MOJ
eISSN: 2574-8130


Research Article Volume 6 Issue 4
1epartment of Medicine for the Older Person, London Northwest University Healthcare NHS Trust, Watford Road, Harrow, HAI 3UJ, UK
2City College of Acupuncture, London, N1 6AH, UK
Correspondence: Eddy Chua, London Northwest University Healthcare, Northwick Park Hospital, England, United Kingdom
Received: November 13, 2021 | Published: December 1, 2021
Citation: Chua P, Kolli V, Devanson R, et al. The impact of COVID-19 on the rapid response team: short term assessment rehabilitation and reablement service (STARRS) in England. MOJ Gero & Geri Med. 2021;6(4):107-112. DOI: 10.15406/mojgg.2021.06.00277
Background: Rapid Response Services have become commonplace in the assessment and management of the older person at home. However, since the arrival of COVID-19, there have been scarce data regarding how the global pandemic has affected the efficacy and modality of such services.
Aim: We examined data from referrals to the Rapid Response Team (STARRS) during the first and second wave of the COVID-19 pandemic in England over the course of one year. We then compared to this to data from the previous year. Weexamined the mode of consultations before referral, hospital avoidance and hospital readmission after 28 days post-discharge.
Results: There was a significant 30% reduction in referrals from A&Ewith increase in GP and LAS referrals such that overall, there was no statistically significant difference in total referral rates. Hospital avoidance and hospital admission at 28 days post-discharge remained unchanged. The most dramatic change was a significant increase in telephone consultations in place of face-to-face consultation before referral to STARRS.
Conclusion: An increase in telephone consultations before being triaged to STARRS is likely to be the new norm; as such STARRS must adapt to ensure governanceon service deliveranceis maintained
The UK currently has a population of 66 million and, consistent with other European countries, will continue to have an increasing ageing population.1 In 2018, there were nearly 12 million people aged >65-years-old, of whom over 5 million were aged >75, 1.6 million were aged >85, 0.5 million were aged >90 and nearly 15,000 were centenarians. The last figure has been predicted to increase to over 21 000 by 2030,1 by which point one in five people in the UK (21.8%) will be aged >65 with similar increases across all elderly demographics.1 The >85 age group is the fastest growing; it is set to double to 3.2 million by mid-2041, and to 5 million by 2066 which is predicted to be approximately 7% of the UK population.1
To support England’s ageing population and those with complex needs, NHS 10 Year Long Term was formulated (August 2019 england.ltp@nhs.net). In Chapter 1: ‘A new service model for the 21st century’, it proposes to:
The Brent Rapid Response Team, STARRS, is staffed by a multi-disciplinary team which includes nurses, physicians, healthcare assistants, physiotherapists and occupational therapists. It is based in Northwick Park and the Central Middlesex hospital with services that operate from 08:00 to 22:00, 7 days a week. There is access to diagnostics including imaging and access to ambulatory care services. Geriatricians are also able to access other clinical specialists acutely in hospital when advice is needed with the option of immediate admission to the hospital if patients deteriorate. STARRS consultants are also able to review some patients in Hot Clinics with trainees from the London deanery.
Furthermore, STARRS has a role in improving patient flow through A&E and supporting the frailty service. Once patients are identified in A&E as suitable for STARRS input, they are discharged to the STARRS assessment area to avoiding breaches in A&E waiting time targets where assessments and treatments can subsequently be completed.
Patient care is coordinated by virtual ward rounds led by a senior member of the team in the morning and a consultant in the afternoon. Webcasting technology facilitates meetings across hospital sites. Out of hours medical support between 17:00 to 22:00 and during weekends 08:00 to 22:00 was provided by six geriatricians. On average, there are approximately 60 patients who are discussed during this virtual session every day. During the virtual ward rounds, the multidisciplinary team discusses patient management, discharge and escalation. Patients are visited daily, up to twice a day, by the team and a driver also helps facilitate patient transfers; STARRS employs its own driver which enables patients to be brought to and from hospital with relative ease. Clinical governance of patients is shared between GPs and geriatricians. Previous analysis over a five-year period supports this model of care, suggesting that it may avoid hospital admissions in addition to being cost effective2 However, we are not aware of any literature on how COVID-19 has impacted the ability of a Rapid Response Service to support the older person at home.
