MOJ
eISSN: 2374-6939


Case Series Volume 10 Issue 6
Orland Park Orthopedics, USA
Correspondence: Blair A Rhode, Orland Park Orthopedics, 16450 S 104th AV, Orland Park, Illinois 60467, USA, Tel 708-364-8441, Fax 708-364-8443
Received: November 19, 2018 | Published: November 26, 2018
Citation: Rhode BA, Rhode WS. Assessing outcomes of arthroscopic rotator cuff repair in the workers compensation patient: case series. MOJ Orthop Rheumatol. 2018;10(6):365-369. DOI: 10.15406/mojor.2018.10.00451
Outcomes from arthroscopic rotator cuff repair in the worker’s compensation (WC) patient have generally been reported as inferior to the general population although large, dedicated studies of the WC patient are rare. This is a consecutive case series of 69 WC patients that underwent arthroscopic rotator cuff repairs. Tear size (cm2), patient’s age and time to surgery as the principal predictors of outcome and final work status. 65.2% of 69 workers achieved RTW status of at least medium level. 73.4% of patients with tear size ≤3cm2 achieved work status of ≥medium while 31% with tear size >3 cm2 achieved the same status. 5% of the patients were classified as not being able to return to work under any condition. Patients with increasing age and tear size tended to return to work at a reduced capacity. A 10% decrease in the number of patients achieving a RTW status of ≥medium for every 100 days of delay to repair was demonstrated. Most patients return to a medium work level or greater although outcomes are affected by age, tear size and delay in treatment.
Keywords: rotator cuff, arthroscopic, workers compensation, return-to-work, tear size, delay to treatment, age
RC, rotator cuff; RCT, rotator cuff tear; RCR, rotator cuff repair; ARCR, arthroscopic rotator cuff repair; RTW, return-to-work; WC, worker’s compensation; MMI, maximum medical improvement; AP, anterior-posterior; ML, medial-lateral; cm, centimeters; UCLA, University of California, Los Angeles
Arthroscopic rotator cuff repair has increased in frequency significantly over the last decade. Approximately 250,000 patients undergo rotator cuff repair (RCR) annually in the United States, at an estimated cost of $3 billion.1,2 Outcome studies using ultrasound and MRI report 20%–70% of RCRs fail by retearing, despite advances in surgical techniques and postoperative rehabilitation.3–5 Even though studies show a significant overall failure rate, satisfaction scores after surgery show significant improvement.6 Failure of repair typically occurs within the first 3 months post-operative, when patients undergo the most intense physical therapy and can represent a failure with continuity.7–10 A failure of repair with continuity occurs in patients with structurally intact repairs that present with persistent weakness and dysfunction that would imply a failed repair, despite imaging that does not demonstrate obvious failure.11-18
When compared to the general population, outcomes in the workers compensation population have often been quoted as inferior.19 Of the twenty-four shoulders of patients who were receiving Workers' Compensation (WC), thirteen (54 per cent) were rated good or excellent, compared with seventy-six (92 per cent) of the eighty-three shoulders of patients who were not receiving Workers' Compensation.20–22 In their series, 58% of WC manual laborers returned to work without limitations compared to 89% of non-WC manual laborers. Workers compensation was created as a no fault system where the employer is relieved of exposure to tort law and the worker gains access to timely and appropriate medical care regardless of fault. Unfortunately, the system often becomes adversarial where access to appropriate care is limited through a process of delay and denial.23 We have previously demonstrated that timely access to appropriate treatment can decrease medical costs and time to Maximum Medical Improvement (MMI) in the working population.24
Most studies that have evaluated outcomes in the workers compensation population have focused on subjective shoulder outcome scores and not functional outcomes. The reasons for lower subjective outcomes in the workers compensation population are multifactorial and not necessarily indicative of a successful outcome in the injured worker. The primary outcome measure to assess a successful result in the workers compensation population is return to work status. One prior study looked at return to work following arthroscopic rotator cuff repair in the workers compensation population.25 They found that 88.5% of the patient’s returned to full duty at a mean of 7.6 months postoperative. They demonstrated that the ability to return to full duty decreased with the patient’s preoperative work level (100% light demand returned to full, 92% medium, 88% heavy and 75% very heavy). Tear size was documented based upon the Cofield definition (43.6% small, 44.9% medium, 11.5% large/massive) and not correlated to final work status.
