MOJ
eISSN: 2574-9722


Research Article Volume 7 Issue 2
1Centro de Ciências da Saúde, Universidade Estadual do Ceará (UECE), Fortaleza, Ceará (CE), Brasil
2Hospital Carlos Alberto Studart Gomes, Fortaleza, Ceará (CE), Brasil
Correspondence: Geanimar Lopes de Andrade Pereira, Centro de Ciências da Saúde, Universidade Estadual do Ceará (UECE), Fortaleza, Ceará (CE), Brasil
Received: April 02, 2022 | Published: April 8, 2022
Citation: Pereira GLA, Almeida GPL, Rocha EMM, et al. Pharmaceutical care in immunosuppressive therapy for heart transplant patients in ceará. MOJ Biol Med. 2022;7(2):52‒59. DOI: 10.15406/mojbm.2022.07.00166
Objective: To assess the impact of adherence to immunosuppressive therapy in association with therapeutical care for heart transplant patients in Ceará.
Method: Randomized clinical study, performed in a public hospital in the state of Ceará, which verified the adherence to treatment through self-report, BAASIS scale (Basel Assessment of Adherence Scale for Immunosuppressives) and measurement of serum levels of immunosuppressants. In the statistical analysis, the Kolmogorov-Smirnov normality test for numerical variable, the Qui-square test for categorical variable and the Mantel-Haenszel test to verify the association of variables in stratified analysis were applied. Significant value of p < 0.05 was considered. Initially, 202 patients were recruited according to eligible criteria, which 101 patients were randomized. 91 patients concluded the study, 45 in Control Group (CG) and 46 in Intervention Group (IG).
Results and discussion: The mean ageof heart transplant of CG was 53 (standard deviation, SD±12), and in IG, the mean was 54 years (SD±10). Most participants were male in both groups. The etiology that more led patients for heart transplantation in both groups (CG and IG) was ischemic cardiomyopathy (CM). Rejection episodes were found in CG (n=15, 33.3%) and IG (n =12, 26.1%) participants. The measure of adherence to immunosuppressantsusing the BAASIS scale presented that, at the beginning of the search, 23 patients in the CG (51.1%) and 24 in the IG (52.2%) did not adhere to the treatment. At the end of the search, greater adherence to the immunosuppressive treatment was observed in patients in the IG (89.1%), against 68.1% in patients in the CG, p=0.003. In the assessment of adherence to immunosuppressants through blood levels, the valued obtained at the beginning indicated that the groups showed differences; at the end of the search, the groups remained distinct.
Conclusion: Patients who received pharmaceutical accompaniment presented greater adherence to immunosuppressants when compared to the control group (p=0.003), when measured by self-report. Therefore, the pharmaceutical cares oriented by intervention and strategies were capable to optimize the adherence to immunosuppressive therapy in heart transplant patients.
Keywords: pharmaceutical attention, adherence to medicament, heart transplantation
Heart transplantation (HT) is the gold standard surgical procedure in the treatment of advanced heart failure (HF) refractory to drug therapy. It is indicated when there is great limitation of functional capacity and low survival expectancy. The procedure requires the care of a multidisciplinary team, with specific skills to offer individualized assistance.1,2
Pharmaceutical care (ATENFAR) aims at patient education and counseling, drug therapy review and outcome monitoring. Adherence to treatment is essential and reflects the degree of correspondence between the patient's behavior and the prescription of health professionals, and encompasses pharmacological and behavioral measures.3
The use of immunosuppressive therapy is sinequa non for the success of the transplant, as it minimizes the occurrence of graft rejection. However, adherence to the therapeutic regimen is sometimes insufficient.4,5 Particularly, the functions performed by the pharmacist can prevent adverse treatment-related events, minimizing treatment interruptions.5
On the other hand, non-adherence has been described as deviation from the therapeutic regimen to a sufficient degree to adversely impact outcomes.6 The lack of adherence can occur, for example, when it has not yet been assimilated by the patient that the transplant is a treatment and not a cure. Thus, the patient is subject to the risk of graft dysfunction due to lack of medication adherence.1,7
This research aimed to evaluate the impact of adherence to immunosuppressive therapy in association with pharmaceutical care in heart transplant patients in the State of Ceará, Brazil (BR).
