MOJ
eISSN: 2574-8130


Research Article Volume 3 Issue 4
1Department of Medical rheumatologist CNS PAISE, Bolivia
2Department of Regional Chief of Epidemiology CNS, Bolivia 3Department of Resident Family Medicine CNS, Bolivia
Correspondence: Amadeo Armando Rojas Armata, Regional Chief of Epidemiology CNS, Bolivia
Received: April 28, 2018 | Published: August 8, 2018
Citation: Callahuara BAI, Armata AAR, Pacheco DVS. Efficacy of the clinical activity of rheumatoid arthritis using the scales DAS28 and HAQ-20 in relation to the BAIC semiological maneuver. MOJ Gerontol Ger. 2018;3(4):317-334 DOI: 10.15406/mojgg.2018.03.00140
DAS28 and HAQ-20 are widely used in clinical research to quantify the activity and evolution in patients with rheumatoid arthritis (RA). In this study, a new semiological maneuver is proposed to evaluate patients. Objective: To determine the degree of effectiveness of the BAIC maneuver in relation to DAS28 and HAQ-20 in the clinical activity of the disease evaluated by the physician.
Material and methods: A prospective, cross-sectional, descriptive study was carried out. 240 RA patients attended in the PAISE N° 32 from August to October were included. In the consultation, the doctor and the patient independently performed the registration of painful swollen joints, subsequently the HAQ-20 was used to evaluate the physical function self-perceived by the patient during common activities in his daily life also the DAS28 evaluating the number of joints affected in each stage of the patient with RA, to later relate to the BAIC Maneuver.
Results: With the DAS28 scale: Inactive 12.5%, Mild Activity 29.6%, Moderate Activity 46.7% and High Activity 11.2%. With the HAQ-20: No difficulty 13.3%, with low difficulty 29.2%, with moderate difficulty 47.1% and cannot do it 10.4%. With the BAIC it was obtained: Mild 42.5%, moderate 45.9% and severe 11.6%. Conclusion: The present study analyzes the clinical value of the DAS28, HAQ-20 scales, in relation to the BAIC maneuver, which helps us evaluate the muscle strength of RA patients. The relationship between the scales and BAIC's semiological maneuver is closely related
Keywords: DAS28, HAQ-20, rheumatoid arthritis
Rheumatoid arthritis (RA) is an inflammatory, systemic, autoimmune, chronic disease of unknown etiology; its main white organ is the synovial membrane; it is characterized by polyarticular and symmetric inflammation of small and large joints, with possible systemic commitment at any time of its evolution. Which compromises the different joint structures, peri-articular and tendinous preferentially the synovial membrane.1
In general it involves large and small joints in association with systemic manifestations such as morning stiffness, fatigue, weight loss. When it involves other organs, the morbidity and severity of the maladies are greater, being also an important cause of premature mortality. This has important social repercussions causing work incapacity increase of direct costs for attention and indirect costs for loss of productivity and subsidies.1.2
As a systemic disease it is very variable in its presentation and in its evolution. Initially produces synovial lesion, presenting a symptomatic complex of an inflammatory type that is responsible for the clinical manifestations, however, occasionally the recognition of rheumatoid arthritis in its initial stages can be difficult due mainly to its different forms of onset. Rheumatoid arthritis can destroy hyaline cartilage cause bone degeneration severe dysfunctions, limited movement and disability.3,4
The first evaluation of a patient with rheumatoid arthritis should include: clinical history (investigate family and personal history of disease rheumatic, comorbid, previous treatments) complete physical examination and request for complete blood count, transaminases, profile Lipids and urinalysis.
In the patient with confirmed diagnosis, it should be investigate signs and symptoms of inflammation joint (activity), functional status, structural damage (radiological lesions) and presence of extra joint manifestations. The differential diagnosis of a patient with polyarthritis includes: infectious causes, other connective tissue diseases (systemic lupus erythematosus, Sjögren's syndrome, overlap, among others). Reactive arthritis, paraneoplastic, etc. The first contact physician must investigate and exclude other diseases that cause polyarthritis, through a clinical history and adequate physical examination, supported by studies of complementary laboratory. The rheumatologist is responsible for controlling the inflammatory process and must monitor the comorbidity associated with the disease.
The factors of poor prognosis in early rheumatoid arthritis are: positive rheumatoid factor, female sex, hopmozigosidad for subtypes of shared epitope (HLA DR 0401,0404), high inflammatory activity equal or greater than two large articulations , commitment of hand joints, time of evolution of arthritis at the beginning of the treatment≥3 months, early detection of radiological erosions, high degrees of disability, presence of extra-joint manifestations, low socioeconomic level and the presence of other antibodies.
Secondary amyloidosis should be suspected in patients with rheumatoid arthritis who develop proteinuria, renal failure, gastrointestinal symptoms, cardiomyopathy and/or hepatomegaly, and in those in which there is a high level of acute phase reactants with little clinical activity. The chronic anemia that accompanies rheumatoid arthritis generally does not require treatment.
Oral iron supplements are not indicated, except in those cases in which the coexistence of a ferropenic component is demonstrated as a cause of the anemia it is recommended to periodically perform biometrics complete blood count to assess the degree of anemia. Cardiovascular disease in patients with rheumatoid arthritis increases the risk of morbidity and mortality. Rheumatoid arthritis is an independent factor of cardiovascular risk. The inflammation Persistent is an additional risk factor. Rheumatoid arthritis patients present with accelerated atherosclerosis, which leads to a increased risk of cardiovascular morbidity and mortality. In women with RA, there is three times more risk of presenting myocardial infarction.
It is recommended to identify the factors of cardiovascular risk: age, male sex, high activity of the disease, smoking, hypertension, dyslipidemia and history of myocardial infarction. Cardiac involvement due to rheumatoid arthritis will be suspected due to the appearance of pain pericardial, heart failure or alterations of driving. Pericarditis will initially be treated with non-steroidal anti-inflammatory drugs (NSAIDs) at full doses, in case of inefficiency, prednisone (dose of 1 mg/kg/ day) in rare cases of tamponade cardiac will perform pericardiocentesis.
Myocarditis will require, in addition to the treatment of heart failure, use of prednisone at high doses. Pulmonary disease should be suspected in the presence of pleuritic pain, dyspnoea, progressive as of recent onset or hemoptysis. In case of pleural involvement it is recommended to perform thoracentesis to obtain an exudate. investigate other pathologies such as infection or neoplasia. The pleural affection should be treated with NSAIDs at full doses or prednisone at medium doses (10 to 20). mg/day).
Acute interstitial lung disease is treated with prednisone (1-1.5 mg/kg/day). If there is not response can be treated with cyclophosphamide or azathioprine Bronchiolitis obliterans with organized pneumonia is treated with prednisone (1.5 mg/kg/day). The treatment of Felty Syndrome (splenomegaly, leukopenia<3.5000/mm3 and neutropenia<2,000/mm3) infrequent extra joint manifestation, requires exhaustive control of the inflammatory activity of rheumatoid arthritis. As specific measure, the use of of granulocyte-stimulating factor when the absolute neutrophil count is less than 1,000/mm3 and the patient has a history of associated serious infections. Extreme precautions should be taken to prevent infections in patients with arthritis rheumatoid among other measures it is recommended to apply the usual vaccines, but never with Attenuated microorganisms if under immunosuppressive treatment. The patient with rheumatoid arthritis must maintain a scrupulous dental hygiene. At the beginning of the diagnosis of rheumatoid arthritis, recommends doing an analysis of the main Risk factors for fracture and loss of mass bone, in the presence of some of them will indicate bone densitometry. The first-line treatment options for osteoporosis are alendronate and risedronate. Hormone treatment is not indicated. Osteoporosis should be suspected in patients>65 years of age, with a history of fragility fracture, Body mass index<19, smoking, estrogen deficiency, active rheumatoid arthritis, HAQ>1.25 and treatment with glucocorticoids at a dose≥7.5 mg/day for 3 months. A high percentage of vertebral fractures are asymptomatic, so it is recommended to perform lateral x-ray of the dorsal and lumbar spine evaluate the existence of fracture or deformity vertebra l.
The manifestations are extraarticular of the AR have the importance of being prognostic markers of an entity that in itself reduces the life expectancy entire 3 and 20 years NDO increases in patients with seropositive disease, begins early, extensive and active; all this is us announcing the importance of extra-articular manifestations that we are going to describe based on your relationship with the pathogenesis of the disease They are classified progressively in, first group with manifestations related to pathogenesis that occurs at synovial level, a second group in relationship with immune hyperstimulation the third group of entities that are particularities of the same AR or associations with other well-defined entities such as the Sjögren's syndrome, and the last, that corresponds to the complications due to immunosuppression or persistent inflammatory activity. All we do this with didactic purposes, since reality is complex and, for example, osteoporosis or anemia is partly they must to the same basic mechanisms of injury of the others are iatrogenic disease and the treatment s used in disease control:1
The first group of Extra-articular manifestations (MEA) correspond to the extra-articular expression of the same process that is observed in the synovium, that is, it would be an extension out of the articulations of what happens pathogenically in the rheumatoid synovitis. Lymphadenopathy is the lymphoid organs side that have been activated by the process immune-inflammatory joint and extra-articular. Anemia is the multifactorial expression of the inflammatory process in which iatrogenic factors are added (gastropathy due to nonsteroidal anti-inflammatory drugs [NSAIDs]) and various deficits that we will comment later Felty's syndrome could consider more a form of clinic extraarticular that of an entity independent of the RA. The Complications are a consequence of the disease or of iatrogenia to the drugs used in the control of RA.
Pathogenesis of extra-articular manifestations
When the biopsy is performed an inflamed organ or tissue, outside the scope synovial, in the patient with A R are several lesions: G ranulomas, vasculitis and chronic inflammatory infiltrates that sometimes adopt the follicle morphology lymphoids that form autoantibodies as the factor rheumatoid. Rheumatoid nodules are granulomas that contribute to one of the seven criteria of the AR established in 1987 by the American College of Rheumatology (ACR) and is one of the most MEAs frequent These nodules are granulomas with an area central with fibrinoid necrosis surrounded by a palisade epithelioid cells and fibroblasts, and outside a crown of mononuclear inflammatory cells. For some, the nodule is a form of vasculitis and for others it is about a response of cellular hypersensitivity.
Vasculitis is another way very heterogeneous pathology of MEA in patients with A R that manifest themselves in the skin, the eyes, in the system nervous and various internal organs. Usually associated with AR-seropositive forms with elevated circulating immunocytes and sometimes with cryoglobulinemia and hypocomplementemia, which supports the pathogenesis through immunocomplexes with activation of the complement system. We must not forget other possibilities of immunocomplexes due to antibodies different from the rheumatoid factor as is the case of antibodies antinuclear antibodies, anti-endothelial autoantibodies, antibodies antifilarin to name a few, and also antibodies neutrophil anticytoplasm (ANCA), which can activate inflammatory cells that release oxyradicals toxic and protease or activate cytotoxicity. In the vasculitis there is a genetic predisposition as sam ple of the association of this disease with HLA-DR4, and we must not forget the role of cytokines and adhesins, that have an undoubted role in vessel vasculitis small and medium.