Factors that affect return to work in the workers compensation population include tear size, patient age, pre and post-operative work requirements, sex, and time to repair. In a retrospective case control study, the mean elapsed time from injury to rotator cuff (RC) repair was 11 weeks with a range of 2 to 25 weeks. Rotator cuff tear (RCT) size had no effect on patient outcome except massive tears repaired after 4 months had the worst outcomes. In general, repairs were not compromised up to 4 months after injury.26 Arthroscopic repair of Full-thickness RCTs (95% were traumatic tears) returned to preinjury level of function in 95% of patients in a group of patients younger than 40 years.27 The result of a retrospective analysis of prospectively collected data on patients presenting with acute RCTs was that early repair resulted in improved outcomes.28 In a case-controlled study of expedited RC surgery in injured workers, the early repaired group of 119 patients was more likely to be working at the final follow up than the control group of 65 patients.29
The purpose of this study was to investigate the outcome of arthroscopic rotator cuff repair in the workers compensation population. This included the patient’s ability to return to work, postoperative strength and clinical outcome scores. Our goal was to determine if rotator cuff tear size, age, time to repair or sex affected our patient’s ability to return to work. This is the largest case series with follow-up that has evaluated return to work in the workers compensation population. It is also the first study to specifically look at tear size based upon area, patient’s age and time to surgery as predictors of outcome and final work status.
This is a Level 3 consecutive Case Series of 69 arthroscopic rotator cuff repairs (ARCRs) that were performed on worker’s comp patients in 2014-2015 by a single fellowship trained orthopedic sports medicine surgeon. Tear size and tear pattern determined repair technique and anchor usage. All repairs were performed arthroscopically utilizing RōG Sports Medicine anchors. The patient population consisted of 48 males and 21 females. Preoperative assessment included strength testing, functional scoring including UCLA scores and diagnostic testing. UCLA scores, ultrasound assessment and strength were recorded at 1, 3, and 6 months postoperative intervals. We continued to follow the patients until Maximum medical improvement (MMI). The RC tear pattern was recorded as the lengths in the anterior-posterior (AP) and medial-lateral (ML) dimensions in centimeters (cm). The two RC tear dimensions were encompassed in a single metric, area=AP*ML in cm2.
At MMI, final work status was recorded. Return-to-work (RTW) status was rated as the ability to perform full, medium/heavy, medium, light-medium, light duty work or none as defined by the Department of Labor Guidelines. One patient was classified as not able to return to work at any level of activity.
Tear size and return to work
Patients were followed with sequential monthly visits until maximum medical improvement was achieved. Patients continued to make improvements out to 6 months postoperative. Improvements in strength measures and UCLA scores were demonstrated as shown in Tables 1 & 2. Both measures improved at 3 months post-OP and demonstrated further improvement at 6 months. Improved outcomes were seen in patients that had tear sizes 3 cm2 or less. There were 5 patients (7.2%) who had a failure of repair which resulted in a decrease in RTW status.
Statistics |
Strength |
Strength |
Strength |
Patient count |
66 |
66 |
69 |
Mean Strength |
4.52 |
4.55 |
4.68 |
Std Deviation |
0.27 |
0.25 |
0.25 |
Minimum |
3.75 |
4.00 |
3.75 |
Maximum |
4.75 |
4.75 |
5.00 |
T-test PV |
0.5089 |
0.003 |
0.003 |
|
Pre-OP vs 3 mo |
Pre-OP vs 6 mo |
3mo vs 6 mo |
Table 1 Statistics of rotator cuff strength at pre-OP and two post-OP times. T-test PV (positive value) comparisons of strength are shown in the lowest row
Statistics |
UCLA score |
UCLA score |
UCLA score |
Patient count |
22 |
30 |
48 |
Mean UCLA score |
13.73 |
18.57 |
21.77 |
Std Deviation |
5.87 |
6.38 |
7.89 |
Minimum |
7 |
2 |
4 |
Maximum |
28 |
30 |
35 |
T-test PV |
0.0074 |
0.0653 |
|
UCLA score |
1 mo vs 3 mo |
3 mo vs 6 mo |
|
Table 2 UCLA scores at three post-OP times. T-test PV values indicate UCLA scores improve on average with increasing post-OP time
The distributions of tear size and patients achieving medium or full RTW status versus those with a lower than medium RTW status is shown in Figure 1. 65.2% of 69 workers achieved RTW status of at least medium level. 73.4% of patients with tear size≤3cm2 achieved work status of ≥medium while 31% with tear size >3 cm2 achieved the same status. 5% of the patients were classified as not being able to return to work under any condition. A two-tailed T-Test of UCLA scores at 6 months after repair indicated that there was a statistically significant difference (PV=0.0001) between workers returning to work and those that were judged less able to RTW based upon rotator cuff tear size, at least at their previous work requirements. Similarly, the t-Test of the difference between Final Strength rating for the two RTW categories had a PV of 0.0001 (Table 3).
