MOJ
eISSN: 2574-8130


Research Article Volume 4 Issue 1
Professor and Chair, School of Physical Therapy, Anderson University at University Center of Greenville, USA
Correspondence: Martha Hinman, Professor and Chair, School of Physical Therapy, Anderson University at University Center of Greenville, USA 225 S. Pleasantburg Drive, Suite B-3, Greenville,SC 29607, office 8646226086, Tel 8644128896
Received: January 28, 2019 | Published: February 5, 2019
Citation: Hinman M. Validity and reliability of a 10-second foot-tap test in older adults. MOJ Gerontol Ger. 2019;4(1):42-46. DOI: 10.15406/mojgg.2019.04.00175
The purposes of this study were to: (1) compare differences in foot-tap speed between younger and older adults; (2) examine the relationship between foot-tap time and foot-activated reaction time (RT); and (3) assess test-retest reliability of the foot-tap test. Number of Subjects: 115 adults (F=70, M4=5) were recruited from local schools and churches; the sample included 72 young adults (18-64 yo) and 43 older adults (65-92 yo). Subjects with known cognitive, visual, or lower extremity motor deficits were excluded. Methods: After signing an informed consent, subjects were seated at a table where they performed a computerized reaction time test by depressing a foot pedal when a stoplight changed colour. SRTs for 5 trials were averaged for each foot. Subjects then performed the foot-tap test using an electronic tapping device (Western Psychological Services, Los Angeles, CA) which recorded the number of foot taps performed during a 10-sec interval. The subjects’ dominant foot was tested first, followed by a test of the non-dominant foot, and a repeat test of the dominant foot (to assess reliability). A 1-min rest was provided between tests. An independent t-test compared the mean number of foot-taps (on each foot) between age groups, and a paired t-test compared the number of foot-taps between subjects’ dominant and non-dominant feet. A Pearson correlation coefficient was used to analyze the relationship between SRT and number of foot-taps, and an intraclass correlation coefficient (ICC3,1) and Limits of Agreement (LOA) graph were used to assess test-retest reliability. All data were analyzed at the .05 alpha level using SPSS 23 statistical software. Results: The mean number of foot taps differed significantly (p≤.001) between age groups with younger subjects averaging 41.45 (±10.91) taps with the dominant foot and 40.65 (±11.44) taps with the non-dominant foot. Older subjects averaged 28.29 (±10.21) taps with the dominant foot and 26.81 (±11.20) with the non-dominant foot. A mean difference of ≈ 3 taps was found between the dominant and non-dominant feet across all subjects (t=4.616, p≤.001). A moderate, inverse correlation (r=-.451,p=.001) was found between SRT and number of foot taps on the dominant foot. A significant correlation was found between the 2 foot-tap tests performed with the dominant foot (ICC=.793, p≤.001). Conclusions: Younger adults averaged 13 to 14 more foot-taps during the 10-sec test than older adults. Additionally, all subjects demonstrated slightly more foot taps using their dominant foot. Faster reaction times were moderately associated with a higher number of foot taps, and test-retest reliability of the foot-tap test was acceptable. Clinical Relevance: This study demonstrates the moderate effect that normal aging has on foot-tap speed and provides normal values that clinicians may use as a reference when testing individuals with various neurological pathologies. However, the moderate correlation found between reaction time and foot taps suggests that these tests do not necessarily measure the same psychomotor attribute.
