MOJ
eISSN: 2574-8130


Mini Review Volume 5 Issue 1
1Student, Faculty of Medicine, Federal University of Jequitinhonha and Mucuri Valleys, Brazil
2Medical Clinic Resident, Faculty of Medicine, Federal University of Jequitinhonha and Mucuri Valleys, Brazil
3Professor, Faculty of Medicine, Federal University of Jequitinhonha and Mucuri Valleys, Brazil
4Palliative Care Team, Santa Casa de Caridade, Brazil
Correspondence: Bruno Bastos Godoi, Faculty of Medicine, Palliative Care Team, Federal University of Jequitinhonha’s` Valley and Mucuri, Santa Casa de Caridade, Diamantina/MG, Brazil, Tel +55(31)986862511
Received: December 13, 2019 | Published: February 6, 2020
Citation: Godoi BB, Freitas LVB, Chaves AA, et al. Palliative care and public health an issue to be held. MOJ Gerontol Ger. 2020;5(1):23?25. DOI: 10.15406/mojgg.2020.05.00224
Palliative Care (PC) is underdeveloped in most parts of the world. PC is based on knowledge inherent to the various specialties, possibilities of clinical and therapeutic intervention in the various areas of medical science knowledge and specific knowledge. The practice of PC should be adapted to each country or region according to relevant aspects such as availability of material and human resources, type of existing health planning, cultural and social aspects of the population served. PC has received very little attention in the field of public health. The probable reasons are that public health’s primary focuses are to prevent illness and premature deaths, and public health professionals may also believe that end-of-life issues are a health system problem rather than a priority to be addressed through population health efforts. With the rapidly aging world population and the associated increase of multiple ‘‘noncommunicable’’ diseases, the need for palliative care will increase dramatically over the next 50 years. Although palliative care services may start in one or more health care organizations that will become centers of PC excellence, it is always important to keep in mind the vision that the process to implement palliative care within a country is striving to integrate palliative care into all levels of the society from the community level upward and from the palliative care expert in the health care system downward. Given this, the creation of Palliative Care teams should be among the priorities of managers, due to the demographic transition and the high demand for palliative care due to the growth of morbidities secondary to chronic degenerative diseases.
Keywords: palliative care, public health, hospices, hospice care
The need for palliative care (PC) has never been greater and is increasing at a rapid pace due to the aging world population and rising cancer and other noncommunicable diseases.1,2 Despite this need, PC is underdeveloped in most parts of the world. PC is expanding in the developed world, despite the myths and misunderstanding about its nature and purpose, but it is just beginning to be available in the developing world, where it is most needed.3–8
Another concept to overcome is the patient who is “out of therapeutic possibilities”. There is always a therapy to be recommended for a patient. In the advanced stage of a disease and with little chance of cure, physical symptoms are factors of discomfort. For these there are procedures, medicines and approaches that can provide physical well-being until the end of life. This therapy cannot be denied to the patient.9–11
The path of adequate information, the formation of competent professional teams, the reaffirmation of the principles of PC and the demonstration of positive results of this treatment modality, is the best way to overcome remaining barriers to the implementation of a PC policy. 9–11
PC is based on knowledge inherent to the various specialties, possibilities of clinical and therapeutic intervention in the various areas of medical science knowledge and specific knowledge. World Health Organization (WHO) in 1986 published principles governing the work of the multidisciplinary PC team. These principles were reaffirmed in their review in 2002: promote pain relief and unpleasant symptoms; not accelerate or prorogate death; integrate psychological and spiritual aspects in patient care; offer support systems that enable the patient to live as actively as possible until the moment of death; provide support system to assist family members during the patient's illness and to cope with grief; multiprofessional approach to addressing the needs of patients and their families, including bereavement follow-up; improve the quality of life and positively influence the course of the disease; should be started as early as possible, along with other life-prolonging measures such as chemotherapy and radiotherapy, and include all necessary investigations to better understand and control stressful clinical situations.10,12–15
The practice of PC should be adapted to each country or region according to relevant aspects such as availability of material and human resources, type of existing health planning, cultural and social aspects of the population served. This should be done according to the scope of PC presented in Figure 1.10,14,16
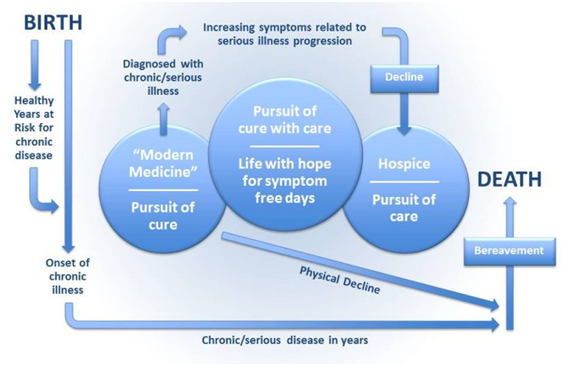
Figure 1 Scope of palliative care.9
When talking about active, progressive and life-threatening disease, it means that PC can and should be indicated in the presence of chronic diseases in different stages of evolution. There is the possibility that death by natural evolution of a process of falling ill can be postponed for years. It is not possible to apply the principles of palliative care only in the case when there is a sudden death due to illness, accident or violence.17–19
The increased survival has also generated a considerable number of Intensive Care Unit (ICU) patients and, consequently, a greater experience of the health professional in the terminality process. Thus, in order to individualize the care provided and organize care in highly complex environments, palliative care is adopted, which uses advanced communication skills in an attempt to alleviate pain, psychological and spiritual suffering.16,20
The use of care protocols in the care of patients under the final conditions of life is extremely important, since it makes health care systematized.
PC has received very little attention in the field of public health worldwide. The reasons are that the primary focus of public health is to prevent any kind of disease or premature death.9–11,13,14,20,21
“End-of-life issues have a huge impact on the dying person’s family”.17 We estimate that in 2030 there will be more than 74 million deaths per year and the majority of this deaths linked to chronic diseases.17,20,21
Globally we have more than 400,000 PC workers, over 1.2 million volunteers, and over 9 million people acting as palliative caregivers. This means that over 10.5 million people are involved with delivering hospice and PC every year.20
WHO has formulated some approaches that can facilitate the PC at public health in order to help more patients who need this kind of care:11,16,20
The need for palliative care
Globally, there is a significant need for PC and its development. At least 60% of people dying will have a prolonged illness and dying older, necessitating from a service of PC.11,13,16,20
With the rapidly aging world population (demographic transition) and the associated increase of multiple ‘‘noncommunicable’’ diseases, the need for palliative care will increase dramatically over the next 50 years: 11,13,16,20
Palliative care for all
It is relevant to say that the process of implementing an excellence PC center is needed to be achieved through integration into all levels of the society from the community level upward and from the palliative care expert in the health care system downward. Despite this, it is imperative to develop a PC system linked to the existing health care system and social support network. “It will be critical for all palliative care experts to spend 40% - 50% of their time educating and supporting other health care professionals and community support systems” (Figure 2).10–13,16,17,22–25

Figure 2 Palliative care for all.16
Palliative Care is an issue that should be solved and delivered for patients who need this kind of assistance. There are several of challenges for effective Palliative Care, such as: a lack of understanding about palliative care in the community; limited funding and under-resourced status; stringent national policies related to increasing availability of some pain control drugs necessary for palliative care, and lack of trained human resources.
Given this, the creation of Palliative Care teams should be among the priorities of managers, due to the demographic transition and the high demand for palliative care caused by the growth of morbidities secondary to chronic degenerative diseases.
None.
None.
The authors declare no conflict of interest.

©2020 Godoi, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.