MOJ
eISSN: 2574-9722


Case Report Volume 8 Issue 2
1Department of medicine, Professor adjunct of cardiovascular surgery, Professor of the Undergraduate Medicine Course and the Stricto Sensu Postgraduate Course-FAMERP and CNPq, Brazil
2Department of medicine, student of medicine school of Sao Jose do Rio Preto-FAMERP-Brazil
3Physician,Vascular surgery resident in medicine school of Sao Jose do Rio Preto-FAMERP/FUNFARME-Brazil
4Professor of Vascular Surgery Discipline in Medicine School in Sao Jose do Rio Preto-FAMERP / FUNFARME, Brazil
Correspondence: Jose Maria Pereira de Godoy, Department of medicine, Professor adjunct of cardiovascular surgery, Professor of the Undergraduate Medicine Course and the Stricto Sensu Postgraduate Course-FAMERP and CNPq, Brazil
Received: April 25, 2023 | Published: May 24, 2023
Citation: de Godoy JMP, de Lima LS,Castellari LMM, et al. Endovascular treatment of ruptured dorsal pancreatic artery pseudoaneurysm: case report. MOJ Biol Med. 2023;8(2):63-65. DOI: 10.15406/mojbm.2023.08.00186
The objective of the present study is to report the technical success of the endovascular procedure in the treatment of pseudoaneurysm of the dorsal pancreatic artery. A 60-year-old white male patient came to the emergency room, complaining of the appearance of an ulcerated wound in the distal third of the left lower limb for 20 days. Alcoholic, smoker and previous diagnosis of chronic pancreatitis. On physical examination, upon admission, the abdomen was normotensive, painless on palpation and without masses or visceromegaly. During the investigation of this ulcer and 12 hours after admission, the patient developed diffuse abdominal pain and distension, more intense in the upper abdomen and associated with peritonitis. A computed tomography scan of the upper abdomen and pelvis was performed, which showed a pseudoaneurysm of the dorsal artery of the pancreas with frank extravasation of contrast into the abdominal cavity, in addition to a moderate amount of free blood around the liver. He underwent endovascular embolization treatment, in which he was selectively catheterized splenic artery and dorsal pancreas with therapeutic success.
Keywords: endovascular treatment, ruptured, dorsal pancreatic artery pseudoaneurysm
True aneurysms of the pancreatic duodenal artery are rare, and often fail to distinguish true aneurysms from pseudoaneuryms. Aneurysms of pancreatoduodenal although rare the incidence of 0.1–0.2%. Timely diagnosis and early treatment are essential for the prevention.1 The risk of breakage is independent of size. Endovascular intervention is the preferred initial treatment, but re intervention rates are high in both groups. The ruptured had an aneurysm-related mortality of 10.5%, and the unruptured 5.6%.2 Visceral artery pseudo aneurysm is a rare complication of chronic pancreatitis (CP), all pancreatic or peripancreatic arteries are reported to be involved, while the hepatic artery is less common.3
Arterial complications affect 1-10% of all patients with pancreatitis, most of whom are ruptured pseudoaneurysms, which represent the most dangerous hemorrhagic complication of pancreatitis and can be treated with a high technical success rate through embolization and/or use of endovascular stent.4 The pooled incidence rates of pseudoaneurysms in acute and chronic pancreatitis were 0.05% and 0.03%. The most common site of pseudoaneurysm was the splenic artery 37.7%. Mortality was lower in chronic pancreatitis and splenic infarction was the most common complication where endovascular procedures were successful in over 97% of cases.5
Early detection and treatment of pseudoaneurysms must be performed, as they carry high mortality after rupture. The splenic artery is most commonly involved, followed by the gastroduodenal and pancreaticoduodenal arteries. Gastric artery pseudoaneurysms are less common, with less than 50 cases reported in the literature so far.5,6 The aim of the present study is to report the technical success of the endovascular procedure in the treatment of pseudoaneurysms of the dorsal pancreatic artery.
A 60-years-old white male patient sought the emergency room of the Hospital de Base de São José do Rio Preto-Brazil, complaining of the appearance of an ulcerated wound in the distal third of the left lower limb for 20 days. Alcoholic, smoker and previous diagnosis of chronic pancreatitis. On physical examination, upon admission, the abdomen was normotensive, painless on palpation and without masses or visceromegaly. During the investigation of this ulcer and 12 hours after admission, the patient developed diffuse abdominal pain and distension, more intense in the upper abdomen and associated with peritonitis. Computed tomography of the upper abdomen and pelvis was performed, which showed a pseudoaneurysm of the dorsal artery of the pancreas with frank extravasation of contrast into the abdominal cavity, in addition to a moderate amount of free blood around the liver (Figure 1).