Statistics |
≥ medium |
< medium |
Patient count |
46 |
23 |
Average age (yrs) |
49.54 |
54.04 |
Std Deviation |
8.67 |
6.34 |
Minimum |
31 |
38 |
Maximum |
78 |
63 |
Median age (yrs) |
50 |
55 |
Table 3 (A) Average patient age at time of achieving final RTW Status indicating either the ability to perform at least at a medium physical demand level or less than medium physical demand level.
Statistics |
≥ medium RTW status |
<medium RTW status |
Patient count |
46 |
23 |
Average RCT (cm2) |
2.73 |
3.86 |
Std Deviation |
3.58 |
3.88 |
Minimum |
1 |
1 |
Maximum |
20 |
14 |
Median (cm2) |
1.5 |
2.25 |
Table 3 (B) Average rotator cuff tear size for patients achieving final RTW status indicating either the ability to perform at least at a medium physical demand level or less than medium physical demand level
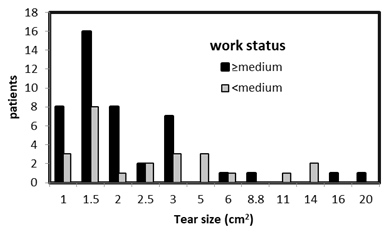
Figure 1 The distribution of patients rated as medium, medium/heavy, and full RTW classification are combined as ≥ medium work status (45 of 69) with 24 workers rated as light/medium or light RTW status (Table 3). One patient was rated as no RTW possibility.
Return to work as a function of age
Tear size increased as a function of increasing age (Figure 2). The linear regression line fit to the data demonstrated a 1.18 cm2 increase every 10 years. There were no massive tears in this population for patients younger than 45 years.
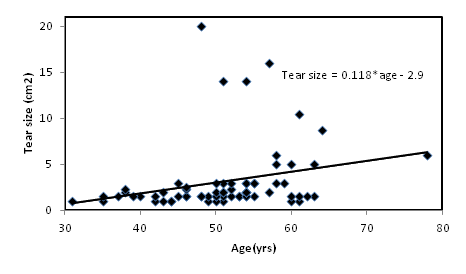
Figure 2 Scatter plot of rotator cuff tear area as a function of age. The solid line is a linear fit of the data delineating the average tear area as a function of age.
The relation of age to RTW status for those rated either ≥medium or <medium is shown in Figure 3. 80% of workers 50 years or younger achieved ≥ medium-RTW status. Workers older than 50 years achieved ≥ medium-RTW status at a 56.4% rate while 43.6% were rated <medium-RTW status.
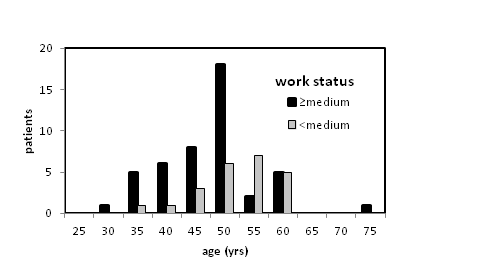
Figure 3 Comparison of the distributions of workers that achieved medium or better RTW status versus those that were rated light or lower RTW status as a function of age. Mean/StDev 47.61/5.09 years for ≥ medium-RTW status (N=46) and 51.96/5.29 years for < medium-RTW status (N=23).