A randomized clinical trial was conducted, where participants were randomly allocated to the Control Group (CG) or Intervention Group (IG), which received pharmaceutical follow-up guided by interventions and strategies. The population consisted of adult heart transplant patients in outpatient follow-up at the Carlos Alberto Studart Gomes Hospital, in Fortaleza, Ceará.
Through the sample size calculation, a sample of 86 heart transplant patients was considered, 43 for the CG and 43 for the IG, with a significance level of 5% and power of the single-tail test of 80% to detect a difference of 51%, based on baseline adherence to immunosuppressants. For the study, 202 patients were eligible, after application of the inclusion and exclusion criteria, 101 patients (total sample) were selected for the study who were randomized and allocated to the GC and GI groups.
In the CG, 50 heart transplant recipients were allocated, of which 2 refused to participate, 1 was not contacted, and 2 were excluded due to lack of exams. The IG initially had 51 heart transplant recipients, of which 2 refused to participate, 1 transplant patient died during the research and 2patients were lost to follow-up. The data collection period was from November/2018 to July/2019. Patients over 18years of age, with three months of heart transplantation at the maximum time of transplantation, were excluded, those unable to attend pharmaceutical consultations and without test results were excluded.
The research was approved by the Hospital Ethics Committee and submitted to Plataforma Brasil (No. 2,985,781). After clarifying the objectives of the study, the participants signed the Free and Informed Consent Term, guaranteeing them the right to privacy and the freedom to withdraw from the research at any time.
The BAASIS scale was used, which was applied at baseline (initial) and at the end of the research. The tool consists of four questions focused on the use of immunosuppressive medication in the last four weeks.6,8 Results are categorized into YES or NO, whenever an answer is yes, a score is given according to frequency.
The study also evaluated blood concentrations of calcineurin inhibitors (Tacrolimus and Ciclosporin) and mTor inhibitors (Sirolimus and Everolimus). The cutoff point for this variable consisted of the first sample collected at baseline, for both groups. For the final collection of the CG group, the sample from the third month after its inclusion in the study was used. In the IG, the sample was collected after the third pharmaceutical follow-up. To obtain data, the patients' medical records and the computerized information system used by the institution (MATRIX) were used.
The immunosuppressive therapy for maintenance of heart transplant patients monitored by the Hospital where the research was carried out is defined by the second Brazilian Guideline on Cardiac Transplantation. The immunosuppressive regimen consists of corticosteroids, calcineurin inhibitors (cyclosporine or tacrolimus) and an antiproliferative (sodium mofetiloucophenolate mycophenolate). Drug standardization is described in Table 1.
Fármaco |
Via |
Dose inicial |
Manutenção |
Nível sérico |
Prednisona |
Oral |
1mg/kg. |
Retirada em 6meses |
Não se aplica |
Metilprednisolona |
Intra-venosa |
500 - 1000mg, dose decrescente até terceiro PO |
Tratamento de rejeição aguda por 3-5dias |
Não se aplica |
Ciclosporina |
Oral |
3-8mg/kg/dia; |
Guiada por sintomas, rejeição e nível sérico |
C0: 350-450 (inicial); 250-350 (3 a 6meses); 200-300 (6 a 12meses); Venosa 100-200 (acima de 1 ano) |
Venosa |
1-2mg/kg/dia; (1/3dose oral) |
|||
Tacrolimus |
Oral |
0,05-0,1mg/kg/dia; |
Guiada por sintomas, rejeição e nível sérico |
Vale: 10-15ng/mL (inicial); 5–10 ng/mL (pós 6meses) |
Venosa |
0,01-0,02mg/kg/dia |
|||
MicofenolatoMofetil |
Oral |
1 g 12/12horas |
500-1,5g 12/12horas |
MPA 2,5-5mcg/ml |
Venosa |
Semelhante a oral |
|||
Micofenolato Sódico |
Oral |
720mg 12/12horas |
360-1080g 12/12horas |
MPA 2,5-5mcg/ml |
Sirolimus |
Oral |
Ataque de 6mg |
2mg/dia - 1x/dia (ajuste por nível sérico) |
Vale: 5-15ng/ml |
Everolimus |
Oral |
0,5-1,5mg/dia |
0,5-1,5mg/dia - 12/12horas |
Vale: 3-8ng/ml |
Table 1 Standardization of immunosuppressive drugs adopted by the Heart Failure and Transplantation Unit (CICU). (In Portuguese)
C0: Serum concentration of the immunosuppressant in the valley (1hour before the next dose)
MPA: Mycophenolate acid
PO: Postoperative
Source: Adapted from the II Heart Transplant Guideline, 2010
The IG patients were monitored monthly by the research pharmacist for three months and combined interventions were performed that included the characteristics of categories I, II and III, as shown in Table 2.