The patient was hemodynamically stable, but with mild tachycardia. He underwent endovascular embolization treatment, in which he was selectively catheterized in the splenic artery and dorsal pancreas (Figure 2). Lipiodol and a controlled-release spring were used to occlude the pseudoaneurysm and dorsal pancreatic artery, maintaining patency of the splenic artery (Figures 3 & 4). At the end of the procedure, there was no extravasation of contrast. During hospitalization, the patient remained in an intensive care bed for 48 hours for hemodynamic surveillance and clinical treatment of post-contrast acute renal failure. The patient was discharged 96 hours after the procedure. Being guided at every hospital discharge to follow up in the outpatient service.
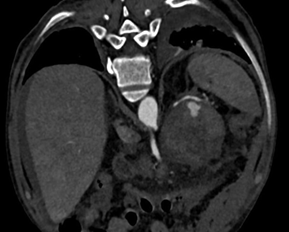
Figure 1 Initial abdominal and pelvis tomography which showed a pseudo aneurysm of the dorsal artery.
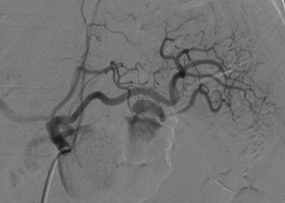
Figure 2 Endovascular embolization treatment, show selectively catheterized in the splenic artery and dorsal pancreas.
The present study presents a case report of ruptured dorsal pancreatic artery pseudoaneurysm, secondary to chronic pancreatitis, in which the therapeutic option was embolization and conservative treatment of abdominal peritonitis. The rupture of the pseudoaneurysm occurred in the hospital during the treatment of a lower limb ulcer, so the diagnosis and intervention were quick. Pseudoaneurysms of the pancreatic arteries are rare in the literature, either as case reports or review of these reports.2–7 Chronic pancreatitis is a complex; multi etiological disease with various clinical presentations can be by different factors alcohol, smoking and genetic.8 The alcoholic etiology of chronic pancreatitis is the most common, the etiology being observed in the case report. Pseudoaneurysm formation is found to be more common (80%) in patients where alcohol abuse is an underlying etiological factor.9 When asymptomatic, the pseudoaneurysm can be an imaging finding. However, if it is symptomatic, this is a warning sign for a possible rupture, in which such bleeding can occur within the pancreatic duct or to the external region of the pancreas, which depends on the topography of the lesion. In the present study, the bleeding was intraperitoneal, causing signs of peritoneal irritation, alerting the patient to the diagnosis.
Bleeding into the duct is called hemosuccus pancreticus and causes symptoms similar to bleeding from the gastrointestinal tract, such as melena, hematemesis, and hematochezia. When they rupture into the abdominal cavity, they cause peritoneal irritation. Therefore, any patient with a history of alcoholism, pancreatitis, or recent pancreatic biliary surgery who presents with a sudden increase in abdominal pain or bleeding symptoms should be investigated for pseudoaneurysm. As for the diagnosis, non-invasive methods can be used, such as tomography and abdominal ultrasound, but usually arteriography is required for confirmation. In the present case, a diagnosis was made with tomography of the abdomen and arteriography for better diagnostic elucidation and treatment. One of the complications to be aware of in these methods is contrast-induced acute renal failure. The patient under study had such a complication, but there was improvement with clinical treatment.
Because it is a rare complication, there are few cases described in the literature showing the diagnosis and management of the condition. In our case, there was therapeutic success through endovascular treatment with glue and controlled-release coils. Thus, the patient was spared an open surgical procedure, prolonged hospitalization and possible intraoperative complications of hostile anatomy due to the history of recurrent pancreatitis. In addition, the patency of his splenic artery was maintained without the use of a stent and consequently maintenance of the spleen.
The endovascular approach in the treatment of pseudoaneurysm of the dorsal artery of the pancreas is safe and effective, especially when the diagnosis and treatment occur early.
None.
Authors declare that there is no conflict of interest.

©2023 de, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.