When evaluating or screening individuals for functional motor deficits, healthcare professionals need valid and reliable tests to assess sensory perception, joint mobility, muscle strength, and motor coordination. Motor coordination is typically assessed using a variety of timed neurological tests which reflect the speed with which the brain is able to perceive a stimulus, process its meaning, and provide an appropriate motor response. This central processing speed is often referred to as reaction time (RT). RT typically increases as people age, putting them at higher risk for injury when faced with situations that require a split-second response. This deficit accounts for some of the increased incidence of falls and motor vehicle accidents among this segment of the population.1-4 This slowing in RT may be attributed to other age-related changes such as reduced visual fields, impaired cognitive abilities, limited joint mobility, and muscle weakness. In addition, this age group consumes a greater percentage of medications which may also adversely affect RT. A 2008 survey of 3500 older Americans between the ages of 57 and 85 found that 81% used at least 1 prescription medication and 29% used 5 or more.5 In addition, 42% used at least 1 over-the-counter medication and 49% used dietary supplements. Drug use was typically higher among older women and has consistently been linked to higher fall risk among this same age and gender group.6,7
To determine whether an older adult’s RT is sufficient to recover from a loss of balance or respond to sudden changes in driving conditions, we need to assess the speed of foot movements. Previous research has shown decreased finger-tapping ability to be an indicator of decreased motor performance and central nervous system processing speed. Timed finger- and foot-tapping tests have both been used as functional screens for individuals with neurological deficits associated with Parkinson’s disease, stroke, attention deficit hyperactive disorder (ADHD), traumatic brain injury (TBI), epilepsy, and congenital hydrocephalus. Finger-tapping is more widely used and normative values have been established for healthy individuals in different age and gender groups. The Computer Finger Tapping Test (CFTT) is one test of motor speed and coordination which records the number of taps in a 10-second interval. According to the data collected by Christianson and Leathem,8 men tapped at a faster rate than women on the CFTT, and all subjects tapped faster with their dominant hand. Furthermore, they reported that finger-tapping speed was highest in the 25 to 39 age group, then decreased with age, particularly among women over the age of 55.
Although several investigators have studied foot-tapping speed, normative values for this neuromotor test have not been well established in the published literature. Furthermore, little is known about differences in foot-tapping speed associated with age, gender, or foot dominance. In a study conducted by Kent-Braun and Ng,9 foot tapping was used as a measure of voluntary muscle activation during rapid, repetitive dynamic contractions. Foot-tap speeds were compared in young and elderly subjects as well as gender groups. Their results indicated no gender differences; however, a significant slowing in foot-tap speed was noted in the elderly group (34 taps/10 sec. vs. 47 in younger subjects). Similar findings were reported by Gaub et al.10 in their case study of a centenarian. They used a 10-second foot-tap test to measure reaction speed and coordination and concluded that foot-tapping captures some of the slowing that occurs in old age.
Another foot-tapping study conducted on children focused on variations in tapping performance between the dominant and non-dominant feet.11 Although these investigators found no significant differences between the dominant and non-dominant feet of young subjects, Peters12,13 reported superior right-footed performance among healthy adults. This preference was thought to be associated with environmental influences such as driving an automobile. Molnar et al.14 reported using the foot-tap test as part of a physical examination to test a person’s fitness to drive a motor vehicle. However, without a range of normal values for adults, the validity of using the foot-tap test to predict an individual’s ability to safely operate a motor vehicle may be questionable.
Although previous studies suggest a decline in foot-tapping speed as people age, further research is needed to document normal foot-tap values within age groups and to verify the relationship between this test and other measures of neuromotor speed and coordination. Thus, the purposes of this study were to: (1) establish normative data for younger vs. older adults; (2) determine whether foot-tap times differed based on foot dominance; (3) assess the test-retest reliability of a 10-second foot-tap test; and (4) determine the nature of the relationship between the timed foot-tap test and a foot-activated, computerized RT test.
A cross-sectional research design was used to gather descriptive data to define normal values for a 10-second foot-tap test by age and foot dominance. This study was approved by the University Research Review Committee at Hardin-Simmons University in Abilene, Texas.
Sample
Adults over the age of 18 were recruited from a university campus, two churches, and two retirement facilities in the local community. All subjects signed an informed consent and completed a brief medical history questionnaire to determine whether they had any pre-existing conditions that would interfere with the test procedures of the 135 volunteers, 115 subjects (70 women and 45 men) met the study criteria and completed all test procedures; 20 subjects were excluded due to conditions that interfered with testing (i.e., physical or communicative) or because they changed their mind and did not wish to complete all test procedures (Figure 1). For data analysis purposes, subjects were sub-divided into a “younger adult” group (n=72) of subjects under the age of 65 and an “older adult” group (n=43) for those aged 65 and older.