There are many other manifestations that the pathologist describes as inflammatory infiltrates with cellular diversity, with exudates and with fibrosis in different proportions, and this in diverse locations such as serous, pulmonary interstitium, myocardium and other organs target to which the immune response is directed towards exogenous antigens or self - antigens that the guest loses the toler ancia . Mention also that the T lymphocytes and mostly the CD4 cells protagonists that induce other immune cells and inflammatory sometimes forming true follicles Lymphoid which can give a local immune response conformation, at least in part, of self - antibodies mentioned.
The extra-articular triad of nodules-vasculitis-serositis is usually detected in regions subject to physical stress such as synovitis in mobile areas (diarthrodiales the nodules in places of friction and hyperpressure, vasculitis in places of bifurcation or more pressure and serositis pleuropericardial in areas of friction). Is also evident that the paralysis of limbs makes disappear the inflammatory activity of the joints corresponding and mechanisms of ischemia-reperfusion mediated by oxiradicals and nitric oxide (NO). Hormone factors show unconformity, since RA synovitis predominates in women 2-4 times more than in men and MEAs, on the contrary, they predominate in man. There are also no correlations between synovitis and the MEAs of the AR.1–4
Manifestations extra-articular clinics
We will start with the manifestations related to the pathogenesis of synovitis, although later we do not detect correlations between both. These manifestations usually appear in active forms and at the beginning of the disease; On the contrary, complications tend to be late, in chronic and active arthritis, while the manifestations of the triad may occur before, during or after the synovitis. (nodules-vasculitis-serositis).
Nodules rheumatoid
They are granulomatous structures which are expressed as nodules of millimeters up to more than 5 cm, located in areas of friction, high pressure or friction, hence its Greater frequency in the extension face of the forearms (olecranon); tend to be firm oval masses, often Multiple and painless, with typical histological pattern . These nodules can be on the surfaces (elbows, knees, scapulae, spine, sacrum, scalp or ankles) and with less often we see them deep (intradermal, tendinous or viscera). Intraderms are usually be on the back of the fingers of the hand, coincide with vasculitis clinic and when the hand is left at rest they can disappear. Tendinous nodules are usually be located in flexor tendons of the hands and those of visceral localization are mostly detected in the lung, in pleuropericardial serous, myocardium, dura mater and choroid, or in the intestine, which we will review later. In number they can be unique or multiple and are usually asymptomatic, but sometimes necrosan or over they infect Rheumatoid nodules often coincide with other systemic manifestations, with the presence of rheumatoid factor and not necessarily with the inflammatory synovial activity, and may even precede the Arthritis Treatment with methotrexate may increase your number at the time that can match reduction of the synovitis. In weeks they disappear and can recur in clusters of nodules.
A rheumatoid nodule is not pathognomonic and we must rule out other pathologies like lipomas, tophi or similar nodules of other rheumatic diseases. The pathogenesis of nodules was discussed and the mechanisms are recognized traumatic factor and the immunological one, either through the reactions of humoral hypersensitivity immunocomplexes, or the delayed or cellular.1–5
It is the first of the specific extra-articular manifestations described in the patients with RA. Its broad spectrum is determined by the the calisa and type of affected vessel , and sometimes local benign deformities are treated at the periungual level and, at other times, a Severe systemic necrotizing vasculitis such as pancreas-crustitis (PAN) that can be fatal. Post-mortem studies show an incidence of 25% but they are rare manifestations, with an incidence of 1 per 100,000 population. They usually occur in patients with seropositive arthritis, aggressive, evolved, with systemic manifestations, but they can appear in patients without active synovitis as well as the nodules, which for many authors are of origin vasculitic It has the same frequency in men as in women. The course is episodic and relapsing with significant morbidity, mortality at 5 years is 50% and the prognosis is worse when they have alterations neurological Patients with vasculitis systemic diseases present weight loss, fever and leukocytosis and, rarely, leukopenia. To level dermal, the lesions go from single plates or several grouped brown at periungual level or on pads; in others we observe subungual hemorrhages, rash or ulcers deep abrupt onset that can be superinfected. They appear in unusual places in venous pathology and It is rare that they suffer from gangrene.
At the systemic level, there are ocular manifestations (scleritis, retinal vasculitis or keratitis). In the nervous system, the most important findings frequent are the monkey multiple neuritis, which they carry worse prognosis but may have alterations in the Central Nervous System.
In lung and heart we can detect several alterations, from the alveolitis, serositis pulmonary arterial hypertension, and infarction of myocardium or aortitis with arrhythmias. At the kidney level there may be vasculitis in one in five, and one in four with kidney failure and frequently with alterations of the sediment. In the digestive tract there are in one of five patients with vasculitis hepatosplenomegaly and infrequently abdomen acute.
The pathology of vasculitis depends on the size of the vessel with involvement of medium-small-caliber muscle arteries with fibrinoid intimal necrosis, lymphocyte infiltrates and polymorphonuclear in the adventitia with segmental lesions of different stages. In the clinic they are expressed at the level dermal, nervous system and other viscera, similar to the bread. There are other forms that correspond to vasculitis leukocytoclastic arterioles or venules in skin and other tissues. Endarteritis with proliferation of intima and thrombosis is usually seen at the level of the vessels small ones in digital arteritis and we should remember that can appear superimposed forms with other vasculitis or it is only venous and capillary lesions with hands cold and sweaty with palmar erythema.
In its pathogenesis, the path of Type III hypersensitivity is supported by the auto - antibodies such as high rheumatoid factor, antibodies antifilarin, antinuclear, others that attached to the antigen they form circulating immunocomplexes and sometimes hypocomplementemia. Other times we will detect antibodies against components cytoplasmic neutrophil like lactoferrin, which gives ANCAp positive. Anti-C1q IgA antibodies are Associated with vasculitis. It also describes the vasculitis associated with alleles HLA-DRB104, the same thing seen in patients with Felty syndrome who often attend with vasculitis. In the last two decades, the study of the endothelium reveals what it was to think and not is but the mechanism of recruitment and activation of circulating cells (leukocytes, platelets). Two groups of mediators of inflammation, cytokines and adhesins have entered with great force in this field explaining the Why and how leukocytes and platelets are activated, migrate and perform their function at the level of phlogogenic focus. Various cytokines (necrosis factor) tumor [TNF ], interleukin-1 [IL-1], cytokines such as IL-8) activate to the endothelium and leukocytes that start the approach first transient by means of selectins (select L in leukocytes, and P and E in endothelium) that interact with polysaccharides (sialil-Lew-x and others), and then with two others groups of adhesins: integrins and the family of immunoglobulins (ICAM-1,2,3 and VCAM-1) interact with intense binding of leucos or platelets to the endothelium and cytokines, and these adhesins allow transmigration to the place of inflammation. In this field, adhesins and constituents extracellular (fibronectin, laminana, collagen and others) adhere and that's how those cells stay migrants, who play their role, which in principle is defensive nature Leukocytosis, very useful in PAN to assess the activity of vasculitis, in these AR forms are not seen, hence their value is low. C-reactive protein (CRP) is not useful except for assess synovitis. Factor VIII, the complement and the factor Rheumatoid and circulating immunocomplexes have more value. TO Next, we review the extra-articular manifestations with an intimate relationship with the pathogenesis of RA and what we will do by the location in the various organs, starting with heart and lung with serositis, that with the vasculitis and nodules makes up the triad of the intrinsic manifestations of RA.1,2
Cardiopulmonary alterations often occupy the second place after the hematological manifestations that we will discuss more late. In the respiratory tract we differentiate two large zones:
These two zones, the interstitium pulmonary and pleural serosa can be altered clinically and above all subclinically. The driving zone has a series of exocrine glands and can be altered due to high frequency of association of the syndrome Sjögren secondary with the RA, what we should keep in mind in interpreting the various findings. The AR as a disease systemic autoimmune affects the lung as well as other viscera, but with poor clinical expression due, on the one hand, to that the alterations are in their mostly mild and our organs have a large reserve capacity, hence they are detected in studies with methodology of great sensitivity or by taking samples or highly sensitive biopsies and only 5% -10% of the patients with RA show extra-articular alterations outside the anemia and nodules. Anyway, the presence of these alterations, and especially the clinics, worsen the prognosis of the AR, hence its importance.6
The lung contains many vessels and connective tissue, that's why interstitial alterations they are to be expected and if they are not more important it is for the effectiveness of the tract defense systems respiratory. Table 1 shows the different methods available to us in the study of pulmonary disease in patients with different pathology. The first three methods (clinical history, exploration, analytical and radiology) are obligated, but have low sensitivity and specificity practically nil. The other six methods we can subclassify them in the nothing bloody (functional tests, computerized axial tomography [CT] high resolution and scans) and washing, and transbronchial biopsies, and especially the transparietal pulmonary They are not exempt from morbidity and even mortality l late, although the direct biopsy study is the most specific of all the methods and they all have high sensitivity. Currently, the TAC has great value to focus where to do the washing or the biopsy, since these pathologies are focal. Using these methods, a great frequency of alterations is observed lungs and the contradictions that were there for the decade of the sixties, in which the existence of Ellman's "rheumatoid lung". This author defended it based on the postmortem studies, in which they detected frequent alterations in serous and interstitial, by the similarity with the pathological findings of synovitis the absence of other connectivity that explains it and the absence of cause’s exogenous.7
Methods |
Sensitivity |
Specificity |
Clinic |
Low |
Null |
Radiology |
Low |
Null |
Analytics |
Low |
Null |
Pulmonary death tests |
high |
Null |
Pulmonary gammagraphy with 67 Ga |
high |
Null |
High resolution pulmonary CT |
high |
high |
Bronchoalveolar lavage |
high |
high |
Biopsy transbronchial |
Moderate |
high |
Biopsy pulmonary |
Very high |
Very high |
Table 1 Methods of study of the pleuropulmonary pathology in arthritis rheumatoid
TAC, computed axial tomography
The first three methods they are obligated, but sensitivity is low and specificity null, hence other methods such as lung function tests and high CT resolution, which have high sensitivity, and also the Pulmonary CT scans the lesion where it can then be perform the bronco wash alveolar and, if necessary, the biopsy pulmonary. If the latter is necessary, it must already be possible the pulmonary will be made and not the transbronchial, because the sample does not go from 1 to 2 mm, so it is usually insufficient to make a correct opinion, and the transparietal biopsy directed by CT gives us in 95% of patients a method much more acceptable. Biopsy is a technique easy to carry out, but it is not exempt from morbidity and even mortality, hence it is chosen when is considered necessary and thinking that his repetition has the same problems. Therefore, the way forward is to carry out a good history and clinical exploration followed by simple radiology and general analytical; to then it is logical to choose some tests functional lungs that will tell us if it is a alteration of the ways or is a restrictive process, and above all it will show us the severity of the process for indicate a TAC that locates the same, it tells us if it is of routes or from another location can tell us if it's about an active inflammatory process, also the extent and severity; and if we look for the diagnosis it will go to the biopsy. In case of pathology interstitial, if we want to go to treatment it can be useful to do the bronchial wash.
