MOJ
eISSN: 2574-8130


Research Article Volume 9 Issue 3
1Graduate Program in Human Development and Technologies, Institute of Biosciences, Paulista State University- UNESP, Brazil
2Department of Physical Therapy and Occupational Therapy, Paulista State University- UNESP, Brazil
Correspondence: Marcos Eduardo Scheicher, Department of Physical Therapy and Occupational Therapy, Paulista State University- UNESP, Marília, São Paulo, Brazil
Received: August 01, 2024 | Published: August 22, 2024
Citation: Cruz TGCD, Nascimento LMD, Silva JFDLE, et al. Effect of frailty, activity of daily living, instrumental activity of daily living and age on cognition of community-dwelling elderly people: a cross-sectional study. MOJ Gerontol Ger. 2024;9(3):41‒44. DOI: 10.15406/mojgg.2024.09.00326
Ageing is the main indicator of cognitive impairment and can affect activities of daily living (ADLs), instrumental activities of daily living (IADLs) and frailty. The objective of this study was to verify the interference of IADLs, ADLs, frailty status and age on the cognition of community-dwelling elderly people. Were used the follow tools: Montreal Cognitive Assessment (MoCa); Edmonton Frail Scale (EFS); Lawton scale and Barthel scale. All subjects included were community residents, aged 60 and over, both sexes. To evaluate the effect of age group and frailty status on cognition was used ANCOVA with Bonferroni post-test. Correlations were made using the Pearson test. Values of p <0.05 were accepted as significant. A relationship was observed between all independent variables and cognition (p <0.0001) and was observed an effect of age and frailty on cognition (p <0.001). There is an association between frailty, age, IADL and ADL with the cognition, and were found that the age group and frailty status interfere on cognitive impairment.
Keywords: aging; cognitive dysfunction; frailty; functional status
The debate on human aging and demographic transition has become increasingly consolidated, as the phenomenon has become a global trend that has gained strength in both developed and developing countries.1 T It is estimated that in 2050, two billion people will be over 60 years old in the world.2 Human aging is caused by an accumulation of changes at the cellular and molecular level that degrade systemic functioning, resulting in a greater risk of developing various diseases.3 Studies have shown that, like other chronic pathologies, aging is the main indicator for cognitive impairment and the development of related dementias,4,5 and even those who do not have a diagnosis of dementia can also develop cognitive decline and neurological changes with advancing age.6
Cognition is defined as a process of awareness of the body and everything that surrounds it, encompassing the following functions: attention, language, task execution, organization, and information processing.7 Cognitive changes can be divided into mild impairments, when the individual presents some cognitive disorder, but without it interfering with executive functions, and with a slight loss of independence to perform more complex tasks, and severe impairments, whose symptoms can lead to the diagnosis of dementia and the inability to maintain normal cognitive performance, leading to functional impairment that significantly interferes with day-to-day life.8,9
Cognitive impairments can interfere with activities of daily living (ADLs) and instrumental activities of daily living (IADLs) and vice versa. ADLs are the most basic and necessary activities for the person's physical maintenance, such as: dressing, performing personal hygiene, walking, eating, etc., and IADLs include more complex tasks such as managing finances, carrying out shopping, social communication, managing medications, etc.10 The decrease in the ability to carry out these essential life activities can lead to insecurity, reduced quality of life and a state of dependence on other people.11
Another situation associated with aging and with growing interest in scientific circles is the frailty syndrome, defined by Fried et al as a multidimensional syndrome with five components: weight loss, exhaustion, low level of physical activity, muscle weakness and slow gait speed.12 Studies show that, despite not being directly part of the five components described by Fried, frailty and cognitive deficit can be related as distinct entities, but with a pertinent occurrence in the same elderly person.13,14 Considering the importance of the subject, the objective of this study was to verify the interference of IADLs, ADLs, frailty status and age on the cognition of community-dwelling elderly people and propose possibilities for maintaining skills and cognition.