Interventions |
Strategies |
(I) informative |
Cognitive/Educational |
Telephone (Call/message) monthly |
|
Group didactic classes with slides monthly |
|
(II) Behavioral |
Behavioral |
Adaptation of daily routine to therapeutic treatment. |
|
(III) Family/Social |
Social support |
Table 2 Strategies to optimize patients' therapeutic adherence to immunosuppressants in the intervention group
The data obtained in the collection were tabulated and analyzed using the IBM SPSS Statistics for Windows, Version 23.0 software. Armonk, NY: IBM Corp. IBM Corp. Released 2015. The categorical quantitative results were presented in the form of percentages and counts and the numerical ones in the form of measures of central tendency. Kolmogorov-Smirnov normality tests were performed for continuous variables. For categorical variables, the chi-square test was used to verify association and the Mantel-Haesnzel test for stratified analysis with 3 variables (intervention). P values <0.05 were considered significant.
The results corresponding to the clinical data of heart transplant patients followed up in the research are presented in (Table 3). The mean age of heart transplant recipients in the CG was 53 years±12 and for the IG 54 (SD±10) years. Most participants were male in both groups. The main etiology that most led patients to heart transplantation in both groups (CG - IG) was ischemic MCP.In the CG, the second determining cause of heart transplantation was Chagas' MCP n=11 (24.4%) followed by idiopathic MCP n=8 (17.8%). In the GI, there was a higher percentage of heart transplant patients due to idiopathic MCP n=11 (23.9%) and a lower percentage of patients with Chagas' MCP n=7 (15.2%). The mean time of heart transplantation in the CG was 72 months (SD±58) and 84 months (SD±64) in the IG.
Etiologia do Transplante n (%) |
GC |
GI |
Grupo Geral |
P |
MCP-Isquêmica |
15(33) |
12(26,1) |
27(29,6) |
0,579** |
MCP-Idiopática |
8(17,8) |
11(23,9) |
19(20,9) |
|
MCP- Chagásica |
11(24,4 |
7(15,2) |
18(19,8) |
|
MCP-Dilatada |
3(6,70) |
6(13,0) |
9(9,90) |
|
MCP-Orovalvar |
5(11,1) |
4(8,70) |
9(9,90) |
|
MCP-Outros3 |
3(6,7%) |
6(13) |
9(9,90) |
|
Tempo de transplante em meses, média (DP) |
72±58 |
84±64 |
78±61 |
0,261 |
Rejeição n (%) |
||||
Sim |
15(33,3 |
12(26,1) |
27(29,7) |
0,449 |
Não |
30(66,7 |
34(73,9) |
64(70,3) |
|
Imunossupressores n (%) |
||||
Tacrolimus |
23(51,1 |
21(45,7) |
44(48,4) |
|
Ciclosporina |
14(31,1 |
12(26,1) |
26(28,6) |
|
Sirolimus |
4(8,9) |
8(17,4) |
12(13,2) |
0,592*** |
Everolimus |
4(8,9) |
3(6,5) |
7(7,7) |
|
Tacrolimus/ Sirolimus |
0(0) |
1(2,2) |
1(,1,1) |
|
Tacrolimus/ Everolimus |
0(0) |
1(2,2) |
1(1,1) |
|
Table 3 Clinical characteristics of heart transplant patients. (In Portuguese)
Continuous variables are expressed as mean and standard deviation; categorical, in the form of n (%) **includes cell with less than 5 individuals; *** includes cells with less than 1 and 5 individuals; 3MCP - hypertrophic, viral and peripartum; MCP (Myocardiopathy); GC (Control Group); GI (Intervention Group); SD (Standard Deviation), p< 0.05, n (number of patients)
In the total sample GC and GI, composed of 91 heart transplant recipients, at some time during treatment, 27 patients (29.7%) had already had an episode of rejection with no statistically significant value (Table 3).
