MOJ
eISSN: 2574-9722


Case Report Volume 9 Issue 2
1Department of Ophthalmology, National Children’s Hospital, San Jose, Iberoamerican University, San Jose, Costa Rica
2Department of Ophthalmology, National Children’s Hospital, San Jose, Costa Rica, University of Costa Rica, San Jose, Costa Rica
3Department of Ophthalmology, Peset Hospital, Valencia, Spain
Correspondence: Leslie Arguello Cruz, Department of Ophthalmology, National Children’s Hospital, San Jose, Costa Rica, University of Costa Rica, San Jose, Costa Rica
Received: March 14, 2024 | Published: April 1, 2024
Citation: Lezama LV, Cruz LA, Pérez AC, et al. Ophthalmic Zika virus disease: ocular findings in two Costa Rican newborns with microcephaly render a new insight of the illness. MOJ Biol Med. 2024;9(2):39-40. DOI: 10.15406/mojbm.2024.09.00215
Zika virus infection is a vectorial tropical illness which has only recently been reported in Costa Rica. Inoculation by this flavivirus can cause a mild fever and rash in the general population. However, when contracted by pregnant women it may result in severe brain abnormalities and cognitive impairment of the newborn. We present the first two reported cases of combined microcephaly with retinopathy presumably due to this congenital viral infection. The ocular findings in both infants consisted in extensive chorioretinal atrophy and pigmented mottling throughout the macula. Despite both newborn turning in a positive result for Zika virus, only one of the mothers reported flu-like symptoms during pregnancy. We must consider the great threat this disease may pose on our health system since it generates a profound disability in the infant and will be therefore associated with long-term healthcare costs.
Keywords: Zika virus, microcephaly, newborn, serum
The first child in our report is a male infant who was born to parents living in the pacific central coast of Costa Rica, with access to all the basic services (running water, electricity, etc.). During the first trimester his mother went to a local health clinic afflicted with fever, malaise, headache and a non-pruritic rash. At that time, she had a normal complete blood count and negative serum testing for dengue virus, Zika virus and Chikungunya virus. She was treated symptomatically and the illness resolved shortly after. Aside this episode there was no other significant medical history found. The patient attended eleven prenatal care visits where all ultrasounds were normal. Nevertheless, she was diagnosed with severe oligohydramnios at 36 weeks of gestation. The child was delivered at 37 weeks gestational age without complications, with a birth weight of 1775 grams, a length of 44 cm, and a head circumference of 24 cm. The Apgar score was 6 at 1 minute after birth and 9 at 5 minutes after birth.
This newborn was referred to the Hospital Nacional de Niños in San José, Costa Rica, where a full evaluation was performed at the age of 28 days. Cranial ultrasound revealed brain hypotrophy with lissencephaly. Serum tests, including polymerase chain reaction (PCR) for the detection of TORCH infections were all negative as opposed to the Zika virus test which came out positive. Upon ophthalmic evaluation, he demonstrated no ocular pursuit. Anterior segment biomicroscopy was unremarkable. Fundoscopic exam revealed bilateral optic nerve hypoplasia and extensive chorioretinal atrophy with pigmentary mottling throughout the macula in both eyes (Figure 1).
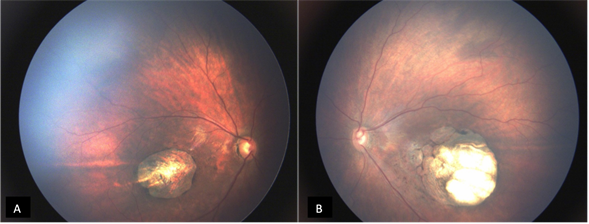
Figure 1 Patient 1. Funduscopic exam of right (A) and left (B) eyes reveals extensive chorioretinal atrophy and pigmentary mottling in both maculae. Bilateral optic nerve hypoplasia can also be observed.
A similar case to the one described was reported weeks after. This newborn’s family lived in a rural area of Costa Rica, with access to basic health services. The mother attended six prenatal care appointments and had one ultrasound in the first trimester, which was normal. Her past medical history was unremarkable, and she had no viral symptoms during pregnancy. The infant was born by vaginal delivery at 38 weeks gestational age, with no complications. She had a birth weight of 3205 grams, a length of 52 cm, and a head circumference of 29.5 cm which led to the diagnosis of microcephaly. The Apgar score was 7 at 1 minute after birth and 9 at 5 minutes after birth. Ophthalmic evaluation in her second live day revealed no anterior segment anomalies. Upon fundoscopic examination, she was found to have optic nerve hypoplasia with foveal, parafoveal, and peripheral pigmentation in both eyes. All serum tests, including those for TORCH infections, were negative. Testing for vector-borne diseases was then considered, which gave a positive result for Zika virus (Figure 2).
Zika virus disease is caused by a flavivirus, transmitted primarily by mosquitoes in the Aedes genus. The incubation period (time from exposure to symptoms) of Zika virus disease is not clear, but is thought to be a few days. The symptoms are similar to other arbovirus infections like dengue, and include fever, rash, conjunctivitis, muscle and joint pain, malaise and headache. These symptoms are usually mild and last for around two to seven days. In contrast, Zika virus infection during pregnancy can cause severe congenital brain abnormalities (including microcephaly) and can even trigger Guillain-Barré syndrome. Intense efforts are ongoing to investigate the link between Zika virus and a range of neurological disorders, within a rigorous research framework.
Zika virus transmission mainly occurs through the bite of an infected Aedes aegypti mosquito in tropical regions. Sexual transmission of Zika virus is also possible and other modes of transmission such as blood transfusion are being investigated. Infection with Zika virus may be suspected based on symptoms and recent history of travel (e.g., residence in or travel to an area with active Zika virus transmission). The diagnosis of Zika virus infection can only be confirmed through laboratory tests on blood or other body fluids such as urine, saliva or semen. Treatment is symptomatic.1
In a recent case series, Belfort et al. described 29 infants with microcephaly and a presumed diagnosis of congenital Zika virus infection. Ocular abnormalities were present in 17 eyes, with pigment mottling and chorioretinal atrophy.2 Ventura et al. described similar ocular findings in their report of ten infants clinically diagnosed with Zika virus-related microcephaly.3 As of 2016, the Costa Rican Ministry of health reported 150 cases of Zika virus infection in pregnant women, with spontaneous abortion as the only identified complication (occurring in 3% of cases).4
Aside from the neurological lesions thoroughly described in scientific literature, these new reports revealing Zika-related severe ocular manifestations cast a new shadow over the illness. The comorbidity of a decreased visual acuity will certainly plummet the patients’ living standards, further hindering their chances at having an ordinary life. Moreover, the urge to minimize the long-term costs in healthcare related to this disease exerts pressure on organizations and governments to take action. Prenatal counseling and education are essential for reducing the incidence of Zika virus syndrome, whereas vector control measures are the mainstay of prevention in endemic zones. Ultimately, a larger research effort is needed in order to develop an effective vaccine that could redefine the future of afflicted patients.
None.
The authors declare that there is no conflict of interest.
None.

©2024 Lezama, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.