Was a cross-sectional study with a convenience sample of 163 individuals aged 60 or over, living in the catchment area of the two Family Health Units (USFs in the Portuguese acronym) of the city of Marília, São Paulo, Brazil. The Ethics Committee of the Faculty of Philosophy and Sciences, Unesp, Marília, approved the study (Approval number 4.168.934). Inclusion criteria: aged 60 years or over, both sexes, resident of the area covered by the USFs. Exclusion criteria: not signing the Free and Informed Consent Form, after agreeing to participate in the research.
A search of individuals aged 60 years or over who were registered with the USFs was performed through the e-SUS Primary Care digital platform.
Next, the assessment was scheduled in two ways:
1) The older adults were contacted by telephone and invited to come to the USF to participate in the study;
2) Community agents of the USFs visited the homes of the older adults and performed the assessments on those who agreed to participate.
Cognition
The Montreal Cognitive Assessment (MoCA) was used to assess the cognition of the participants. The total possible score of the test is 30 points and normal scores depend on the level of education (illiterate: ≥ 12; 1 to 4 years of study: ≥17; 5 to 11 years of study: ≥20; ≥ 12 years of study: ≥ 26).9
Level of dependency
ADLs and IADLs were assessed using the Barthel index and Lawton scale, respectively. The Barthel index assesses the ability to eat, dress, transfer, control sphincter and perform personal hygiene.15 The Lawton scale assesses the ability to perform more complex tasks to achieve a more independent life in the community, such as: ability to use the telephone/cell phone, use public transport, prepare meals, manage medications, manage finances, tidying the house and doing housework.16
Frailty
To assess frailty, the Edmonton Frail Scale (EFS) was used. This tool consists of the assessment of nine domains (cognition, general health status, functional independence, social support, medication use, nutrition, mood, functional performance, and urinary continence).17
Data were assessed for normality using the Shapiro-Wilk test and for homogeneity using the Levene test. To evaluate the effect of age group and frailty status on cognition (adjusted by education level) was used ANCOVA with Bonferroni post-test. Correlations were made using the Pearson test, with cognition as the dependent variable and frailty, age, IADLs and ADLs as independent variables. Given a significant correlation, a linear regression was performed to determine R2. The analyzes were carried out using SPSS 22.0 software and values of p < 0.05 were accepted as significant.
Were evaluated 163 elderly people, 94 women (72.30 ± 7.65 years old) and 69 men (72.28 ± 7.11 years old), with a total average age of 72.22 ± 7.60 years old. Figure 1 shows the correlations and linear regressions between the variables evaluated. Correlations were observed between all variables, with emphasis on frailty and IADLs.
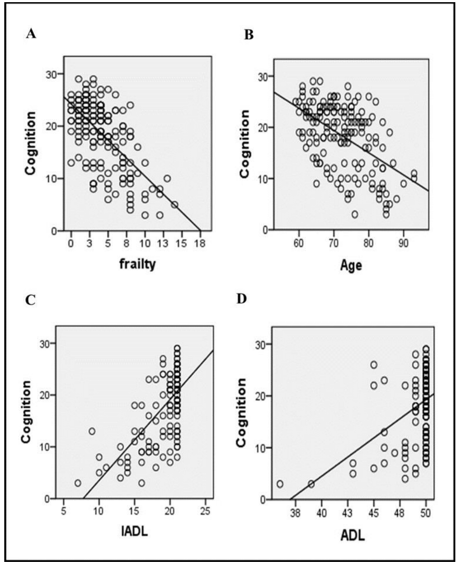
Figure 1 A) Correlation between frailty and cognition, r = -0.634, p < 0.0001; R2 = 0.402; B) Correlation between age and cognition, r =0.520, p <0.0001; R2 = 0.27; C) Correlation between IADL and cognition, r =0.663, p <0.0001; R2 =0.44; D) Correlation between ADL and cognition, r = 0.422, p <0.0001; R2 = 0.18.
An effect of age group [F (1.0,160) = 14.37; p < 0.001] and frailty status [F(1.0.160) = 40.49; p < 0.001] was observed on cognition in the evaluated sample. Figure 2 shows comparisons of cognition between age groups and between frailty statuses after the post-hoc test.