The characterization of the heart transplant recipient's adherence to immunosuppressive drugs, performed in the baseline period immediately after inclusion in the research and in the final period, through the items of the BAASIS scale were gathered in (Table 4). At baseline, both groups (CG/IG) were similar. The results show that 23 (51.1%) of the heart transplant recipients from the CG and 24 (52.2%) from the IG did not adhere to one or more than one of the four items evaluated, at least once in the last four weeks. Among the questions measured by the BAASIS scale, the non-adherence of heart transplant patients has a higher percentage when the question refers to the lack of fidelity to the prescribed medication times, n=17 (37.8%) in the CG and n=19 (41.3 %) in the IG. In the final period, the values decrease to n=7 (15.6%) in the GC and n=3 (6.5%) in the IG (Table 4).
BASAL |
GC |
GI |
Geral Group |
*p |
Adherent |
22(48,9) |
22(47,8) |
44(48,3) |
0,919 |
Noadherent |
23(51,1) |
24(52,2) |
47(51,7) |
|
Q1. Do you remember not taking your immunosuppressant medications in the last 4 weeks? |
||||
No |
33(73,3) |
37(80,4) |
70(76,8) |
0,421 |
Yes |
12(26,7) |
9(19,6) |
21(23,2) |
|
Q2.You have missed several consecutive doses of your immunosuppressant drugs in the last 4 weeks? |
||||
No |
42(93,3) |
41(89,1) |
83(91,2) |
|
Yes |
3(6,7) |
5(10,9) |
8(8,8) |
0,479** |
Q3. Do you remember taking your immunosuppressant medications more than 2 hours apart from the prescribed time in the last 4 hours? |
||||
No |
28(62,2) |
27(58,7) |
55(60,4) |
0,731 |
Yes |
17(37,8) |
19(41,3) |
36(39,6) |
|
Q4.You have taken a dose lower than the dose prescribed by your doctor in the last 4 weeks? |
||||
No |
40(88,9) |
40(87,0) |
80(87,9) |
0,777 |
Yes |
5(11,1) |
6(13,0) |
11(12,1) |
|
FINAL |
GC |
GI |
Grupo Total |
*p |
Adherent |
31(68,9) |
41(89,1) |
72(79) |
0,018* |
No adherent |
14(31,1) |
5(10,9) |
19(21) |
|
Q1. Do you remember not taking your immunosuppressant medications in the last 4 weeks?? |
||||
No |
39(86,7) |
45(97,8) |
84(92,3) |
0,046** |
Yes |
6(13,3) |
1(2,2) |
7(7,7) |
|
Q2.Have you missed several consecutive doses of your immunosuppressive drugs in the last 4 weeks? |
||||
No |
44(97,8) |
46(100,0) |
90(99,8) |
0,309*** |
Yes |
1(2,2) |
0(0) |
1(2,2) |
|
Q3. Do you remember taking your immunosuppressive drugs more than 2 hours apart from the prescribed time, in the last 4 hours? |
||||
No |
38(84,4) |
43(93,5) |
81(88,9) |
0,168** |
Yes |
7(15,6) |
3(6,5) |
10(11,1) |
|
Q4.You have taken a dose lower than the dose prescribed by your doctor in the last 4 weeks? |
||||
No |
40(88,9) |
45(97,8) |
85(93,3) |
0,086** |
Yes |
5(11,1) |
1(2,2) |
6(6,7) |
|
Table 4 Characterization of adherence (GC – GI) to immunosuppressive drugs in heart transplant patients using the BAASIS scale
*p < 0.05; **includes cell with less than 5 individuals; *** includes cells with less than 1 and 5 individuals; BASAL (initial research period); FINAL (final period of the research). Q1 (Question 1); Q2 (Question 2); Q3 (Question 3); Q4 (Question 4)
Figure 1 shows the characterization of heart transplant patients after the responses attributed to the BAASIS scale at baseline, characterizing adherence and non-adherence to immunosuppressive drugs. In the CG, 22 patients (48.9%) were adherent to immunosuppressive therapy, while in the IG the result was n=22 (47.8%). The two groups (CG/IG) showed no statistical difference between them (p= 0.919) at baseline.