Before entering the classification of the various manifestations pleuropulmonary should always make a memory of other etiological possibilities such as:
In Table 2 you can see the various pleuropulmonary forms in RA and it is common to see combined forms. The first five they are relatively frequent manifestations and the rest are exceptional, in which it is discussed whether they are intermingled Conectivitis or vasculitis. All of them have little expressiveness clinical and radiological, are very heterogeneous and Its pathogenesis is poorly understood. In these rare ways there four that have poor prognosis and little response therapeutic, so the interest in them is every most important day: we are referring to the pulmonary fibrosis, acute interstitial pneumonitis, vasculitis and bronchiolitis obliterans.
In general, the demonstrations Pulmonary diseases in patients with RA predominate in men with double incidence than in women, unlike the disease synovitis . It usually appears after 40 years. 10% of the pleuropulmonary manifestations precede arthritis and in two - thirds delos appears after 4 to 6 years of evolution of arthritis. The cough, chest pain, dyspnea or hemoptysis are late manifestations. Simple radiology is scanty and non-specific and the histopathology is heterogeneous in relation to the chronology of the facts and the location.
Then we will describe the various pleuropulmonary manifestations in patients with RA.
Pleuropathy with or without leak |
Pulmonary nodules without coniosis |
Caplan syndrome or coniosis with pulmonary nodules |
Pneumonitis or alveolitis diffuse interstitial |
Track alterations aerial |
Vasculitis with or without pulmonary arterial hypertension |
Apical fibrosis |
Syndrome shrunken lung ( shrinking lung ) |
Pathology of the wall thoracic |
Myopathies |
Alteration of costovertebral, costoesternal or chondritis and injuries bone |
Table 2 Pleuropulmonary manifestations of rheumatoid arthritis
Pleuropathy
The pleuropatía is, with infectious complications, the pleuropulmonary manifestation more frequent in patients with RA. The incidence is 0,3 % in women and 1.5% in men, who in general are over 40 years. The majority attend without clinic, which does not is usually beyond 5% and reaches 20% if they are does simple radiology. In post-mortem studies the frequency reaches 50%. The pleuropathy follows arthritis in 75%, are simultaneous at 20% and only 5% precedes the arthritis. Between 3% and 39% there is a spill pleural, which is generally subclinical and when there is characterized by pain and dyspnea in 38%, cough in 25% and fever in the 14%.
The pleural fluid is usually be an exudate with increased protein (4g/dl or more) cells (100-3,500 mononuclear and lymphocytes/mm3) and there are degenerate phagocytes with or without eosinophils, being typical that the macrophages have ingested IgM that is in their cytoplasm, and these cells are called ragocitos. Lalactate dehydrogenase (LDH), adenosine from aminase (ADA) and proteins are usually elevated and the rheumatoid factor can have higher titres than serum, which It suggests local training. A noteworthy fact is the reduction of glucose below 35 mg% with normoglycemia and is thought to be due to a selective blockage of glucose transport. The absence of microorganisms or malignant cells eliminates the possibility of effusion infectious or neoplastic. The biopsy with granulomas or rheumatic nodules give the diagnosis of rheumatoid pleuropathy. Restrictive pleuropatía is rare, the same as observing calcifications or large leak.
The treatment is done with anti-inflammatory drugs, low doses of steroids and rarely n eed perform centesis toraco thoracotomy or 1 to 4.8.
Nodules rheumatoid
These are rare forms that are seen in 1% of the radiology of patients with RA that tend to be smokers are patients with subcutaneous nodules, systemic alterations, high factor titers rheumatoid and antinuclear antibodies. Its size goes from few millimeters to more than 5 cm, unique or multiple, located at the periphery of the middle lobes and superiors. Half of them cavitate, but do not calcify if they are not accompanied by silicosis. They can study alone or with coniosis as is the case of the miners producing the Caplan syndrome that is later described as associated with other coniosis. Nodules without conosis predominate in the bases with diameters between a few millimeters to more than 5 cm. The edges are rounded or scalloped and little clear in general. They can cavitate by giving pneumothorax, pioneumothorax or hemoptysis. The course is capricious, with disappearance in months and only exceptionally precede arthritis.
In the miners of Wales, Caplan describes patients with rheumatoid arthritis who have pneumoconiosis with pulmonary nodules located in lung fields high Subsequently, they are described as associated with asbestosis or coniosis for talc, granites, aluminum, textile products and others inorganic powders. They are generally nodules multiple rounds with well-limited edges and minor size than nodules without coniosis.
The diagnosis of rheumatoid nodules should always be histological with its central fibrinoid necrosis, its palisade of histiocytes and the mononuclear corona on the outside. It can be seen in initial forms is vasculitis with deposits of immune complexes.1–5
Interstitial alterations: alveolitis or fibrosing pneumonitis
Interstitial pathology pulmonary is the first extra-articular manifestation described in 19487 and prevalence varies according to sample chosen and the methodology used as described before. The clinical radiological incidence of Pulmonary alterations is 5%. With the use of pulmonary death tests, three-quarters of patients they have ventilatory alterations with predominance of obstructive alterations of 41% in 104 patients over restrictive with 21%. If to these alterations we unite the incidence of 37% reduction of the TLco we can conclude that more than half of patients with RA have criteria functional interstitial disorders.8 With the lung biopsy, alterations reach 80% of patients in which, together with the functional and pathological data, supports the existence of the rheumatoid lung. The clinical, functional alterations, findings radiology and the histopathology of alterations interstitials in patients with RA are similar to those in the idiopathic pulmonary fibrosis. Pathologists and clinical as RY Katzenstein et al.,9,10 describe four forms with translation prognosis-therapeutic, so in the We can subclassify them in: interstitial pneumonitis common (NIC): the form most frequent in subjects of 50 years with slow onset and poor prognosis due to the lack of or little response to corticosteroids, since these are scarring lesions of different age formed by fibrosis plaques with foci Fibroblastic and pitted lung with scanty inflammation and without bronchiolitis or hyaline membranes. The three other forms show a good response to corticosteroids in subjects from 30 to 40 years with more acute beginnings and pathology more inflammatory than fibrotic and not There is a honeycomb lung and they are: a) interstitial pneumonitis desquamative without hyaline membrane or bronchitis , without fibroblast proliferation in which there are many peribronchiolar macrophages and collagen fibrosis makes 25% do not respond well to treatment; b) pneumonitis acute interstitial without bronchitis , without macrophages intraalveolar and sometimes with hyaline membranes and excellent response to corticosteroids, and c) finally, pneumonitis nonspecific interstitials with variable onset and that appears about 50 years and with 10% mortality and in interstitial inflammation occasions, clusters of intraalveolar macrophages and focal bronchial inflammation without Hyaline membranes and variable fibrosis with proliferation diffuse or focal fibroblastic . The authors exclude idiopathic forms of bronchiolitis obliterans with pneumonitis organized by its high frequency of association to other entities (infections, post-transplants , drugs, diseases like connectivitis ) and so it cannot be excluded since in these forms the RA is included, and there is no association with the interstitial lymphocytic pneumonitis because it is a lymphoproliferative process associated with immunodeficiencies, and neither include giant cell pneumonitis here its association with heavy metal pneumoconiosis.
Patients with interstitial lung pathology have AR with factor rheumatoid and antinuclear antibodies similar to what you see in idiopathic pneumonitis. The clinic is late with progressive dyspnea, dry cough and tardily acropachy. Right heart failure, the Pulmonary arterial hypertension and cyanosis are very little frequent In the exploration there are bibasal crackles inspiratory In radiology usually see pattern is interstitial reticular, nodular reticulum or lung Skewed with severe diffuse pulmonary fibrosis better analyzed with High resolution CT, with infiltrative alterations that they respond partially with corticoids or it is fibrosis established and irreversible. Most arthritis proceeds to pulmonary alterations and a small percentage of interstitial manifestations precede even in years to arthritis. The prognosis is similar to that of idiopathic forms and survival at 5 years is 50%. There may be pulmonary hypertension and Signs of right failure and exceptionally vasculitis.
Function tests They characterized by lung ventilatory pattern not obstructive (reduction of FVC, TLC and FEV1 /FVC ratio and high RV/TLC), mixed pattern with or without reduction of TLco and PAO 2.
Phan in et al.5 describes a series of causes of interstitial pathology to take into account when making the diagnosis of pathology interstitial lung disease in patients with RA: a) agents physicochemical (gases, vapors, solvents, aspiration of acids or bases); b) inhalation of organic and inorganic powders (asbestos, aluminum , silica, farmer's lung and other forms of extrinsic allergic alveolitis); c) pneumonitis virus; d) iatrogenicity by drugs; e) uremia, failure of left ventricle; f) other conectivitis with commentators such as lupus, Sjögren's syndrome , mixed disease , is cleroderma or others, and g) forms of fibrosis idiopathic.1–4,8–11
The manifestations of lung airways in RA were the "Ugly duckling" since well into the decade of the seventies the alterations of the airways were relate to smoking and with pollution or infections. It also influenced the no sufficiently sensitive methods were available almost the decade of the eighties. Collins et al in 1976 revised a large sample of patients, but they include many smokers and for the first time the alteration of the airway by RA 12; and as always they have of serious events to be studied better, what which happens the following year when Geddes et al 13 describe 6 patients with a severe, progressive picture and fatal that did not respond to various steroid treatments were immunosuppressant’s, 5 of them were patients with RA and They had been treated with d- penicillamine. The post-mortem histopathology showed the existence of bronchiolitis obliterans and This led them to perform other works demonstrating that the AR can cause airway obstruction and which is synergistic with tobacco. In this same decade, other authors confirm the obstruction of the airborne RA out of smoking habit 14-17. As of the eighties, discusses whether obstructive alterations or restrictive, and in this sense, in the thesis I read in 1988 and in a large sample of 104 patients with RA I could see a frank predominance of obstruction eleven (Table 3).