Return to work as a function of surgical delay
An important consideration in RTW is whether the delay to repair is a factor in the eventual ability to perform the required duties. A scatter diagram of work status on a scale of 1=sedentary to 6=full RTW indicates RTW status decreases 0.12 units for every 100-day delay to repair (Figure 4). When the delay to repair period is limited to 400 days, the linear regression line fit indicates there is a 10% decrease in the number of patients achieving a RTW status of ≥medium every 100 days of delay to repair (Figure 5).
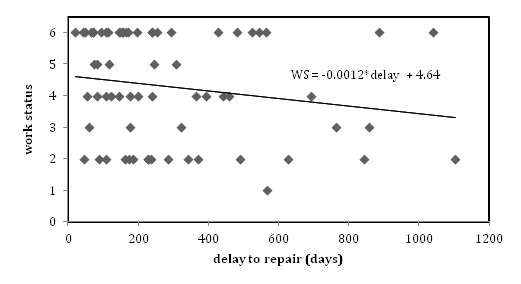
Figure 4 RTW status as a function of time to repair in days from the date of injury where return to full duty = 6, medium/heavy =5, medium = 4, light/medium = 3, light = 2, sedentary = 1. The linear regression line fit to the data has a negative slope of 0.0012 indicating a poorer repair outcome as the time to repair increases.
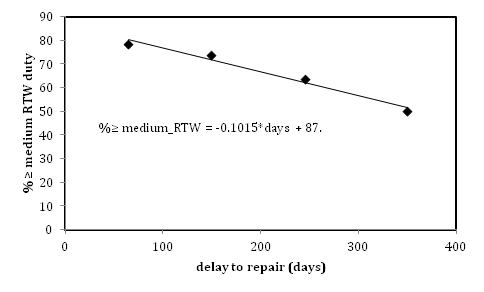
Figure 5 Data in Figure 4 is combined as the per cent of workers that achieve at least medium RTW status in four 100 day periods plotted at the average time to repair in each period. There is a 10% decrease in RTW status of ≥ medium duty with each 100 day delay-to-repair as observed in the slope of the linear-trend line fit of the data.
Return to work and gender
UCLA scores at 1, 3 and 6 months were lower for females. A T-test of the difference of the 6 month values, male/female=22.7/20.3, yielded a two-tailed P value of 0.0043, a statistically significant result. There is little difference between the sexes in the strength measurement except at 3 months where males are stronger and a T-test yields a P-Value of 0.0154, which is statistically significant. Overall it is a minor difference. When RTW status is considered 71% of males (34 of 48) were rated at ≥medium RTW status while 52.0% of females (11 of 21) achieved ≥ medium RTW status. RTW at full duty status was achieved by 44% of males and 29% of females.
Shoulder injuries account for a significant amount of medical expenses and as such causes and preventions have been extensively researched. Many reports have focused on prognostic factors for recovery after ARCR. A systematic review identified 12 significant prognostic factors after selecting 10 studies out of 455 that were reviewed.30 Twelve factors that were found to be significant are: demographic age and gender, clinical (BMD, DM, level of sports activity), preoperative shoulder ROM and obesity, RC integrity (size of lesion, tendon retraction and number of involved tendons, fatty infiltration), other concomitant element involvement. Repair failure rate was between 18 and 29% except for one study that had nearly a 40% failure rate possibly due to a difference in tear size in the study. Another systematic review of RCRs that reduced 662 studies to only 12 found only moderate evidence for increasing age, larger tear size, additional procedures and Workers’ comp to have a negative influence on RCR functional outcomes.31 Another systematic review indicated that baseline scores and a work compensation claim were the most significant predictors of functional outcomes while concluding that it was not possible to reach any definitive conclusion regarding the most relevant predictors of RCR outcomes.32
Based on the numerous systematic reviews of prognostic factors that influence RTW, an ‘umbrella review’ of 56 systematic reviews was conducted.33 Positive factors for RTW were higher education and socioeconomic status, higher efficacy and optimistic expectations of RTW, less severe injury, RTW coordination, and interventions that include the workplace and stakeholders. Negative RTW factors were older age, being female, higher pain or disability, depression, higher work demands, previous sick leave and unemployment, and activity limitations. RTW was shown to be effected by economic, social and job-related factors.34