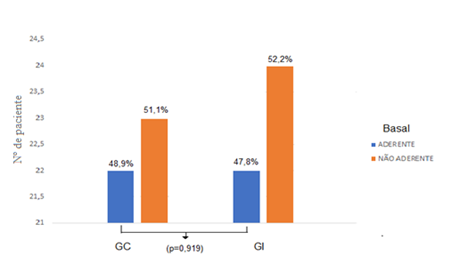
Figure 1 Characterization of adherence to immunosuppressants in heart transplant recipients, GC - GI, at baseline using the BAASIS scale GC: control group; IG: intervention group (In Portuguese).
Figure 2 shows the result measured using the BAASIS scale, at the end of the survey. For the GC group the adherence was n=31 (68.9%) and for the GI the adherence was of (89.1%) corresponding to 41 heart transplant patients, there is a significant increase in the percentage of adherence to immunosuppressants (p= 0.010).
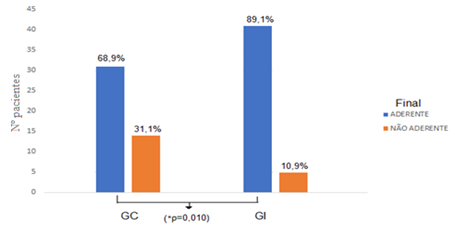
Figure 2 Characterization of adherence to immunosuppressants in heart transplant recipients, GC - GI, in the final period using the BAASIS scale GC: control group; IG: intervention group (In Portuguese).
Figure 3 shows the changes observed by the BAASIS scale, at the end of the research, among adherent heart transplant patients for the two groups, GC and GI. In the CG, there was an increase in the adherence of heart transplant recipients to immunosuppressants of n=9 (20%), even without pharmaceutical follow-up, however this improvement was not significant (p=0.543). Analyzing the GI in the same period, after the pharmaceutical follow-up, there is an increase in the rate of heart transplant patients adhering to immunosuppressive therapy from (47.8%) to (89.1%), which corresponds to an increase of 19patients, with statistical significance(p=0.003).
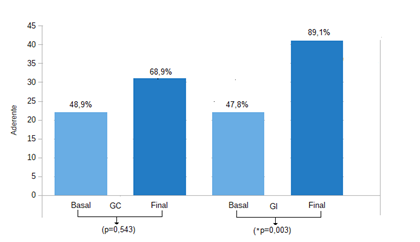
Figure 3 Characterization of heart transplant recipients adherent to immunosuppressants by the BAASIS scale in the GC - GI in the baseline and final periods. CG: Control group; IG: Intervention group (In Portuguese).
The assessment of blood levels of immunosuppressants was the other method that the study used as a reference to measure adherence to therapy. Samples were collected at baseline and at the end of the research.