Test procedures
Foot dominance was first determined by asking subjects which foot they would use to kick a ball. Next, an online reaction time test was used to assess each subject’s RT.15 The test was downloaded onto a laptop computer which was used for every data collection procedure. Because foot-tap speed was the main focus of this study, a foot pedal (Pedalpax SA1, Cincinatti, OH) was used in place of a handheld computer mouse to operate the reaction timer. Subjects were seated in front of the computer screen with their knees in approximately 90 degrees of flexion and their dominant foot resting on the foot pedal (Figure 2). RT was recorded as the time (in seconds) required for each subject to perceive a change in traffic signal color from red to green and respond by depressing the pedal. Each subject was given 2 or 3 practice trials before performing 5 consecutive recorded trials. The average of these 5 trials was recorded on each subject’s data form. The RT test was then repeated using the non-dominant foot.
The foot-tap test was administered after the RT test. Subjects were again seated in a chair with knees flexed approximately 90 degrees and feet resting on the floor. An electronic tapping device (Western Psychological Services, Los Angeles, CA) was positioned under one foot, and the subject was instructed to tap as many times as possible until told to stop (Figure 3). The timer recorded the number of foot taps over a 10-second time period. The subject performed one practice trial with the dominant foot before performing the recorded trials on the non-dominant and dominant foot, with a one-minute rest between trials.
Data analysis
Descriptive statistics and independent t-tests were used to establish and compare normative data for the RT and foot-tap test between the 2 age groups. A paired t-test was then used to compare the number of foot-taps between subjects’ dominant and non-dominant feet. Test-retest reliability of the foot-tap test was examined using data from the practice and recorded trials on the dominant foot; an interclass correlation coefficient (ICC3,1) and limits of agreement (LOA) graph were used to analyze this relationship. Finally, the relationship between the subjects’ RT and number of foot-taps was analyzed using a one-tailed Pearson correlation coefficient to establish concurrent validity for the foot-tap test. All data were analyzed at the .05 alpha level using SPSS 23 statistical software.
A significant difference was found between the number of foot taps recorded for younger and older adults in both the dominant (t=6.324, p<.001) and non-dominant foot (t=6.408, p<.001). For subjects in the young age group (18-64 years), the average number of foot taps was 41.45±10.91 with the dominant foot and 40.65± 11.44 with the non-dominant foot. Older subjects (65-92 years) averaged 28.29±10.21 taps with their dominant foot and 26.81±11.20 taps with their non-dominant foot, a difference of 13 to 14 taps (Figure 4). A similar age-related difference was found in the reaction time of older subjects demonstrating an average of 0.17 seconds slower with both feet. A significant difference was also found between the number of foot taps recorded with the dominant and non-dominant foot (t=4.616, p<.001) across all subjects. In this analysis, subjects averaged approximately 3 taps more with their dominant foot.
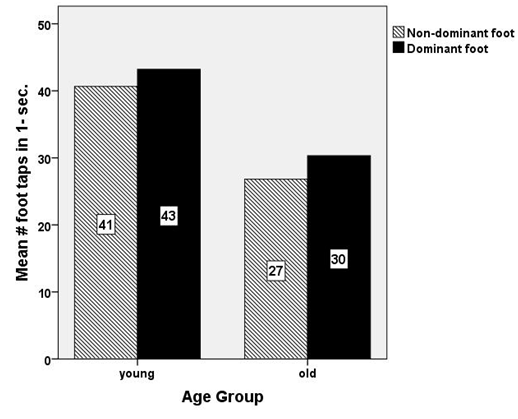
Figure 4 Comparison of number of foot-taps performed with the non-dominant and dominant foot of young and old subject.
Results of the reliability analysis for the foot-tap test suggest a moderately high correlation between the practice trial and recorded trial with the dominant foot (ICC=.793, p<.001). The LOA analysis also suggests good reliability between these two trials. In all but 5 subjects, the difference between trials fell within 2 standard deviations of the mean difference of the 2 foot-tap tests (Figure 5).
When assessing the concurrent validity of the foot-tap test, a significant, moderate correlation was found between the average RT and number of foot taps recorded with the dominant foot (r =-.451, p< .001). RTs and foot-taps were inversely related in that faster reaction times (i.e., fewer seconds) correlated with a higher number of foot taps (Figure 6). However, the coefficient of determination (r2) indicates that the number of foot taps only accounts for 20% of the variance in subjects’ RT.