This study investigated the relationship of variables such as frailty, IADL, ADL and age on cognition.
Originally, cognitive status was not considered in the initial description of the frailty phenotype described by Fried 12, but it has gained notoriety for its ability to predict cognitive changes.18 Because of this, a term called “cognitive frailty” was created, characterized by physical frailty and cognitive changes not explained by Alzheimer's disease or another type of dementia.19
The results of the study pointed in the same direction: the frailty status interferes with cognition. In this sense, several longitudinal,20-22 and cross-sectional studies,23,24 have also demonstrated that higher levels of frailty are associated with cognitive decline. In reality, it can be said that there is a two-way relationship, as shown in Figure 3.
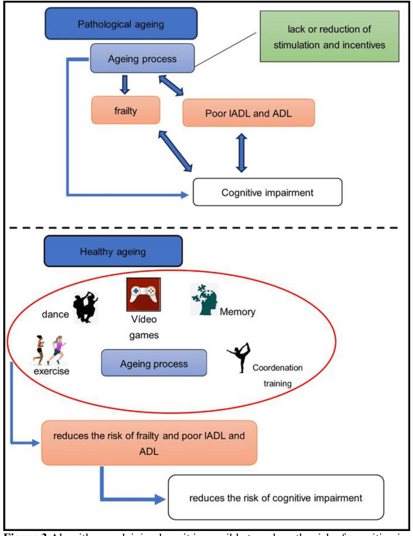
Figure 3 Algorithm explaining how it is possible to reduce the risk of cognitive impairments. IADL: instrumental activities of daily living. ADL: activities of daily living. All figures have creative commons licenses.
Frailty conditions is associated with adverse outcomes such as reduced mobility and physical capacity, increased risk of dependence and mortality.25 These conditions can contribute and accelerate cognitive impairment.26,27 In relation to this topic, as important as showing the relationship between frailty and cognition is suggesting actions to prevent the occurrence of frailty and, consequently, reduce the chance of elderly people developing cognitive decline associated with frailty. One way would be to screen frailty in the elderly in primary care, dividing them into greater or lesser risk of developing frailty syndrome and promoting necessary actions to prevent it.
In addition to the increase in numbers, it was also observed that the elderly have been living longer, bringing consequences such as changes in the central nervous system and changes in cognition. As described above in relation to frailty, in addition to highlighting this association, it is important to develop strategies to change this trajectory. Knowing that there is an association between age and cognition and that older elderly people may show greater declines, could carrying out activities earlier reduce this decline? The literature points out that when a person is involved in several activities, the chance of maintaining the health of the central nervous system is greater.28
Studies have shown that targeted interventions are effective in improving performance immediately after training in the trained tasks.29–31 Why not offer activities in primary health care aimed at promoting healthy ageing of the central nervous system, such as dance, video games, memory training, coordination training, social interactions, aerobic exercise, for example?28
IADL and ADL are very important for healthy aging, as they allow the elderly to maintain their autonomy and independence.32,33 Our results showed that the higher the IADLs and ADLs, the better the cognitive capacity. The literature indicates that the difficulty to successfully complete ADLs related to cognitive impairment can be understood as a cognitive-functional hardship.34 As with fragility, there is also a two-way relationship here. Do IADL and ADL interfere with cognition or does cognition interfere with IADL and ADL?
As described above, it is necessary to screen deficiencies in these two aspects and act in the short, medium, and long term, focusing decisions on the elderly, according to their needs. This form of approach is a fundamental component of health care,35 and can indicate individuals who are already sick or in the process of becoming ill, guiding the health team to make individualized decisions.
Figure 3 explains how it is possible to develop healthy aging and reduce the possibility of cognitive impairment related to frailty, IADLs and ADLs.
The results showed that there are association between frailty, age, IADL and ADL with the cognition. Besides, were found that the age group and frailty status interfere on cognitive impairment.
The authors would like to thank all the participants.
The authors declare no conflicts of interest of any nature.

©2024 Cruz, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.