Table 5. shows that, at baseline, the groups showed differences with p=0.043. The CG had 23 (51.1%) and the GI had 33 (71.7%), patients with normal blood levels of immunosuppressive drugs. At the end of the study, the GC increased in 3 patients with the rate of blood levels of immunosuppressants out of range (6.7%), while the GI showed a slight increase in the number of patients with normal blood level n=1 (2 ,two%). These results showed that the groups remained different and the statistical analysis did not allow inferences about follow-up. Both groups were similar regarding the immunosuppressive therapy prescribed. Tacrolimus stood out as the most prescribed calcineurin inhibitor (Table 5).
PERÍODO BASAL |
|
|
|
|
|
BASAL |
GC n (%) |
GI n (%) |
TOTAL n (%) |
*p |
|
Normal 1 |
23(51,1) |
33(71,7) |
56(61,4) |
||
Fora de Faixa |
22(48,9) |
13(28,3) |
35(38,6) |
0,043* |
|
IMUNOSSUPRESSORES n (%) |
|||||
Tacrolimus |
23(51,1) |
23(50,0) |
46(50,6) |
||
Ciclosporina |
14(31,1) |
11(23,9) |
25(27,5) |
||
Sirolimus |
4(8,9) |
8(17,4) |
12(13,1) |
0,647*** |
|
Everolimus |
4(8,9) |
4(8,7) |
8(8,80) |
||
PERÍODO FINAL |
|||||
FINAL |
GC |
GI |
TOTAL |
*p |
|
Normal |
20(44,4) |
34(73,9) |
54(59,2) |
||
Fora de Faixa |
25(55,6) |
12(26,1) |
37(40,9) |
0,004* |
|
IMUNOSSUPRESSORES n (%) |
|||||
Tacrolimus |
24(53,3) |
23(50,0) |
47(51,7) |
||
Ciclosporina |
14(31,1) |
12(26,1) |
26(28,6) |
||
Sirolimus |
3(6,7) |
8(17,4) |
11(12,0) |
0,461** |
|
Everolimus |
4(8,9) |
3(6,50) |
7(7,70) |
|
|
Table 5 Assessment of adherence to immunosuppressants in heart transplant recipients using the right method and the list of immunosuppressants prescribed in the baseline and final period (In Portuguese)
*p < 0,05; the reference values are found in table 1; **Includes cells with less than 5 individuals ***Includes cells with less than 1 and 5 individuals
Interventions |
Strategies |
n (%) |
Informativas |
Face-to-face Cognitive/Educational |
46 (100) |
Phone call and messages. |
44 (96) |
|
Group didactic classes with slides. |
18 (39) |
|
Behavioral |
alarm reminder |
40 (87) |
Someone's help to remember. |
4 (9) |
|
Adaptation of daily routine to therapeutic treatment. |
41 (89) |
|
Family/Social |
Social support by the family member/caregiver. |
27 (59) |
Table 6 Adherence to interventions and strategies in the IG (n=46)
During the three-month follow-up of patients in the intervention group, the pharmacist (researcher) adapted and implemented interventions and strategies that optimized adherence to immunosuppressive therapy by self-report at the end of the research. Interventions and strategies are presented below:
(I) Informational Interventions
All patients in IG n=46 (100%) were treated with the face-to-face cognitive educational strategy. In each pharmaceutical service, the patient was informed about the importance of adherence to drug treatment and pharmacotherapy. These meetings lasted an average of 50 minutes. Of these patients, 44 (96%) received monthly calls and messages via the mobile application (WhatsApp), but two (4%) participants were not included in this strategy, as they live far away, with difficulties in accessing communication. Also in this intervention, group didactic classes were given monthly, with slideshows, and n=18 (39%) were willing to participate, the others justified their absences, due to work activities, others due to home distance.
(II) Behavioral Interventions
Forty patients in the intervention group (87%) started to adopt the alarm reminder on their cell phones and four (9%) started to receive help to remember the time of administration of the medication. Also in this intervention, an adaptation of the daily routine to the drug treatment of heart transplant patients was elaborated and applied, which was accepted by 41 patients (89%).
(III) Family/Social
In this strategy, the participation of 27 companions (59%) who interacted throughout the research was obtained. The others claimed the lack of support in the follow-ups, due to the work activities of their family members and others did not have caregivers.