Ventilation alteration |
Percentage |
Obstruction to flow aerial |
41 |
Alterations restrictive |
twenty-one |
Combined forms or mixed |
eleven |
Table 3 Ventilatory alterations in 104 patients with rheumatoid arthritis
In the analysis of data whose classification in the various patterns is based on the criteria given by Miller 18 which are quite restrictive is clear, at least in this sample, that in the patients with RA there is obstruction, and having only 11% of smokers there is still 31% of obstructives without being related to tobacco; there was no history of pollution, infections or other causes of obstruction and for this reason it makes us relate this alteration primarily with the AR. In the same decade, Begin et al refer in 6 patients with RA and associated Sjögren's syndrome that in lung biopsies detect alterations similar to those of the glandular biopsy and that obstructive pulmonary alterations in patients with RA are due to Sjögren's syndrome associate,19 which is not accepted by other authors. AND ntal sense, in a study of patients with Sjögren primary the incidence of obstruction and The restriction is similar, so it must be taken into account , and even more so because patients with RA who suffer from of secondary Sjögren or with anti-Ro antibodies do not they should be given gold salts and less aug-penicillamine, since they are hypersensitive and the yatrogenia is more intense We must remember the work that only 10% of the patients in the sample had clinical evidence or alterations in radiology simple and that this great frequency of functional alterations are slight in the majority, that is, that it is a subclinical alteration very little evolutionary. Outside some cases with bronchiolar alteration, the great most patients give no reason for us worry excessively of this manifestations.9
The various alterations of the Respiratory tract can be studied Subclassifying them by their topography:
1) Obstruction of proximal pathways (larynx to main bronchi) with three forms: a) rheumatoid nodules in the tract; b) tracheomalacia , and c) cricoaritenoiditis . The first two are cases exceptional with easy solution in the first and not In a second. The cricoaritenoides is a small diarthrodial articulates tion that abducts and ab duce the ropes vocal and can inflame causing hoarseness and in some cases inspiratory stridor. In 30% of patients with RA it can There are alterations of the voice, in 50% of the necropsies there alterations and through laryngoscopy, method common to detect this alteration, in 32%, what reaches 54% if we make a TAC that level during dela disease. In general it has little clinical significance, but it should be taken into account when intuiting surgery to these patients or because it favors aspiration, and more during decubitus.1
2) Alterations of bronchial pathways to the small way correspond to bronchiectasis, chronic bronchitis, asthma and other processes that are generally not related to RA, but they can be presented together.
3) The manifestations of the Small way are important, not because of the frequency, but because they are potentially serious. The first to describe them were Collins and Geddes, who, respectively, describe obstructive pictures in RA of non-smoking patients and the second public 6 commented cases of bronchiolitis that related in much with d- penicillamine.12,13
The little way corresponds to the membranous bronchioles and Respiratory bronchioles correspond to divisions 16 to 23 and have a diameter less than 2 mm. Your interest resides in that, because of the great division, they have a short journey, but its area is large and in the first there is no transfer of gases and in the respiratory with alveolar ducts and alveoli in its wall allow the exchange of gases.14,15 Being of small length, the bronchioles are easily invaded distally from the bronchi and proximally from the alveoli. By these reasons, the pathology of the small way is the apple of discord for pulmonologists pathologists and radiologists. At a functional level we can find obstructive or restrictive pictures, but the clinic is usually silent and appear late with dry cough and dyspnea of effort, to which fever and others can be added systemic symptoms; in some forms of constrictive bronchiolitis dyspnea is abrupt, but there is no wheezing or other asthma or pulmonary thromboembolism data . In the exploration, just some crackles basal inspiratory or more intense sounds described like crackles; and you do not hear, yes it is isolated pathology, of these routes the roncus or sibilants of other pathologies. The possible causes of bronchiolitis are summarized in Table 4 Of course we should have in account here tobacco, chronic bronchitis, asthma, bronchiectasis and cystic fibrosis that can invade distally these pathways in their evolution, or emphysema and the alveolar processes that invade bronchioles retrograde (aspiration pneumonitis, chronic eosinophilic pneumonitis , pulmonary fibrosis idiopathic and other alveolar processes).
Diseases systemic rheumatism: rheumatoid arthritis , l upus erythematosus, Sjögren's syndrome , scleroderma , dermatopolimiositis , mixed disease and vasculitis as the Wegener 's granulomatosis or Churg -Strauss |
Infections: virus ( cytomegalovirus , adenovirus, respiratory syncytial virus and retroviruses), bacteria (pneumococcus, Legionella ) and others such as Mycoplasmas and Nocardias |
Inhalation of Toxic fumes and gases (tobacco, sulfur dioxides , nitrogen, chlorine , ammonium, ozone, trichlorethylene , phosgene, talc, cadmium oxide, sulfur and fluoride powders ) Y mineral powders or acid aspiration or bases |
Reaction to Drugs: gold salts, d- penicillamine , salazopyrin , sulindal , bleomycin , busulfan , cyclosporins , amiodarone yparaquat |
Other: colitis ulcerative, thyroiditis, post- irradiation syndrome , reaction of the graft against the host in transplanted lung, heart and bone marrow bone among others |
Table 4 Etiology of the bronchiolitis
In practice we must take into account these charts in those patients with those rheumatic diseases when there is dyspnea and also take some of these drugs, and especially in AR that have secondary Sjögren's syndrome in relationship with gold salts and of course lad-penicillamine. Two forms of bronchiolitis appear to be differentiated:16–25 bronchiolitis proliferative and constrictive bronchiolitis.
bronchiolitis proliferative , hyperplastic with or without pneumonitis, is rare and usually occur in both sexes equally towards the sixth decade of the lifetime. It consists pathologically in a bronchiolitis that is extends to ducts and alveoli and the injury is a bronchial epithelial lesion followed by an exudative intraluminal fibrinoid lesions forming as a round joined by a pedicle to the wall or not (Masson's bodies ) with immature fibroblasts, and invade and thicken duct walls and alveoli (pneumonitis or organized alveolitis) with alveolar macrophages loaded with lipids. In the first phase there are diverse cellular infiltrates and intensity variable that evolve towards fibrosis. The clinic is the described in bronchiolitis and will depend on the origin and extension. The analytical shows speed of very high globular sedimentation (ESR) with leukocytes normal chest radiology evidence bilateral infiltrates, multifocal, sometimes migratory, and in the TAC alveolar consolidation and glass images tarnished. Pulmonary functional tests show restrictive pattern to which you can add reduction of the TLco. The important thing about this process is its good response to corticosteroids with good prognosis, although recur frequently.
Constrictive bronchiolitis very rare, is limited to the membranous bronchioles and does not there are no alveolar or bronchial alterations. Here the injury is in the wall with injury submucosa initially, diverse infiltrates with great fibrous reaction that ends up reducing or canceling the light fibrosis, and we can find mucus plugs and bronchiolectasis. The clinic corresponds to cough pictures dry and progressive dyspnea, sometimes severe, suggesting pulmonary embolboembolism with normal or mild radiology hyperinflation with obstruction to the flow air without alteration of the TLco ; It is intense and progressive, without response to bronchodilators or to corticosteroids For all this it is a way with serious prognosis, unlike the other way. of all modes, there is evidence of at least partial responses in patients treated with immunosuppressants in single or combined therapy .
Both forms must be analyzed etiologically looking for infections, history of inhalation or pollution. In transplanted patients, and especially in the lung, constrictive bronchiolitis occurs in the third of them. Through the clinic, radiology, pulmonary function tests, CT, washes, bronchoscopy and biopsy we will make the diagnosis, and After avoiding toxic inhalations and suspending the treatments involved, treatment with corticosteroids and immunosuppressants.
Vasculitis
«Where there are no glasses there is no inflammation »is a fundamental axiom of injuries related to RA; It endotheliitis usually common, perolas vasculitis are rare. Fassbender describes a form systemic necrotizing similar to the PAN with bad prognosis, another with digital endothelitis with a phenomenon of Raynaud and occasionally pulmonary hypertension. Later another form with infiltrates is described lymphohistiocytes in muscle arteries with proliferation of the average and occasionally thrombi that close the light of the glasses.1,8
Alterations disorders in patients with rheumatoid arthritis
Contrast that the prevalence clinic is only 1% to 5% in patients with AR, while the post-mortem pathological findings are between 30% and 50%.
Injuries are infiltrated inflammations or fibrosis basically that can reach ballast layers and are found more in patients with forms Aggressive, seropositive joints.1–4 Table 5 summarizes the frequency of different cardiac alterations in the pathology and in the clinic.
Injuries |
Histological frequency |
Clinical frequency |
Pericarditis |
11% -50% |
1.6% -2.4% |
Non-specific myocarditis |
4% -30% |
Weird |
Granulomatous myocarditis |
3% -5% |
Weird |
Disease of the conductive tissue |
? |
8% -10% |
Coronary arteritis |
15% -20% |
Weird |
Valvular disease |
6% -60% |
Weird |
Table 5 Cardiac Changes in Arthritis rheumatoid
Pericarditis
It is the manifestation cardiac disease, it may occur alone or with pleuritis, and its clinical incidence ranges from 1% -10%, in echocardiographic studies between 20% -31% and in necropsies reaches half of patients with RA. his annual incidence is 0.3% in women and 0.44% in mens.
The clinic usually correspond to the acute form of pericarditis with effusion, which it is expressed by chest pain and vascular congestion. It can be seen in AR initial or evolved and the echocardiography shows thickening of the two layers with leak; the puncture allows toverify an exudate with elevated cells and proteins, factor positivity rheumatoid with degrees higher than blood peripheral. Immune complexes, cholesterol and cholesterol crystals in evolved forms, there may be figures high neutrophils, red blood cells, ragocitos and descent of complement and glucose. If the biopsy is done, we can find a nonspecific inflammatory infiltrate or granulomas- rheumatoid nodules more specific. In general they have a benign course, with good response to corticosteroids and recur 15%. The forms restrictive or pericardial tamponade is exceptional and they usually respond to corticosteroids and surgery, resecting the parietal serosa. Sometimes you need to add immunosuppressants to prevent reactivation.
Myocarditis
Its prevalence is low if the We compare with other connectivitis; in general it is about nonspecific myocarditis or focal fibrosis they are only discovered in necropsies. There can be serious ways such as necrotizing myocarditis, myocardial disease diffuse or hypertrophic cardiomyopathy. Considered In general, nonspecific myocarditis have a prevalence of 15%, myocardial nodules do not pass of 5%, coronary arteritis is rare, but studies post mortem come to give figures of 20% and he says that before his suspicion we must establish a treatment immediate with corticoids and cyclophosphamide. They describe autoantibodies to muscle fibers and structures cardiac muscle, but its meaning is unknown. There are arrhythmias ( complete or partial AV blocks ) due to granulomas, infarcts or infiltrates. In patients with intense RA and with rheumatoid nodulosis can detect aortitis granulomatous.