Although statistically significant, the correlation between RT and foot taps was not high enough to suggest clinical relevance. The coefficient of determination (r2) for the analysis of the relationship between number foot-taps and reaction time was only 20%. Therefore, 80% of the variance in reaction time was accounted for by other factors not measured in this study. Thus, in a clinical setting, the foot-tap test would not be a reasonable substitute for measuring an individual’s RT. There are several possibilities as to why the correlation between foot-taps and RT was not stronger. One of the possible factors associated with these results may be the significant levels of fatigue experienced by many subjects during the foot-tap test. Decreasing the number of repetitions of the foot-tap test or providing longer rest periods may have allowed subjects to perform more foot-taps in the 10-second period.
Our results did find a significant age-associated decline in the number of foot-taps which was consistent with the findings of previous studies. For example, Aoki and Fukuoka16 found that older individuals, averaging 69 years of age, had significantly longer intervals between taps compared to younger individuals. This would result in a decreased number of taps performed within a given time period as demonstrated in our study. In a similar study of finger-tap speed, Christianson and Leathem8 also reported a significant performance decline among individuals over the age of 55.
Our data analysis revealed a slight difference in number of foot-taps performed with the dominant versus non-dominant foot, given that all subjects averaged about 3 more taps when using their dominant foot. This finding differs from those reported by Gabbard and Hart11 in a similar study performed with pediatric subjects. Perhaps the influence of functional use across a longer lifespan may account for more pronounced differences seen in older adults compared to children.
There was limited prior evidence regarding the test-retest reliability of the foot-tap test, and our results demonstrated a moderately high reliability for this test. Nevertheless, further research is needed to better support the clinical relevance of the test before using it as a clinical tool for assessing the speed of a motor response. The sensitivity of the foot pedal used to measure the reaction time and foot-tap test may have affected the accuracy of the recorded measurements in both the RT and foot-taps tests. For example, unless the subject fully depressed the pedal in the RT test, it did not record the movement. In addition, if the subject did not lift his or her foot completely off the pedal between taps, the next tap was not recorded. Although some trials were repeated when these errors were noticed by the subject or the evaluator, it may still have resulted in some inaccurate measurements.
Several other limitations in the study design that may have influenced the results. For example, subjects who reported prior ankle surgeries, sprains, or sensory deficits were not excluded. Thus, it is possible that some of these conditions, particularly sensory deficits, could have affected the subjects’ tapping abilities. However, older adults have some type of biomechanical and/or sensory impairments in their ankles and feet, so this sample was representative of the older population. In addition, other investigators Aoki and Fukuoka16 previously reported that decreased tactile sensitivity was unrelated to finger-tapping performance in the older subjects who participated in their study. A second limitation was the lack of a controlled environment during the data collection. Subject history, reaction time, and foot-tap tests were all performed within close proximity at each testing location. Thus, distractions or competition among subjects could have influenced some of the test results. Many subjects also had decreased dorsiflexion range-of-motion associated with tight heel cords. This required a minor adjustment (10 degrees or less) in the knee angle used by some subjects during the foot tap test. The comparison of foot-taps and RT between male and female subjects was not a major focus of this study. Nevertheless, a comparison of gender groups revealed that the men in our study typically had faster RTs and a greater number of foot taps than the women. The mean difference in RT was approximately 0.1 second and the mean difference in foot taps was approximately 6 taps.
In conclusion, the results of this study do support an age-related decline in motor response time with a moderately high degree of test reliability. Because the performance of functional motor tasks such as walking, stair-climbing, and driving are dependent upon the ability to elicit a quick response with one’s feet, this information is useful in assessing the ability of older adults to safely perform these motor tasks and avoid potential injuries.
The author would like to acknowledge the following individuals who assisted with the data collection for this study: Shannon Higgins, Cassie Sandifer, Haylee Sherwood, and Emily Wren.
No conflict of interest has been declared by the author.

©2019 Hinman. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.