Initial coronavirus cases in the UK were first reported in late January 2020, and by the end of March the same year 4426 people in the UK had died within 28 days of testing positive with COVID-19. In England, the first lockdown began on 23 March 2020. Non-essential high street businesses, schools and indoor sports venues were closed; people were advised to work from home where possible, to avoid public transport and to practice social distancing. The first concessions in this strict lockdown were made in May 2020 and further relaxed throughout the summer. However, by early November, national restrictions had to be reintroduced in England, initially using a three-tier system. This was changed to a four-tier system in December due to concerns of rising cases attributed to a new variant of the virus. By early January 2021, national restrictions were again reintroduced. The rules during this lockdown were very similar to the first lockdown. By early March, there was a phased exit out of lockdown.3
We analysed data obtained from the Key Performing Indices (KPI) for STARRS. For each year, the KPI starts from April and includes up until March the following year. However, as COVID-19 became prevalent starting in March 2020, data were used from the period of March 2020 to February 2021. We then compared this data to the KPI over a similar time for the previous year, during which we looked at the referral numbers, mode of triage before referral (face-to-face or telephone consultation), length of stay on the virtual wards, hospital admissions whilst under STARRS and hospital readmission 28 days post-discharge from STARRS. For sub-analysis, we separated referrals into categories: General Practitioners (GP), London Ambulance Service (LAS), Accident and Emergencies (A&E) and others. The category labelled ‘others’ consisted of referrals from a number of specialties which included Infectious Diseases for intravenous antibiotics, anticoagulation clinics to manage labile international normalized ratios (INR), community rehabilitation teams including the Intermediate Integrated Home Care team for closer symptom management or treatment with medications such as intravenous antibiotics or diuretics. The student t-test and the chi square were utilised for statistical comparisons.
Due to increasing numbers of GP referrals over the last four consecutive years, response time for the current year was recorded differently. In previous years, the response time was recorded from the time a referral was accepted to the time patients were seen. GPs were now asked at the time of referral if patients needed to be seen within 2 hours or 4 hours. This was to prioritise referrals. As such, the response time may not be directly comparable to previous years. During the first wave of the pandemic, STARRS supported the Anticoagulation clinic at Northwick Park Hospital for 5 months (March to July 2021). In total, 827 patients had their INR taken by STARRS. As these patients were undertaken by STARRS as a one off due to exceptional circumstances surrounding the first wave (STARRS only accept patients with labile INR) these patients were removed from analysis.
Patient demographics, response times, length of stay in the virtual, hospital avoidance admission (HAA) and hospital admission after 28 days
From March 2019 to Feb 2021, 9,639 patients were seen by STARRS. The ratio of females to males was similar at 3:2 (female age from 22 to 107 years and male age between 21 to 104 years). Over 99% of patients were aged 65 years and above. The mean length of stay in the virtual ward also remained the same at less than 5 days as in the previous year.
Response times
Due to changes in recording of this as described above, for the period between March 2020 to Feb 2021 98% of the referrals were seen with four hours as opposed to 83% in the previous year.
GP referrals
GP referrals were reduced initially in the first 2 months (March and April) during the first wave; however, there was no specific trend during the second wave. Overall, there was no significant increase in the number of accepted GP referrals when compared to the previous year Figure 1a.
A and E referrals
A and E referrals were dramatically reduced, especially in the first wave, and continued to do so but to a lesser extend during the second wave. As a result, overall, referrals from A and E were significantly reduced by greater than 30% when compared to the previous year prior to the pandemic Figure 1b.
London ambulance service referrals
LAS referral, by contrast, showed no significant changes during the first wave. Although there was a slight increase in accepted referrals in the second wave with an overall increase by 22% in the study periods, this did not constitute a significant statistical difference (Figure 1c).
Referrals from others
It would appear that referrals had increased mainly during the first wave;these were patients for INR management. However, these patients did not have labile INR before referral. STARRS only undertook this to support the anticoagulation clinic and as suchwhen this figure (827 patients) was removed, there was a non-statistical increase of 8% compared to the previous year. (Figure 1d).