Endocarditis
20% -30% of patients with AR have valvular alterations. The injury more Aortic regurgitation is common, with rare stenosis; the mitral and tricuspid is affected very few times. The lesions detected correspond to thickening valvular, nodules on the cusps of the valves or fibrosis. The nodules are usually seen in patients who have rheumatoid nodulosis These can perforate, breaking shells and cords, which causes very bad heart failure serious that forces to intervene surgically.
Manifestations ophthalmic in patients with rheumatoid arthritis
The ocular alterations are more prevalent in patients with advanced RA, seropositive, erosive and with other manifestations extraarticulate. Their presence worsens the prognosis of arthritis and can alter vision. The most frequent and specific to the disease are the alterations of the anterior pole of the eye and especially the sclerosis, which are more frequent in women. When studying the origin of a sclerosis by the ophthalmologist more than One third of these are due to rheumatoid arthritis. Perhaps the most frequent alteration is the dry keratoconjunctivitis of Sjögren's syndrome associated secondary and iatrogenicity to drugs used in the RA treatment.1-4.26
Conjunctivitis and keratitis
As we have referred previously, the most frequent is keratitis sicca, present between 20% -45% of the AR in its course evolutionary. They are asymptomatic in general, but some forms Severe injuries and corneal perforation, specifying aggressive treatment with immunosuppressants and corneal transplant. He Diagnosis is easily performed with the test Schirmer and staining with rose bengal or fluorescein. There are very infrequent forms of acute keratitis, sclerosing, keratolysis with skin ulcers that need treatment with corticosteroids and immunosuppressants.
Scleritis and episcleritis
Episcleritis has a incidence of 0.17%, can be focal or diffuse, does not alter the vision and you see a red eye that has a self-limited course in 4-6 weeks. We rarely observe complications (uveitis, cataracts). Scleritis are more frequent (incidence of 0.67%), are usually detected in the sixth decade, more in women, and almost 70% are forms bilateral is more serious than episcleritis and is the more specific to the AR. The clinic characterized by pain, photophobia, epiphora, visual disturbances, reddened eye and in nodular forms and may perforate the eye ( scleritis perforating ). It can be accompanied by glaucoma, cataracts, retinal detachment and nerve injuries optical. The treatment depends on the severity and is done with corticosteroids and immunosuppressants.
Ocular yatrogenia medication
In short, the treatments used (such as NSAIDs and gold salts) can be deposited in the crystalline altering the vision. The antimalarials are deposited in the cornea and retina, with visual loss in few cases if the established controls are maintained. The corticoids are associated with subcapsular cataracts, so we must have them under observation and remove them when Signs of yatrogenia appear.
Manifestations neuromuscular diseases of rheumatoid arthritis
The pain and disability that The arthritic condition does not allow the patient to be aware of muscular weakness or paresthesias, and this state does not allow the doctor to do a good exam physical. Despite this, we must bear in mind that a patient with RA may have neurological symptoms and must do a thorough study of:1–4
Alterations of the nervous system peripheral
1) Neuropathies by Entrapment.
2) Sensory neuropathy diffuse
3) Mononeuritis multiple.
4) Neuropathy autonomic
Neuropathies by entrapment in RA are due to the underlying inflammatory process, to the rheumatoid nodules or the destruction and joint deformities.
The most neuropathy frequent corresponds to the tunnel syndrome of carpus, which is due to the understanding of the median nerve in the carpus due to synovitis, or flexor tenosynovitis. 50% -65% of patients with RA will suffer, attend acroparesthesias night predominantly nerve hypoesthesia medium and the Tinel and Phallen tests are positive, confirming with driving techniques of nerve to measure the severity and indication surgical Before treating, they should be discarded and treated other causes such as diabetes, hypothyroidism, infections or secondary amyloidosis among others. The treatment is directed to reduce or cancel the inflammatory process with the treatment of AR, immobilize with resting splints and, if it fails, infiltrate them or intervene surgically. 25% of patients refer clinic posterior tibial nerve entrapment or tarsal tunnel syndrome with paresthesias, pain in plant, fingers, ankle and sometimes calves that can wake them up and improve with walking. The study of conduction of the posterior tibial nerve will assess the severity and the need for surgery.
Other entrapments described are those of the posterior interosseous with muscle atrophy , radical neuropathy that makes it impossible or difficult extension of the fingers, the compression of the ulnar in Guyón's canal , elbow or cervical level more rarely.
Polyneuritis and mononeuritism are multiple symmetric distal forms or forms asymmetric with worse prognosis. Is it so related to the presence of systemic vasculitis. The neuropathies of the autonomic nervous system are usually be exceptional and in general are subclinical.
Manifestations of the system central nervous
The central alterations neurological diseases in RA are very rare if we except cervical myelopathy. This injury is due to compression or narrowing of the cervical spinal canal by dislocation or atlas-axis subluxation. 20% of the patients with RA have radiological criteria (odontoid separation -atlas greater than 3 mm in cervical radiography of flexion profile), although the Cervical myelopathy is uncommon. It usually occurs in patients highly evolved, seropositive, with erosions and deformities. The Clinic consists of a high cervicalgia with reference to occiput or cervical roots, with weakness in extremities inferiors, sign of Babinski to tetraplegia and one must have account for traffic accidents with subsequent shock to intubation during anesthesia. The treatment consists of immobilize the spine with a collar, treat osteoarthritis intervene with vertebral fixation. Another way to displacement is the invagination of the odontoid towards the inside the skull, which may require surgery. There are paintings described in the chapter of central vasculitis and transverse myelitis, but they are exceptional forms. Other times there are agranulomas or rheumatoid nodules with clinical central or radicular compression.
Manifestations muscular
It is common to detect weakness and muscle atrophy in patients with RA, causing more functional disability and pain. These manifestations are related with the activity of arthritis, with inactivity, the use of corticoids and associated neuropathies. The Association of polymyositis with RA is exceptional. Sometimes alterations in muscle biopsies those are nonspecific.
Manifestations kidney
In the kidney we can find us with several alterations that mostly do not are related to arthritis, and I mean the alterations of the sediment (proteinuria, leukocyturia , hematuria , interstitial nephritis or tubular necrosis with or without renal failure and hyperkal emia by NSAIDs and / or analgesics). The use of gold salts and d- penicillamine for arthritis may be accompanied by a syndrome Nephrotic due to membranous glomerulonephritis or due to wing secondary amyloidosis and tubular acidosis is related to the presence of secondary Sjögren's syndrome.1-4,27–29
There are authors who describe disturbances of urine sediment due to arthritis rheumatoid and even true glomerulonephritis are described segmental or proliferative, but they are exceptional and must look for systemic lupus or vasculitis systemic.
Dermal
Alteration - most characteristic and frequent skin of AR are the rheumatoid nodules which have already been discussed. He the rest of the manifestations are due to vasculitis (ulcers, purpura) or to the iatrogenicity of NSAIDs, background treatments and other therapies. Dry skin and mucous membranes with or without purpuric lesions can relate to Sjögren's syndrome.
Digestive
In the digestive tract we can see dyspepsia, erosions, ulcers and perforations iatrogenic to NSAID. Vasculitis can cause ischemia, hemorrhage or perforations, toxic hepatitis due to NSAIDs, hepatitis autoimmune syndrome in Sjögren and hepatosplenomegaly due to amyloidosis.
Hematologic
Anemia is undoubtedly the more frequent extra-articular manifestation ; in its Most are anemias normocytic - normochromic , less frequently normocytic-hypochromic or microcytic anemias , and very often they are megaloblastic and hemolytic. They are multifactorial deorigen: a) by the basic inflammatory process in relation to the acute phase reactants by the improvement in treating arthritis; b) by digestive dehierro losses due to iatrogenic NSAID and altered laliberación of Fe from bone marrow; c) by reducing the half life of red blood cell; d) lower spinal formation with erythropoietin or staraumented , but insufficient to compensate for the medullary formation, and e) by the activity of TNF, which inhibits the formation and improvement with anti-TNF antibodies. Portodo this, most patients have anemia.Cerca have 25% B 12 deficiency Folic acid, so they mask the microcytosis. Treatment begins by treating arthritis well, supplying Fe sifalta and using erythropoietin in anemias that should not be transfused.1-4
The erythropoietin that stimulates the formation of erythroid colonies has been described as elevated , normal and low. We, in a review of 136 patients with RA, detected high figures, but not enough to improve anemia, and, when administered, improved and avoided transfusing at least 50% of patients with anemia.30 The anti- inflammatory treatments and remission- inductive drugs (background T) may present with cytopenias or aplasiamedullary.
In 40% of patients with AR we detected more than 5% of eosinophils in peripheral blood, more frequently in seropositive patients and patients with increased IgE class rheumatoid factor have worse prognosis. Thrombocytosis is common and reactants withother acute phase relates. The thrombocytopenia must be encuenta regarding NSAID treatments, treatments background and especially immunosuppressants. A small subgroup of patients with RA show a large clonal population of large lymphocytes in peripheral blood, marrow, or liver. It is a non-producer population of IL-2, without receptors for immunoglobulin Fc, they form rosettes with lamb erythrocytes, they have little response to amitógenos and they lack natural killer activity (NK).
75% of patients have neoplasms, with a higher prevalence in men with AR-active and active; Sometimes they simulate neuroproliferative processes. The biopsy shows follicular hyperplasia and no evidence of malignancy.
Manifestations bone
Osteopenia and loss of Bone mass is frequent in patients with RA. There are two ways: a) the juxta-articular , by the synovial inflammatory process and that relates to the increase in PGE2 induced by cytokines (IL-1, TNF), and b) diffuse osteoporosis, which is multifactorial origin, in which the activity is included inflammation, immobility, corticosteroid treatments and immunosuppressants, lack of calcium and vitamin D and factors hormonal (menopause in women). For this reason, vertebral bone fractures and at neck level femur, and less frequently stress fractures in bones of the legs or pelvis. The treatment consists of treating it AR so that it maintains good physical activity, giving calcium and vitamin D 3 supplements , and if there osteoporosis using the same anti - reabsorptive therapy osteoporosis in general (hormone, calcitonin, bisphosphonates).1–4
Syndromes associates
We will not comment on the group of interspersed with other connectivitis, except the syndrome Sjögren secondary for being very associated, and we will comment on the Felty syndrome, which may well be considered as a extraarticular manifestation without rank no sological.
Syndrome of Felty
It was defined by Felty in 1932 as the AR triad, splenomegaly and neutropenia. To articular clinic we should add the presence of ulcers in the legs, oral ulcers and sometimes in the cornea. Neutropenia, adenomegalias and splenomegalies of various sizes absent in a third of patients. One percent of RAs have it and it is usually associated with erosive forms and seropositive There is a strong association to HLA- DR4 (80%), and especially to subtype DRB1 0401. There may be infections recurrent when neutrophils are very low. Other Associations are episcleritis, serositis and peripheral neuropathy. The treatment is controversial and they are used corticosteroids, metrotrexate and in some cases salts of gold or splenectomy. In very serious cases it is used cyclophosphamide with corticosteroids at high doses even if the risk of infection.