Assessment of adherence to immunosuppressive therapy in heart transplant recipients by self-report (BAASIS)
This is the first randomized clinical trial conducted in Brazil that evaluated adherence to immunosuppressive therapy in heart transplant recipients by BAASIS self-report. The results show that the interventions and strategies applied with pharmaceutical care increased therapeutic adherence to immunosuppressive treatment, measured by self-report.
The literature shows that it is possible to achieve great benefits in immunosuppressive adherence, through simple interventions, as long as it is conducted to a non-adherent population and adapted to the specific reasons of each patient. Alloway et al. and Klein et al. report that the implementation of informative/educational, behavioral and social interventions, when skillfully performed, become useful tools in combating the numerous factors that influence patients' non-adherence to therapeutic treatments.7,9,10
During the current research, adaptation and implementation of combined interventions for heart transplant recipients who were part of the IG were easy to conduct and agile enough to be included in daily practice in order to optimize therapeutic adherence, in accordance with the literature.
The improvement in adherence evidenced in the present study is consistent with the results presented in other studies. In the clinical trial by Gnatta et al., the impact of pharmaceutical care on adherence to immunosuppressive treatment in kidney transplant recipients was also evaluated through the methods of measuring self-report and blood levels of immunosuppressants. They concluded that the participation of the pharmacist was timely and important, increasing in addition to adherence to safety in the conduct of drug treatment.11
Chisholm et al., concluded results that also value the role of pharmacists aimed at interventions that optimize adherence, becoming fundamental in the drug treatment of transplant patients. Similar findings were demonstrated in a randomized clinical trial that evaluated immunosuppressive adherence by the Medication Event Monitoring System® (MEMS). At the end of the survey after the six-month follow-up, the follow-up group showed a significant improvement in adherence when compared to the control group. The authors justify the results by planning and implementing several stages of interventions according to the needs of the group being monitored.12,13
There is a need for educational interventions to be practiced continuously in the transplanted population, given that the literature presents weaknesses in some situations of therapeutic treatment that begin in the pre-transplantation with the lack of guidance on pharmacotherapy and persist in the post-transplantation period. Therefore, transplant centers that do not provide proper support to receive and prepare the patient for a new lifestyle and still have failures in communication between patients and health professionals can negatively interfere with adherence to pharmacotherapeutic treatment.11,14
The present study showed, as a result of the BAASIS scale in the baseline period for both groups (CG and GI), the occurrence of non-adherence of heart transplant recipients in the research, with a delay of more than 2 hours in the use of immunosuppressants the main item reported. Forgetfulness was the main reason alleged for non-compliance. Similar data were presented by Oliveira et al., who evaluated adherence to immunosuppressants with the same instrument, indicating a rate of 49% of non-adherents and the same reason for non-compliance with drug prescriptions.15
Failure to comply with immunosuppressive regimen schedules is frequently demonstrated in studies that assess adherence, with delays of 1.5hours and 2hours. The fact is that the literature proves that attitudes that produce delays in the administration of doses can change the dosages of immunosuppressants in the blood. Small failures in adherence to the immunosuppressive regimen result in damage to the health of the organ.16-20
It is worth mentioning that the CG for which there was no pharmaceutical care provided also showed a gain in adherence to immunosuppressive therapy. The researchers assume that this finding, although not statistically significant, was influenced by the close contact that the two groups had with each other, as the discovery of the information generated new learning that they themselves started to disseminate, making the information offered to the IG participants, to be shared with CG participants.
Assessment of adherence to immunosuppressive therapy in heart transplant recipients by concentration in blood levels of immunosuppressants
The values obtained in the analysis of blood levels of immunosuppressive drugs in the sample at baseline reveal a difference between the CG, which presented with only 51.1% of heart transplant patients with normal values, while for the IG more than 70% of heart transplant patients had immunosuppressant concentrations in the normal range with a statistically significant difference even before receiving pharmaceutical care, at the end of the research the number of heart transplant patients in the CG who had blood levels outside the normal range increased, while in the IG there was a small improvement in percentage.