There has been an ongoing debate as to whether patients with workers’ compensation claims have worse outcomes after RCR. Some studies found no difference in outcomes.35,36 In contrast, the results of a Level I prognostic study indicated that after controlling for confounding factors Patients with Workers’ compensation claims reported worse outcomes.22 However the study had several limitations such as not addressing all the confounding variables, analyzing fatty degeneration or tendon quality, and lower outcome expectations in the workers included in this study relative to another study.37 In another study, 54% of patients receiving Workers’ comp rated their outcomes as good or excellent compared to 92% of patients not receiving WC.19 42% of WC patients returned to full activity while 94% of non WC patients returned to full activity. However, 94% of WC patients were rated having moderate to strenuous activity while 49.4% of non WC patients were so rated. WC recipients had lower recovery for all outcomes when age, smoking and traumatic injury were not considered but when these differences were accounted for there was little difference in outcomes.38 Socioeconomic factors may also have to be addressed in shoulder function studies that conclude WC patients have worse outcomes after RCR.39
We have demonstrated that 65.2% of 69 of patients that underwent an arthroscopic rotator cuff repair from 2014 to 2015 returned to a medium level position or higher. Improved outcomes were demonstrated in patients that had tear sizes 3cm2 or less. This is the first paper that has performed a statistical analysis based upon tear area in relation to final work status. We have also demonstrated lower levels of return with increasing age (40% medium or higher return in age over 50 vs 77.6% return under 50) although tear size was a confounding variable due to the higher tear size association in the age over 50. Female patients also had a lower level average final work status.
In the adversarial environment of workers compensation when treatment is often delayed due to surgery denial, we have demonstrated that this has an adverse effect on final work status outcome. In fact, we found a decrease in 0.12 work status units (Figure 4) for every 100-day delay to repair. This manifested in a 10% decrease in patients achieving a RTW status of >medium every 100 days of delay to repair. Studies have shown that early referral to a specialist with subsequent appropriate surgical management can result in a 10-fold decrease in medical costs and a 60% decrease in time waiting for surgery and time off work. We have previously demonstrated that removal of barriers to care in a subset of injured workers suffering from compressive neuropathies resulted in a decrease in time to MMI from 47 months down to 5.7 months with a cost savings of greater than $200,000.24,40
This was a retrospective consecutive case series utilizing a single surgeon for surgical treatment and follow-up. The surgeon was not blinded during follow-up to the patient’s diagnostic parameters (tear size, age, sex). This same surgeon performed all surgical procedures and follow-up. Our clinic operates as a patient’s choice treatment center. We have no contractual arrangements with employers or insurers that require injured workers to treat with our clinic. Therefore, employer/insurer bias towards final work status outcome was minimized. There was likely a confounding bias relative to tear size and patient age as demonstrated by the fact that tear size was demonstrated to increase with increasing patient age. The final determination of work status was determined by the surgeon accounting for all outcome variables regardless of the patient’s preoperative job description.
This paper focused exclusively on evaluating the outcome of arthroscopic rotator cuff repair in the workers compensation patient to avoid confounding factors. We have demonstrated that there is a high level of return to work in the capacity of medium or higher effort. Outcomes are better in patients with tear sizes ≤3 cm2 and age <50 years. Although the results of rotator cuff repair are often reported as inferior for patients with workers compensation, there is no study that specifically looks at return to work rates or final strength assessment in patients without workers compensation in comparison to patients with workers compensation. This case series demonstrates that good to excellent results can be obtained with appropriate surgical and postoperative management. Most patients can return to work either at moderate to full duty or if employers make the necessary accommodation for individual abilities. Males achieved ≥ medium-RTW status at a higher rate than females: 71% of males (34 of 48) were judged ≥ medium-RTW status while 52% of females (11 of 21) were so classified. Increasing delay to repair reduces the likelihood of returning to a high level of activity. Tear size and age remain the principle factors affecting likelihood of achieving a high level of activity after ARCR.
None.
None.

©2018 Rhode, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.