Secondary Sjögren's syndrome
The syndrome Sjögren (SS) is a conectivitis characterized by sialoadenitis, which like the synovitis of RA has a high degree of infiltration by CD4+T lymphocytes of subgroup Th1. The prevalence is 1% for RA and between 0.5% -3% for the SS, that Bloch subclassifies in primary forms (SSp) and secondary (SSs) in the sixties. Almost half of the AR attend SSs and more than 60% of SSps are suffering from arthritis non-erosive, and both entities are more frequent in women with 4/1 for the AR and 10/1 for the SSp. Genetically, and with In relation to HLA-II, RA is associated to DR4 and SSp to DR3 , that is, they are well-defined entities when we talk about forms of SSp and AR. When the SSs goes with AR, what differential characteristics does it have? The answer is that it is more benign, less evolutionary, alterations extraglandular are smaller, there is less parotidomegaly and at analytical PCR is almost always elevated in RA active and barely increases in SS; the cytopenias are more frequent in SS that RA and anti-Ro and anti-LA antibodies are most characteristic of the SS and are barely detected in the SSs to AR. The lymphoproliferative processes predominate in SSp (4.3%) compared to AR (0.8% -1.6%). The diagnosis of SSs follows the same steps as the SSp, but with the AR criteria in case of association to it and the therapy is identical to the SSp31
Manifestations of the complications of rheumatoid arthritis
In this section we will summarize the manifestations in three groups:
1) Amyloidosis high school.
2) Those due to drug iatrogenia .
3) Other: arteriopathies scleroses and infections.
The sections of the infection in patients with low defenses and that of the yatrogenia to the various treatments we will not comment them for their extension and we ended up with amyloidosis high school.
Amyloid is a substance pathological protein that is deposited at the extracellular, being able to give tissue dysfunction and organs, where it is deposited. It is formed in 95% by fibrillar proteins and the remaining 5% is a glycoprotein or component P. In primary forms the fibrillar protein is a light chain of immunoglobulins that synthesizes B lymphocyte and in amyloidosis secondary is a non-immunoglobulin protein that synthesizes the hepatocyte The causes of secondary arthritis are multiple: chronic infections (tuberculosis, bronchiectasis, osteomyelitis) and currently chronic inflammatory processes (AR, juvenile chronic arthritis, spondyloarthritis, lupus erythematosus and other connective tissue), neoplasms and familial Mediterranean fever predominate . Rheumatoid arthritis is associated with amyloidosis between 10% -25%, with an incidence of 5% -19% and contributes to the increase in morbidity and mortality of patients with RA.1–4 Amyloidosis in RA rarely occurs before 2 years of evolution and is often seen in patients with very advanced forms and persistent inflammatory activity. Of the 64 patients with secondary amyloidosis described by Gertz at the Mayo Clinic32 three quarters of them are due to RA and the most frequent presentation is due to kidney deposition with proteinuria, 25% develop nephrotic syndrome and some renal failure; diarrhea, constipation or malabsorption follow but gastrointestinal manifestations are not usually seen in patients with RA. Less than 5% show clinical signs of hepatosplenomegaly, adenopathy or the carpal tunnel.33,34 In extensive studies of patients with RA and amyloidosis with 120 patients, renal and gastrointestinal alterations exceed 50%, cardiac alterations 30% and survival at 4 years is close to 60% and most of the death is due to renal failure and infections.35 The biopsy that confirms the diagnosis is that of subcutaneous fat in the abdomen, the most accessible rectal, with high frequency of positivity, and of course the renal because it is where there are more amyloid deposits with positivities greater than 90%.
The osteoarticular manifestations in amyloidosis are varied: erosions and subchondral cysts, subluxations, osteoporosis, lytic bone lesions, osteonecrosis, subcutaneous nodules, contractures, pathological fractures, spondyloarthropathy and neuroarthropathy. There may be deposits of crystals and iron in the histology.
The treatment of amyloidosis is contradictory in terms of results and most of them are works with little sample or short-term treatments, so the answer is difficult. However, in the secondary forms the first thing is to treat the inflammatory process well or the infections if they exist. Other treatments are mattresses and immunosuppressants alone or combined ( methotrexate , cyclophosphamide and corticosteroids).36–38
We should refer to two other topics that are infection in patients with rheumatoid arthritis and the extensive and heterogeneous iatrogenicity to the multiple therapies used in rheumatoid arthritis, but there are extensive reviews to inform about those topics l.
Occupational therapy counseling should be considered for those patients who experience functional limitation. It is important to coordinate all the professionals involved in the treatment of the patient, an approach oriented to specific problems and an adequate assessment of the effects of the interventions. In the care of a patient with rheumatoid arthritis, the individual needs of the patient must be taken into consideration through the involvement of a multidisciplinary team.
A personalized management plan should be established, in which short, medium and long-term goals and objectives are defined, appropriate to the particular functional capacity, considering that the RA is an entity with variable prognosis, with the objective of achieving full inclusion or reintegration of the patient in his society.
It is recommended the implementation of a patient education program that includes at least the following aspects: 1) Provide information concerning the disease, treatment and outcome 2) Monitoring and control of the adverse effects of DMARDs, biological therapy and NSAIDs; 3) Physical and occupational therapeutic plan; 4) Pain control; and 5) Joint protection.
Non-pharmacological treatment interventions
Such as dynamic exercise, occupational therapy and hydrotherapy are interventions that are useful in the comprehensive care of patients with rheumatoid arthritis. Physical exercise and strengthening exercises are recommended in patients with early rheumatoid arthritis. Exercise is prescribed in an attempt to modify the adverse effects of RA on muscle strength, aerobic capacity and endurance. All patients with rheumatoid arthritis should receive indications about the exercises to be performed, and should be personalized according to age, number of joints involved and disease activity. Exercise is recommended, from the moment of diagnosis, a program of aerobic physical exercise. Initially, it is preferable that it be supervised to individualize it and adapt it to the degree of physical preparation and to the concrete, joint and extra-articular circumstances derived from the disease and the concomitant pathologies. Aerobic exercises can be combined with muscle strengthening exercises (regional or general), flexibility and improved coordination and manual dexterity. Physician’s mustprovide education on the joint protection measures for patients with rheumatoid arthritis. The patient with rheumatoid arthritis should be given access to adequate psychosocial support, including aspects related to interpersonal relationships and even sexuality. Food supplements are not indicated as part of the treatment of the patient with early rheumatoid arthritis. Acupuncture has not shown utility and its usual use in all patients with rheumatoid arthritis is not recommended. Rehabilitation includes the evaluation, prevention and treatment of disability, with the aim of facilitating, maintaining or returning the highest degree of functional capacity and independence possible. Its main purpose in rheumatoid arthritis is to treat the consequences of the disease (pain, muscle weakness, limitation in daily activities) and prevent functional deterioration. The low-power laser and the TENS, in an isolated and independent way are effective for reducing pain in the short term.
The application of TENS is recommended to reduce pain (the TENS has the advantage of the convenience of application with portable devices to use at home). The combination of paraffin (thermotherapy) and active exercises are effective in limiting pain. The application of heat and cold can provide temporary symptomatic relief of pain and stiffness. The data on ultrasound, muscle electrostimulation and magnetic therapy are still insufficient to recommend them on a regular basis, but should be considered in selected cases that have not responded to other alternatives. In the phases of active inflammation (with the main objective of avoiding pain and reducing inflammation), static orthoses can be used (initially all day and then only at night). If the patient has functional problems, functional orthoses adapted to the specific problem and to the anatomical area that interferes with the function can be associated during the day (part-time).
Pharmacological treatment (aine and steroid)
NSAIDs are clearly indicated for the control of inflammation and pain in rheumatoid arthritis and are superior to pure analgesics such as paracetamol.Nonsteroidal anti-inflammatory drugs (NSAIDs) should be considered in the treatment of patients with rheumatoid arthritis, after evaluating the individual risk at the gastrointestinal, renal and cardiovascular levels.There is no difference in efficacy between non-selective NSAIDs.An evaluation of health technologies concludes that COX-2 inhibitors have an efficacy similar to NSAIDs.NSAIDs that specifically inhibit COX2 haven a better safety profile at the gastrointestinal level.
NSAIDs are used to reduce the symptoms ofpain and inflammation in rheumatoid arthritis.They should not be used as a single drug and do not replace DMARDs.Any NSAID must be used at maximum dose for at least one week before considering that there is a therapeutic failure.Once the symptoms are controlled, NSAIDs should be used at the lowest effective dose.It cannot be recommended, based on efficacy, no NSAID over another (in particular, the efficacy of traditional NSAIDs is similar to that of coxib).The topical route is less effective than the oral route.The side effects of NSAIDs are dependent on the dose and duration of treatment, the main gastrointestinal, fluid retention and hypertension.Other less common but equally serious ones includes kidney disease and hypersensitivity.
It is not advisable to use two or more NSAIDs simultaneously, since concomitant use does not increase efficacy and instead increases toxicity.Should be considered the use of protecting gastric mucosa in patients with RA and risk factors for development of ulcers with NSAIDs (advanced age, prior history of gastrointestinal ulcer sites within, concomitant use of steroids, high dose NSAIDs) .The use of NSAIDs in patients at high risk of cardiovascular disease should be avoided.In patients with congestive heart failure, edema or uncontrolled hypertension, the use of NSAIDs should be restricted.
In patients receiving anticoagulants, NSAIDs should be restricted.The use of non-pharmacological measures (repos) is recommended as the first choice.Lose weight, cane, rehabilitation), paracetamol or codeine.In patients with renal impairment, the use of NSAIDs should be restricted.
In patients with liver disease, NSAIDs should be used at the minimum necessary dose for the shortest possible time and determining liver enzymes;in patients with severe hepatic impairment, use is contraindicated.
The use of low doses of glucocorticoids, in rheumatoid arthritis of recent onset (1 to 2 years of evolution) delays the appearance of radiological lesions.
Steroids reduce pain and inflammation and should be considered adjunctive therapy (temporarily) to DMARDs in the management of patients with rheumatoid arthritis.There is direct and indirect evidence that corticosteroids can be used as bridge therapy.In no case should corticosteroids replace the treatment with DMARDs.They should not be used as monotherapy and their use requires a specific indication.Given the association of the use of steroids with the rapid loss of bone mass, the joint use of vitamin D, calcium and other preventive treatments for osteoporosis is recommended in situations where a treatment of more than 3 months is expected.The adverse effects, benefits and risks of short- and long-term corticosteroid therapy should be considered and discussed with the patient prior to the onset of glucocorticoids.