The results achieved with similar studies corroborate those of this research, such as the group by Klein et al. which showed the impact of pharmaceutical care, during 12months, on adherence to immunosuppressants in transplant patients, with the intervention group more likely to achieve desirable blood levels. In the study presented by Corrêa et al., in patients undergoing allogeneic hematopoietic stem cell transplants after pharmaceutical follow-up for six months, the data indicated that the control group obtained 65% of the levels considered within the range, vs the intervention group 82%.10,21
In the research by Gnatta et al.11, a different finding is observed, in the measurement of tacrolimus dosage, the result showed that in the first measurement of the blood level there was a significant difference for the group under follow-up. However, during the research, the other collections did not show significant differences.
In view of these results, it is confirmed what the literature says that keeping the blood levels of immunosuppressive drugs in the proper range is an arduous task, as several factors can influence the impairment of this activity. Genetic factors can affect the serum concentration of calcineurin inhibitors, whereas physiological factors, such as variation in renal function, can modify the serum concentration of tacrolimus. Corrêa et al., also highlights drug interactions and incorrect use of drugs, such as tacrolimus, which may have its absorption compromised by concomitant ingestion with food.21,22
The task of controlling blood levels of drugs at desirable values is challenging, however it is known that to achieve this effect it is necessary to keep them within a narrow therapeutic window. On the other hand, if the levels are above the expected range, they can cause intoxication, leaving the patient vulnerable to risk.21
Faced with the challenges presented in the pharmacotherapy of transplanted patients and witnessed in this research, the presence of the pharmaceutical professional acting in the follow-up of the pharmacotherapy is deemed necessary, developing actions, which are conceptualized as interventions or pharmaceutical recommendations. This professional act aims to solve or prevent unfavorable clinical outcomes, arising from the use of medications, and non-adherence.23
Some limitations presented by the research may have interfered with a better outcome. The study was not blinded, exposing the applicability of the interventions in the IG. During the research, it was observed that patients in both groups were close, which led to the sharing of information between the IG and the CG. Oliveira Filho et al. suggest that in clinical trials patients should be blinded to the intervention used for practical purposes and avoid bias in the results. However, authors state that blinding in some cases becomes difficult or even impossible for some technical reasons, for example: in some types of interventions, including educational ones, a resource used by the present research. Another limitation of the study was not having performed the screening to select the population of non-adherents, due to the small size of the sample. They suppose that this reason may have compromised the measurement of blood levels, showing that the groups were different at the beginning of the research, while they should have been homogeneous as suggested in the literature.13,24,25
The research time limitation for pharmaceutical follow-up was small. Perhaps, it also influenced the outcomes of blood levels of immunosuppressants to promote a desired outcome. Studies that assess adherence show positive results with at least 6 months of follow-up, which may vary up to 2years.26,27
There is still a lack of randomized clinical trials that assess medication adherence in heart transplant recipients, weakening the discussions. The clinical relevance of this study showed an increase in the rate of adherence to immunosuppressive therapy through self-report. The finding represents future changes in adherence to drug therapy in heart transplant patients, given that non-adherence is related to unfavorable clinical outcomes. It is believed that transplant centers can support the introduction of pharmaceutical care with a focus on reducing the rates of non-adherence to drug therapy treatment in heart transplant recipients.28-30
This study reached its objective to the extent that it fulfilled the presented result, in the goal defined by the methodological course of the research, based on data collection and represented by the elaboration of the Master's dissertation in Transplantation. The present study showed that heart transplant recipients who received pharmaceutical care guided by interventions and strategies (informative, behavioral and social/family) showed a significant improvement in adherence to immunosuppressive therapy assessed through self-report, when compared to patients in the control group who did not have pharmaceutical follow-up. Therefore, pharmaceutical care was able to optimize adherence to immunosuppressive therapy in heart transplant patients. Despite the encouraging results achieved in this research, further studies are needed to explore adherence to immunosuppressive therapy in the heart transplant population.
None.
The authors declared no have conflict interest for the study.

©2022 Pereira, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.