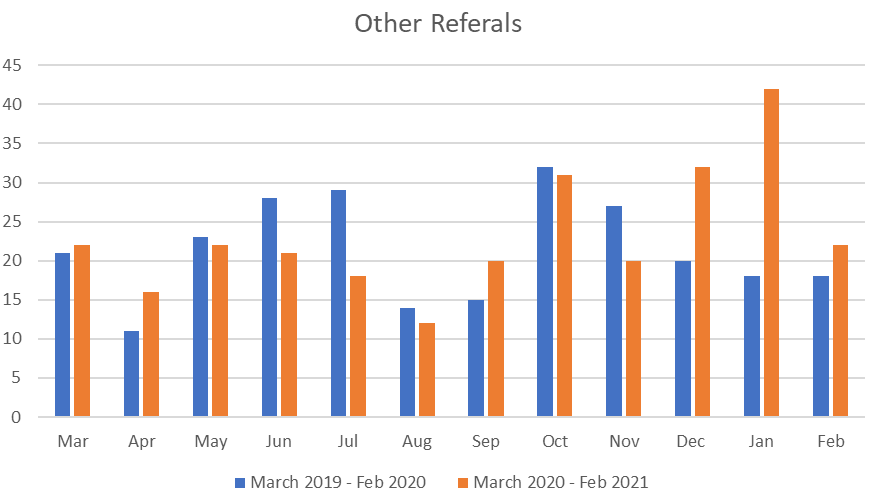
Figure 1d Referral from others besides GP/A&E and LAS mean Total number of referrals 256 Vs 278t-test, p=0.55.
Overall, the total number of accepted referrals were similar compared to the previous year at 4797 and 4842. HAA also remained unchanged at 85% versus 83% as was Hospital admission within 28 days after discharge from STARRS (8 and 7% respectively Table 1a).
|
Source |
March 2019-Feb 2020 |
March 2020-Feb 2021 |
|
GP |
2978/3623 (82) |
3163/3720 (85) |
|
A&E |
641/739 (87) |
466/511 (91) |
|
LAS |
173/224 (77) |
226/288 (78) |
|
Others |
219/256 (86) |
245/278 (88) |
|
Total Hospital Avoided Admissions |
4011/4842 (83) [a] |
4100/4797 (85) [b] |
|
Total Hospital Admissions within 28days after discharged from STARRS |
281/4011 (7) [c] |
328/4100 (8) [d] |
Table 1a Hospital Avoided Admissions and Hospital Admissions with 28 days after discharged from STARRS, percentages in parenthesis, [a vs b and c vs d , chi square, p= not significant]
Triage of patients after consultations (Face to face Vs telephone triages)
Table 1c shows how patients are triaged to STARRS after consultations. Over the lastfour successive years, the number of face-to-face contacts before referrals had been steadily declining. The onset of the COVID pandemic, however, precipitated a sharper decline in this trend to just over 1% of consultations.
Satisfaction of service
Satisfaction of the service remained high during COVID. During the pandemic there were 2 complaints and no serious incidents compared to 9 complaints over the previous four years.
COVID-19 has caused significant change in many aspects of life and the Rapid Response Service is no exception to this. In England, the first and second wave of the pandemic occurred between the months of March to May 2020 and from October 2020 to February 2021.
Overall, the number of referrals were not significantly different compared to the similar time period of the previous year; there were, however, a number of differences on sub-analysis. GP referrals were initially reduced in the months of March and April but thereafter were not affected by the second wave. As such, the number of referrals from GP increased by nearly 100 patients (2.6%) yet was still not statistically significant. During the first wave, testing capacity for COVID-19 was limited in the UK; in our hospital, this was limited to 50 tests a day. There were also limited supplies of personal protective equipment (PPE), both of which impeded the Rapid Response Team’s ability to see referrals from patients at home. These factors became less restrictive during the second wave. Patients have, however, grown more reluctant to attend hospitals which may also account for the observed slight increase in GP referrals in the second wave.