The most effective corticosteroid to-articular intra use its local persistence and minor depression pituitary-adrenal axis is triamcinolone hexacetonide).In the absence of this drug in the market, a therapeutic alternative is methylprednisolone acetateOver a year, no more than three injections should be applied to a particular joint and there should be a minimum period of 30 to 90 days betweenone and another application.It is recommended to intentionally monitor the adverse effects of steroids, such as diabetes, cataracts, infection, systemic hypertension, dyslipidemia , atherosclerosis and osteonecrosis.avascular.
Pharmacological treatment (DMARD)
Early treatment of the patient with rheumatoid arthritis increases the likelihood of controlling the inflammatory process and reducing structural damage.The goal of RA treatment includes control of pain and inflammation, prevention of structural damage and induction of complete remission of the disease.Disease modifying drugs (DMARDs)they reduce the signs and symptoms of rheumatoid arthritis, improve physical function and laboratory markers of disease activity, as well as reduce radiographic progression.DMARDs for use in RA include: chloroquine , leflunomide , methotrexate , cyclosporin A, penicillamine, and sulfasalazine .The delay in starting treatment with DMARDs will beIt is associated with greater radiological damage and poor functional status.There is evidence that the relapse of signs and symptoms of RA is presented when suspending the DMARDs, which suggests that its sustained use is necessary.Patients with rheumatoid arthritis and factors ofpoor prognosis, they should initiate intensive treatment with DMARDs as soon as possible.In the treatment of the patient with RA;The combination of DMARDs compared to monotherapy should be preferred.
All patients with a definitive diagnosis of rheumatoid arthritis should start their specific treatment within a period of no more than 1 month, from the moment of confirmation of the diagnosis.The initial choice with DMARDs should take into account patient preferences and existing comorbidities.Patients must be informed of the possible benefits, risks and control requirements of the DMARDs to be used.Methotrexate (MTX) is a drug of choice in the treatment of rheumatoid arthritis and should be used in patients at risk of developing persistent disease.Induces greater sustained efficacy over time, has greater long-term adherence, reduces mortality has acceptable toxicity, is low cost and easy to dose.
The initial treatment recommended in all patients who have not been previously treated with any DMARD is the (MTX), due to its excellent efficacy and safety profile.In rheumatoid arthritis, without factors of poor prognosis (radiological erosions, rheumatoid factor, anti-CCP antibodies, presence of extra-articular disease, HAQ 1 or high inflammatory load), the initial use of DMARDs with a lower toxicity profile is acceptable. , among which antimalarials and sulfasalazine stand out.The starting dose of Sulfasalazine (SSZ) is 500 mg per day, increasing 500 mg every week to reach 2 grams per day.If the active patient persists, a maximum dose of 3000 mg per day can be reached.Methotrexate and sulfasalazine are DMARDs of choice, in the treatment of RA, due to a favorable efficacy and adequate toxicity profile.
The combination MTX+sulfasalazine is recommended in patients in any period with high disease activity and poor prognostic factors.The starting dose of MTX varies from 7.5 mg - 15 mg weekly.The current trend is to use higher starting dose (15 mg./Week).The addition of folic acid (5-10 mg/week) is associated with a significant reduction in the adverse effects of MTX.
The use of chloroquine is restricted to combination with other DMARDs.The combination MTX + chloroquine is recommended in patients with moderate and high activity of the disease, regardless of the duration of the disease and factors of poor prognosis.The combination MTX+Leflunomide is recommended in patients with intermediate or long disease duration (≥6 months) and poor prognostic factors.Close monitoring of liver function tests should be done.The dose of leflunomide for the treatment of rheumatoid arthritis is 20 mg per day.In order to achieve effective therapeutic concentrations more rapidly, a loading dose of 100 mg per day for 3 consecutive days can be administered.Leflunomide and sulfasalazine would be useful alternatives for the initiation of treatment, in case of contraindication to MTX.The combination of MTX and cyclosporineA , is more effective than cyclosporin A in monotherapy and moderately better than MTX.Combination therapy (not including biologics) in onset arthritis is more effective than monotherapy.The combination MTX+chloroquine +sulfasalazine is recommended for all patients with poor prognostic factors and moderate to high activity, regardless of the duration of the disease.It is recommended to assess the therapeutic failure or toxicity, within a maximum period of three months and, consequently, consider the change of treatment.The goal of treatment should be to maintain a DAS28<3.2.Triple therapy (MTX, chloroquine and SSZ) is no more toxic than mono or double therapy.
Biological therapy
The indication of anti-TNF includes patients with active or structurally progressive rheumatoid arthritis and documented MTX failure (taken for at least 3 months at an optimal dose).Biological therapy is recommended in patients with failure to at least the combination of 2 DMARDs (MTX, LFN, HCQ, SZA) at an optimal dose.Biological therapy must be indicated, monitored and supervised by a specialist in rheumatology.The goal of the anti-TNF treatment will be to obtain remission of the disease, a DAS28 <3. Taking into account its high cost, the biological agents should be considered as first choice drugs only in those patients that present a formal contraindication to DMARD. Taking into account their high cost, biological agents should be considered as first choice drugs only in those patients who present a formal contraindication to DMARD.In particular cases, biological therapy can be used initially, particularly in patients with poor prognosis factors and rapid progression of the disease.The simultaneous combination of biological agents is contraindicated at present.Comorbid states must be identified that contraindicate the initiation of biological therapy, including active and recurrent infections, as well as neoplasm.
The history of a malignant solid tumor in the preceding five years contraindicates the use of anti-TNF agentsPrior to the start of biological therapy, request: chest x-ray, PPD (anti-TNF), serology for hepatitis B and C viruses, as well as quantification of immunoglobulins (particularly conrituximab ).Biological therapy should not be used in pregnant women, in lactation and in patients with severe hypersensitivity known to the agent in particular.In patients with a family history of lymphoma, the risk/benefit ratio should be carefully evaluated before deciding the use of a TNF antagonist.Infliximab (IFX) delays radiological progressionof the disease.
It is recommended to use infliximab, initial dose of 3 mg/kg/infusion, and increase the dose if necessary without exceeding 6 mg/kg/infusion.Subcutaneous ETN+MTX orally in combination therapy is clinically more effective than MTX in short-term monotherapy .The combination etanercept + MTX significantly improves the clinical response, radiological evolution and functional capacity compared with monotherapy in both the short and long term (TEMPO study).In general, ETN is a well-tolerated treatment compared to MTX in parameters such as asthenia, headache or diarrhea.The adverse effect that occurs most frequently, compared with placebo or MTX, is the reaction at the injection site.ETN represents an effective and safe alternative in the treatment of rheumatoid arthritis, because it significantly improves the clinical response, radiological evolution and functional capacity of the patient.Adalimumab (ADA)+MTX is effective and safe in the treatment of RA, both early onset and long-term.Rituximab (RTX)+MTX is effective and safe for the treatment of rheumatoid arthritis with a positive rheumatoid factor, in patients with an unsatisfactory response to DMARDs.The most appropriate dose is 1,000 mg RTX in 2 doses 15 days apart.It is the one that provides a better clinical response according to the ACR criteria, without significantly increasing the side effects.
RTX in monotherapy or in combination with MTX or other DMARDs is effective and safe, and can be used in patients with therapeutic failure to anti-TNF, as well as initially in patients with contraindications to the use of them.Rituximab should be administered in conjunction with methotrexate in appropriate doses.It is recommended the application of methylprednisolone intravenously (100 mg) prior to the administration of rituximab to reduce the frequency and severity of reactions during infusion.Rituximab can be used in patients with active disease (DAS28>3.2 and rheumatoid factor positive, who have an intolerance incomplete response or proper use of anti-TNF drugs.Rituximab should be prescribed by a rheumatologist who is an expert in the diagnosis, evaluation and treatment of patients with rheumatoid arthritis.The drug must be infused into a specialized medical unit that has an emergency area.Patients with hepatitis B should not receive treatment with rituximab .Vaccines with inactivated pathogens for hepatitis B,Pneumococcus and influenza should be administered at least 4 weeks before starting rituximab administration.Rituximab should not be administered in children, pregnant women, or during lactation, allergy or hypersensitivity to rituximab or any of its components.The use of rituximab is contraindicated in the presence of active and recurrent infections as well as in severe heart failure (Table 6) (Table 7) (Table 8).
Characteristic |
Type-1 |
Type-2 |
Type-3 |
Type of polyarthritis |
Self-limited |
Minimally progressive |
progressive |
Identifiaction site |
General office |
General office |
Rheumatology clinic |
Percentaja de paclentes vlatos by the rheumatologist |
5-20% |
5-20% |
60-90% |
Increase of pllatellates by the rheumatologist |
<5% |
60-90% |
60-90% |
Percentage increase for rheumatoid factor |
01:01 |
3-5: 1 |
3-5: 1 |
proportion of HLA-DR4 in relation to the population |
100% |
10% |
10% |
percentage of patients referring to 3-10 years |
They do not require long-term treatment |
Well, but with some progression |
Bad, Progression despite the treatment |
response to the tradlelonal trarmlento of other types |
Rheumatoid factor HLA-DR4 |
Dynamic course on the first 30-180 days |
Dynamic course in the first 30-180 days |
Table 6 Characteristics of patients with polyarthritis who meet criteria for classification for rheumatoid arthritis
Morning Rigz |
Joint morning maturity that lasts at least 1hour |
Arthritis of 3 or more Articular groups |
At least 3 joint groups should beInflammed simultaneously and be objectified by a doctor. The 14 articulatory groups are: proximal interphalangeal, metacarpofalangias, eyelids, knees, ankles and mettarsofalangicas |
Arthritis of jointsof the hands |
At least one articulation of the hands should be inflamedcarpo, metacarpophalangeal, proximal interphalangeal) |
Artrits symmetric |
Simultaneous involvement of the same joint group (defined in criterion 2) on both sides of the body |
Rheumatoid nodules |
Subcutaneous nodes in bone prominences. surface extension or zoning juxta joints observed by a doctor |
Rheumatoid factor serum |
Préncia of high values of factor rheumatoid by any method with a result in controls less than 5% |
Radiological alterations |
Radiological alterations typical of rheumatoid arthritis in posteroanterior radiographs of the hands. Must exist erosion or osteoporosis juxta articulare clear and defined in 'affected joints |
Table 7 Classification criteria for rheumatoid arthritis American College of Rheumatology
Clase funcional |
Definicion |
I |
Complete capacity to perform the usual activities of daily life, including self-care, avocational and vocational activities |
II |
Can perform the usual self-care and avocational activities but with limitations in vocational activities |
Ill |
You can carry out activity activities but you have limitations in the |
IV |
It has limits for carrying out usual activities of self-care avocational and voaciomles. |
Table 8 Criteria reviewed by the American College of Rheumatology for Rheumatoid for the classification of functional status in rheumatoid arthritis
Morning Rigz Joint morning maturity that lasts at least 1hour Arthritis of 3 or more Articular groups At least 3 joint groups should beInflammed simultaneously and be objectified by a doctor. The 14 articulatory groups are: proximal interphalangeal, metacarpofalangias, eyelids, knees, ankles and mettarsofalangicas Arthritis of jointsof the hands At least one articulation of the hands should be inflamedcarpo, metacarpophalangeal, proximal interphalangeal) Artrits symmetric Simultaneous involvement of the same joint group (defined in criterion 2) on both sides of the body Rheumatoid nodules Subcutaneous nodes in bone prominences. surface extension or zoning juxta joints observed by a doctor Rheumatoid factor serum Préncia of high values of factor rheumatoid by any method with a result in controls less than 5% Radiological alterations Radiological alterations typical of rheumatoid arthritis in posteroanterior radiographs of the hands. Must exist erosion or osteoporosis juxta articulare clear and defined in 'affected joints
Scale of HAQ-20 Health Assessment Questionnaire
HAQ-20: Pincus was one of the first to use instruments to obtain quantitative information on the functional capacity of patients with RA. In this way, it was observed that patients with more severe disabilities presented lower long-term survival, demonstrating that functional tests allow the identification of patients with a high risk of progressive disease and increased morbidity and mortality. Disability can and should be measured through questionnaires such as the HAQ-20, which is a comprehensive assessment tool for the health of patients with rheumatoid arthritis and is feasible to use in our environment; because it gathers the basic attributes to be considered a valid instrument: on the other hand, it gives information to the clinician in a practical way.4The HAQ questionnaire ( HealthAssessmentQuestionanarie ) is a self-assessment instrument, easy and fast response, with good reproducibility and internal consistency.It is effective in predicting functional deterioration, work disability, joint surgery and premature mortality.Mood or social support are relevant aspects for the patient and can condition adherence and response to treatment, so it is recommended to consider this aspect to assess the need for additional interventions.
