 |
1 |
|
6-medium_heavy |
5 |
1 |
|
7-heavy |
15 |
14 |
Table 2 RC tear size influence on work status (WS) outcome
Irrespective of tear size, 70 % of patients achieved a medium-heavy or heavy RTW classification (Table 2). Patients with smaller tears failed to achieve medium heavy or heavy WS in 6 out of 26 cases (23%) while patients with large tears (>3 cm2) 9 out of 24 cases failed achieving higher WS (37.5%).
There is often a considerable delay between the date of injury and the first visit to a physician depending in part on the patient’s perception of need and medical approval for a visit. The average time between surgery and the first patient visit was 121 days (SD= 79) with a range of 4 to 419 days. Non-approved cases took 14 days longer to surgery than approved cases. The average delay between surgery and date of injury was 195 days (SD=159) with a range of 14 to 885 days. After eliminating two approved cases that had over 800 days delay, the average approved delay was 159 days which was 38 days shorter than that of the non-approved cases. However, due to the importance of returning to work and its accompanying financial considerations for both worker and employer, the more important measure is the time to MMI (tMMI) from the time of surgery. Average tMMI was 8.9 months (268 days) (SD=88.6, minimum tMMI=148 and maximum tMMI= 589 days). Complications: two patients that had spine surgery and one patient had post-operative adhesive capsulitis.
Multiple studies have documented a disparity in ARCR outcomes between WC and non-WC patients.12,13,19 In the Misamore10 study of two patient groups that consisted of 24 WC patients with 10 that had strenuous activity, 13 that had moderate activity and one rated non-manual the comparison group of 79 non-WC patients consisted of 22 judged to be at strenuous levels of activity, 17 at moderate levels and 40 were rated non- manual in their activity. The study reported 42% of WC patients RTW at full duty vs 94% non-WC that RTW at their previous level of activity. Clearly a significant difference due to WC status was found. It should be noted that the groups were not matched cohorts.
A WC vs non-WC surgical outcome disparity occurs for all types of surgery. This was demonstrated by a meta-analysis that found 129 out of 175 studies that reported the presence of worker’s compensation, irrespective of litigation, WC patients had worse outcomes.20 Workers’ compensation claims and associated proceedings increase the time for full RTW.21
In a retrospective analysis of 1773 consecutive patients that had shoulder surgery performed by a single surgeon 77% RTW with 40% at full duty and 37% at light duty.21 The highest RTW rate of 62% was achieved for patients that underwent debridement for calcific tendinitis. Twelve procedures were used for RCR and only those patients that underwent capsular release were the only ones to show a significant improvement in work level within 6 months. The relation to worker’s comp was not analyzed.
Biopsychosocial factors such as power imbalance, stigmatization, perceived blame, and differing contractual agreements when workers compensation is involved may provide a negative bias towards return to work in the WC patient. Other factors such as health status and social difficulties may also create return to work disparities.22 Our study attempted to reduce possible biases by restricting the patient cohort to WC patients with no previous surgeries or comorbidity, personal injury, being federal employees, having previous ipsi-lateral shoulder injury, and any concomitant pathologies in-order-to minimize possible confounding factors. Ninety-eight percent (49 of 50) WC patients returned to work, with 58% achieving full work status.
Additional factors that influence the time to RTW include the time to surgery, access to care issues such as when a patient is allowed to see a surgical specialist, and the time for the insurer to authorize the surgery. Once a patient was seen by the physician, on average 121 days elapsed before surgery similar to a study that found an 82 day delay between consent to surgery and surgery.23 In this study, RTW post-surgery occurred on average in 8.7 months which is comparable to a study of early RTW in a cohort of 55 WC patients that had a mean time to MMI was 7.6 months.24 Using ASES scoring scale they found all patients reported good outcomes while WC-patients subjective outcomes remained inferior to no-WC patients. In a review of a worker’s compensation database involving RCR, even geriatric (>65 yrs) patients RTW about 5 months after either ARCR or open repair.25 Other studies found RTW time ranged from 7.6 to 9.8 months.23,24 WC litigation against an employer invariability results in delayed RTW and increased health-care costs.
Inferior outcomes and higher complication rates were found in a large study (45 WC, 45 non-WC matched by age and sex). WC patients had a higher rate of prior surgery, a confounding variable and a condition avoided in the present study. WC patients had a higher reoperation rate, persistent pain and inferior 2-year outcomes.13 Time to MMI (tMMI) was 1 year on average (364 da), with RTW time nearly 1 year (354 da).
While there is substantial evidence that WC patients have worse outcomes after RC surgery than non-WC patients, there are other studies do not support this outcome. Evidence presented here demonstrates that when confounding factors are controlled and the patient population is relatively homogeneous, WC patients have excellent outcomes after RCR surgery. A majority of patients return to work at full capacity and nearly all workers RTW when a reduced level of work effort is afforded them an outcome that is likely of benefit for all involved parties.
Although our study did not compare the WC patient to the non-WC patient, we feel multiple factors may skew return to work rates. Non-WC patients may have lower job requirements that allow a less demanding return to work. Employer/employee relationships may be damaged and become adversarial due to the workers’ compensation process such that a continued work relationship becomes “poisoned”. Furthermore, when a worker not injured while at work lacks legal rights afforded by the workers’ compensation system, the non-WC patient may simply “work hurt” out of financial necessity. A longitudinal analysis of these patients may demonstrate an attrition of these patients to different, lower demand jobs over time.
In light of all of the negative risk factors for return to work in WC patients, we still achieved a 98% return to work with 58% achieving full duty. Work has been reported to be better than unemployment for both physical and mental health.26,27
None.
The authors declare no conflicts of interest.

©2021 Rhode, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.