A very striking feature were the referrals from A&E, especially during the first wave, such that by the end of the study period A&E referrals were reduced by more than 30%. Patients became reluctant to attend hospitals, especially during the first wave of the pandemic. As such, hospital attendees had reduced such that in our local hospitals, very significant numbers of hospital beds remained unoccupied. With the initiation of the COVID-19 vaccination programme in December 2020, this phenomenon continued to be observed during the second wave, although to a lesser extent. However, it has also previously been noted that there has been a steady decline in A&E referrals over successive years.2 It is very likely that another contributory factor is responsible; the increasing frailty in a sub-group of patientswith a greater tendency to relapse soon after discharge from hospital or from A and E.
LAS referrals showed no significant differences in trend during the first and second wave. The limitations on testing and PPE may account for the slight decrease in referrals noted during the first wave. However, in the latter half of the second wave (December 2020 to Feb 2021), a trend of increasing referrals from the LAS was noted such that the total number of referrals over the study period had increased by 64 patients (22%), although this was not noted to be statistically significant. This is largest number of referrals to STARRS over the past 5 years (Table 1b). This was less likely to be related to COVID-19 but changes in service specification. From October 2020, STARRS, in line with all Rapid Service Services in the North-West London Sector, agreed to accept referrals directly from the central LAScentral Hub after a telephone consultation. This may explain the increasing referrals from LAS over the last 3 consecutive months.
|
Time |
No of patients |
|
March 2020 to Feb 2021 |
288 |
|
March 2019 to Feb 2020 |
224 |
|
March 2018 to Feb 2019 |
250 |
|
March 2017 to Feb 2018 |
249 |
|
March 2016 to Feb 2017 |
220 |
Table 1b London Ambulance Service referrals over the past five consecutive years
The ‘others’ group referrals from a number of disciplines including the anticoagulation clinics where patients with labile INRs are monitored, administration of intravenous antibiotics, palliative care services and community rehabilitation teams. During the first wave, STARRS supported patients at home who were unable to attend anticoagulation clinics. However, after excludingthese patients with stable INR, there was increase in the number of referrals by 8% which was not a statistically significant rise.
The most striking change between the years is the mode of consultation used before triaging patients to STARRS.Almost overnight, here was a fall by nearly 20% in the rate of face-to-face consultations in favour of telephone consultations. However, the decline in face-to-face consultations for telephone consultations preceded COVID19, fallingover the last 3 consecutive years (Table 1c) and subsequently to just over 1%in the immediate aftermath of the pandemic in March 2020. At the time of writing, this figure has now risen to about 5% being telephone consultations followed by triaging to STARRS.
|
Time |
Type of consultations |
|
March 2020 to Feb 2021 |
T 4749 (99) |
|
F2F 48 (1) |
|
|
March 2019 to Feb 2020 |
T 3922 (81) |
|
F2F 920 (19) |
|
|
March 2018 to Feb 2019 |
T 3712 (78) |
|
F2F 1047 (22) |
|
|
March 2017 to Feb 2018 |
T 2787 (64) |
|
F2F 1569 (36) |
Table 1c GP referrals and triaged to STARRS after telephone consultations (T) and face to face consultations (F2F) over the last four consecutive years; percentages in parenthesis
The ESTEEM trial examined the effect of telephone triages for the management of same day consultationrequests in 42 GP practices in four centres in the United Kingdom.4 This was a large study where patients were randomised to telephone triage delivered by a GP, a nurse orusual care groupwith5,000 patients in each group. The number of subsequent contacts with GP practices, A&E attendances within 28 days and cost were evaluated. Overall, the results were quite favourable as telephone triage interventions were associated with reduced workloads for GPs, no greater A&E attendances and no increased costs. The only significant negative finding noted was that there were more subsequent patient contacts after telephone triage over the next 28 days. GP telephone triage was associated with a 33% increase and nurse telephone triage was associated with a 48% increase in the mean number of contacts per patient over 28 days). This might be attributable to a decrease in patient confidence or satisfaction in their management plan. It was noted that nurse triage sported the lowest patient satisfaction rate and the highest level of further primary care contact. A final deficiency with the ESTEEM trial’s applicability to the Rapid Response Service was that, amongst the study population, only just over 10% in each of the groups were >75 years old.