Scale DAS28
The instrument DAS28 (index composed of activity), based on the count of 28 joints, has proven to be a simple, valid, reliable and sensitive tool to change the activity of rheumatoid arthritis.It is recommended to perform a clinical evaluation on a monthly basis, until remission of the disease or a low activity level is reached.
It is important to recognize that the DAS28 instrument has limitations because it excludes 3 joint groups that are 1) hips, which are a valuable marker of poor long-term prognosis;2) ankles, which are affected in more than 50% of cases;and 3) feet, which are affected early, in patients with rheumatoid arthritis.To assess inflammatory activity, it is recommended to count painful and swollen joints, pain assessment, overall evaluation of the disease (by the patient and by the doctor), determination of acute phase reactants and use of activity indices, such as YOU GIVE.The evaluation of the degree of inflammatory activity should be measured at intervals of one to three months, until remission is achieved.Patients must have a formal annual evaluation, in which the activity of the disease is determined investigate extra-joint manifestations, effects of the disease on the quality of life, work status, disability, comorbidities and adverse effects of the drugs.
The subjective assessment of the doctor about the activity of the disease is the clinical criterion most used in daily practice.Its use as an exclusive response criterion is not advisablethe pain must be evaluated by the patient.Its measurement is recommended with a horizontal analogue visual scale of 10 cm, divided into 1 cm segments.The measurements will be accompanied by numerical descriptors from 0 to 10, where 0 will mean "no pain" and 10 "maximum pain".The overall evaluation of the disease should integrate the doctor's point of view and the perspective of the patient.For its measurement it is recommended to use a horizontal analogue scale of 10 cms., divided into 1 cm segments.The measurements will be accompanied by numerical descriptors from 0 to 10, where 0 means "very well" and 10 "very bad".
Semiological maneuver of BAIC
The proposal of the BAIC maneuver aims to assess the musculotendinoarticular force (FMTA) at the level of the hand in rheumatoid arthritis, it consists of asking the patient to pinch the index finger with the thumb posteriorly with each of the fingers successively , when there is inflammation at joint level, it notably limits thestrength of it.At the same time the examiner can assess the power of the same trying to open the clamp (FMTA).Normally an opposition with each and every one of the fingers against the thumb is possible, at the same time evidencing an opposition of the patient when trying to open the clamp (FMTA).In conditions of inflammatory autoimmune activity, the BAIC maneuverit is possible to perform th only with the first or with any of the fingers and there is no opposing force trying to open the clamp.For a better understanding the following classification is proposed:
Baic maneuver classification
Mild: From zero to one affected joint. No difficulty in clamping
Moderate: Two to three affected joints, and moderate difficulty of impingement
Severe:From four to more affected joints, and difficulty in pinching
Diagnosis and early treatment of the disease is essential to reduce the active stage, progression,remission and the associated mortality decrease.The diagnosis of the patients is based on the criteria of classification with the scales;DAS 28 that determine the inflammatory activity with the number of affected joints and the HAQ - 20 that allows us to evaluate the motor activity in the daily life of each of the patients.TOitselfBAIC maneuver will allow us to identify patients who come to consult with rheumatoid arthritis with compromised musculotendinoarticular force (FMTA) having a higher predisposition to mild, moderate, severe disease development.Thus, these patients can benefit from an early, effective treatment, preventing the advance of the progression of joint and systemic damage of the disease.The objective is to determine the efficacy of the clinical activity of rheumatoid arthritis using the DAS28 and HAQ-20 scales in relation to the BAIC maneuver in patients treated in the PAISE N ° 32 during the months of August, September and October of 2017 in the city of Cochabamba.
A Descriptive, Transversal and Prospective study was conducted in 240 patients with Rheumatoid Arthritis who were treated in the PAISE N°32 during the months of August, September and October of 2017; at the time of consultation, the doctor and the patient independently carried out the Painful and inflamed joints and the latter, the global assessment scale (EVG). Later he used the HAQ-20 that allows to evaluate the physical function self-perceived by the patient when carrying out common activities in his daily life, likewise the DAS28 evaluating the number of affected joints in proven cases of Rheumatoid Arthritis and its main scales used for its clinical diagnosis .
We evaluated 240 patients, of which 41 male patients corresponds to 17.08%, and 199 female patients representing 82.91%, who attended the consultation from August to October 2017 (Figure 1), (Figure 2) (Figure 3), (Figure 4), (Figure 5).
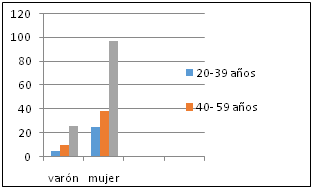
Figure 1 Demographicdata of patients with AR According to the age group, the highest percentage that attend the consultation are older than 60 years with a female 40.41%, and with 2.08% in men between the ages of 20 and 39 years.
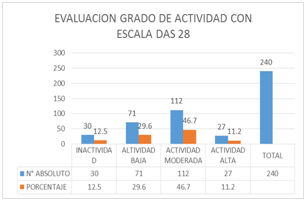
Figure 2 Evaluation degree of activity with scale das28. According to the results obtained with the DAS28 scale, 12.5% are inactive, 29.6% have low activity, 46.7% with moderate activity and 11.2% with high activity.
Figure 3 The results obtained with the HAQ-20 to assess the activity of daily life is that 13.3% have no difficulty, 29.2% with low difficulty, 47.1% with moderate difficulty for daily activities and 10.4% can not perform daily activities.
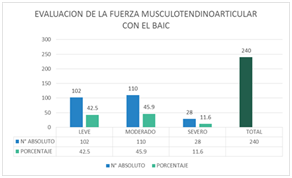
Figure 4 The evaluation of the musculotendinoarticular force (FMTA) was also performed with the BAIC maneuver having the following results: Mild 42.5%, Moderate 45.9% and Severe 11.6%.
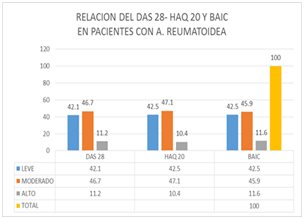
Figure 5 The relationship between the scales of DAS 28 - HAQ 20 and the semiotic maneuver of BAIC, is closely related, in the patients assessed during the three months of study, taking into account each of the results that are shown in each of these scales.
The present study was carried out to analyze the clinical value of the scales DAS28, HAQ-20 and the semiotic maneuver of BAIC.
The instrument DAS2 8 (score of activity of the disease), based on the count of 28 joints, has proved to be a simple, valid, reliable and sensitive tool to change the activity of rheumatoid arthritis. It is recommended to perform a clinical evaluation on a monthly basis, until remission of the disease or a low activity level is reached. It is important to recognize that the DAS28 instrument has limitations because it excludes 3 joint groups that are 1) hips, which are a valuable marker of poor long-term prognosis; 2) ankles, which are affected in more than 50% of cases; and 3) feet, which are affected early, in patients with rheumatoid arthritis.9 To assess inflammatory activity, it is recommended to count painful and swollen joints, pain assessment, global evaluation of the disease (by the patient and by the doctor), determination of acute phase reactants and use of activity indices, such as the DAS.9 The evaluation of the degree of inflammatory activity should be measured at intervals of one to three months, until remission is achieved. Patients must have a formal annual evaluation, in which the activity of the disease is determined, investigate extra-joint manifestations, effects of the disease on the quality of life, work status, disability, comorbidities and adverse effects of the drugs.9 The subjective assessment of the doctor about the activity of the disease is the clinical criterion most used in daily practice. It is not advisable to use it as an exclusive response criterion. The pain must be evaluated by the patient. Its measurement is recommended with a horizontal analogue visual scale of 10 cm, divided into 1 cm segments. The measurements will be accompanied by numerical descriptors from 0 to 10, where 0 will mean "no pain" and 10 "maximum pain". The overall evaluation of the disease should integrate the doctor's point of view and the perspective of the patient. For its measurement it is recommended to use a horizontal analogue scale of 10 cms, divided into 1 cm segments. The measurements will be accompanied by numerical descriptors from 0 to 10, where 0 means "very well" and 10 "very bad". The HAQ questionnaire (Health Assessment Questionanarie) is a self-assessment instrument, quick and easy to answer, with good reproducibility and internal consistency. It is effective in predicting functional deterioration, work disability, joint surgery and premature mortality.9
The semiotic maneuver of BAIC allows us, in a simple way, to identify rheumatoid arthritis and musculotendinoarticular force (FMTA) patients who present a greater predisposition to the mild, moderate and severe development of the disease. Thus, these patients may benefit n of early, effective treatment, preventing the progression of joint damage progression and systemic disease.39–56
Relating the DAS28, the HAQ-20 with the semiotic maneuver of BAIC that we propose, this is an important tool to evaluate the musculotendinoarticular force in patients with rheumatoid arthritis.
None.
Author declares that there are no conflicts of interest.

©2018 Callahuara, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.