A concern that this shift towards telephone consultations by GPsbefore Rapid Response Service triage is that telephone consultations may be more challenging for the demographic serviced by STARRS. Consultations with older patients areoften more time consuming as they tend to have several co-morbidities, a greater likelihood of cognitive and hearing impairment. As such, the history may often come from a second party caller (e.g.,spouse) or worse a third-party caller (e.g., a relative some distance away fromatient). It is therefore significantly more difficult to fully appreciate the extent of the patient’s symptoms via the telephone.
Furthermore, the frail older patient is more likely to present with an altered clinical presentation or atypical presentation. An example would be worsening heart failure presenting with non-specific symptoms such as increasing confusion, poor intake or decline in mobility. Alternatively, the frail older person with acute coronary syndrome may presentwith non-specific symptomssuch as worseningconfusion and poor intake without the typical features of central crushing chest pain. Atypical presentation is common in the frail older patient.
In a retrospective observational study in the Netherlands of 355 patients (aged >80,mean age of 86)who presented to anA&E department, atypical presentation was noted in 188 which constituted 53% of the study’s population5 A similar study by Limpawattana et al.found the rate of atypical presentation to be approximately a third of the study group.6 The Dutch study found that in theatypical presentation cohort, the most frequent diagnoses werefractures, neurological conditions and infections. In 99% of the atypical presentations, patients had a geriatric syndrome namely frailty, sarcopenia, cognitive impairment and anorexia of ageing.7 This is not a new entity but merely new terminology. This was first coined by Bernard Isaacs over 50 years ago, the “geriatric giants” which encompasses immobility, instability, incontinence and impaired cognition.8
Atypical disease presentation was also noted to be more common in the frail older person (59%) than in non-frail older%).9 Patients with an atypical presentation were more likely to have a longer stay in hospital, less likely to be discharged back to their own home,5 a longer diagnostic process, higher rates of misdiagnosis which delays treatment and a poorer clinical outcome.10-15
A small comparative study (n=106) on quality, safety of telephone versus face-to-face consultation concluded that the former was more convenient with good satisfaction rates from patients and doctors. However,there were significant concerns about patient safety compared to face-to-face consultations. Telephone consultation may be more suited for follow-up and management of long-term conditions rather than for acute management.16 Video consultations (VC) on the other hand may be more suitedfor single pathologies.Infrastructure issues will need addressing before this can become mainstreamed use in primary care.17,18
Since frailty and atypical presentation are very closely linked, Rapid Response Teams need to have mechanisms in place to meet this. Some of these are already in place in STARRS and include regular training and upskilling of the team, mortality meetings and constant review of the lessons that can belearnt. Furthermore,senior members of the team vet GP and LAS hub referrals and when necessary, challenge theappropriateness of the referrals.
The Rapid Response Service should not be perceived as an emergency service unlike LAS. In future, STARRS will needmore sessions in hot clinics to enable medical review of patients. There is also a need for audits on patient outcomes from hospital admissions whilst under the care of Rapid Response Team as we are not aware of any significant body of literature on this.19 This is important for several reasons, a low threshold for hospital admission may result ininappropriate attendances to the A&E buta higher threshold for hospital admission may result in prolonged hospital stay or even greater mortality due to delayed clinical diagnosis.
The length of stay in the Rapid Response Services is around 5 days. We are seeing increasing numbers of patients being referred soon after discharge. Future research should be directed to look at the efficacy of alternate models of carefor this group of patients and for patients who are regular users of hospital services. An example is the Integrated Care Pathway Team. This operates in a similar way tothe Response Team model but with less intensity, visiting patients up to 3 times a week but with the ability to support patients for up to six weeks.2
In conclusion, the total number of referrals, hospital avoidance, hospital admission were not affected by COVID-19, A&E referrals however, were significantly decreased and the modality of consultations shifted even further in favour of telephone consultations over face-to-face consultation. The effect on the former may be transient but the increase in telephone consultations prior to referral may be the new norm. Rapid Response Teams will need to rise to meet this challenge to ensure that management of the frail older person is not compromised.
The authors would like to acknowledge Shunshun Wang, University of Manchester for her constructive comments in the manuscript.
None.

©2021 Chua, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.