MOJ
eISSN: 2573-2935


Research Article Volume 2 Issue 1
1Department of Psychiatry, Usmanu Danfodiyo University Sokoto, Nigeria
2Department of Community Health, Usmanu Danfodiyo University Sokoto, Nigeria
Correspondence: Abdulfatai T Bakare, Department of Psychiatry, College of Health Sciences, Usmanu Danfodiyo University Sokoto, Sokoto State, Nigeria, Tel 08024336474
Received: September 23, 2016 | Published: October 24, 2016
Citation: Bakare AT, Isah BA. Psychoactive substances use among in-patients in a nigerian neuropsychiatric hospital: prevalence, pattern and presentation. MOJ Addict Med Ther. 2016;2(1):18-22. DOI: 10.15406/mojamt.2016.02.00016
Objectives: To determine the extent of drug abuse, to identify common drugs of abuse among psychiatric patients in a Nigerian hospital, to determine the duration of exposure to substances prior to presentation for treatment, to identify the common mental and behavioral problems leading to admission.
Design: A cross-sectional descriptive study.
Setting: The study was carried out at the Federal Neuropsychiatric Hospital Kware, Sokoto State and north-western Nigeria.
Participants: One hundred and four inpatients (104) were interviewed. Ethical approval was obtained before the commencement of the study.
Main outcomes measure: Self-report questionnaire on substance use. Analysis was done using the statistical package for social sciences (SPSS), version 20.
Results: The lifetime prevalence of substance abuse among the patients on admission was 69.2%. Active abuse of drugs (during the last month prior to admission) was reported in 43 (41%). Common drugs of abuse were cannabis 39 (90.7%), the cough syrup, Tutolin/Codeine 35 (81.4%) and Solvents/Inhalants, a tire repair solvent 30 (69.8%). The mean duration of substance abuse prior to presentation was 7.1±4.3 years. The common mental and behavioral symptoms at presentation were poor sleep (93%), physical/verbal aggression (74.4%) and aimless wandering (51.2%).
Conclusion: The lifetime prevalence of drug use was quite high among psychiatric patients in this hospital. The abuse of cannabis, codeine syrup and solvents/inhalants still remain a great challenge among patients of the hospital. Most of the patients present for treatment after long duration of abuse when dependence on the drug has developed leading to difficulty in management. We recommend that routine screening and brief interventions for substance use should be critical components of mental health service delivery in psychiatric facilities.
Keywords: Substance abuse; Hospitalized patients; Psychiatric hospital
Substance abuse is on the increase and of global concern. It is a major public health problem, especially in developing countries where there is limited access to effective interventions.1 The study of Ghaleiha in Hamadan on patients hospitalized in psychiatric wards reported that approximately half showed comorbidity with substance abuse.2 Directly or indirectly, every community is affected by drug abuse and addiction. Recent trends indicate that the use of substances have dramatically increased, particularly in developing countries.3
Drug abuse among psychiatric inpatients is a widely recognized problem. Response to treatment in co-morbid patients with this comorbidity is poor, with high rates of recurrence and treatment non-adherence.4 Substances use occurs in all segments of all societies, especially among college students, which results in decreased work, decreased academic performance, increased risk of contracting HIV and other sexually transmitted diseases, accidents, intoxication while working, absenteeism, violent crime, theft and psychiatric symptoms, such as lethargy, hopelessness and insomnia.5,6 According to the United Nations Office on Drugs and Crime,7 about 15 million people in the world used opium and heroin and about 14 million people used cocaine in 2001.
In Australia, according to the most recent national survey on drug consumption, the National Drug Strategy Household Survey (2001),8 about 38 per cent of the population aged fourteen and over or 5.9 million Australians, have used an illicit drug at some stage in their lives, and nearly 17 per cent have reported recent use of an illicit drug. According to a comprehensive Australian study9 illicit drug-related illness, death and crime cost the Australian nation approximately $6.1 billion in 1998-99.Many mental disorders are associated with an increased risk of later substance use disorders.10 The use of drugs such as lysergic acid diethylamide (LSD), cannabis and amphetamines produce symptoms so similar to schizophrenia that accurate diagnosis becomes difficult.11,12
In sub-Saharan Africa, high rates of substance use have been reported among persons presenting for psychiatric evaluation to mental health facilities.13-15 For instance a recent study in Tanzania revealed that the prevalence rate of substance use in psychiatric populations may be as high as 68.5%.13 This rate, though extremely high, was lower than the prevalence of 74% reported in a South African psychiatric facility.14
A study in Israel among hospitalized psychiatric patients reported a lifetime prevalence of drug abuse to be 24%; cannabis abuse was found in 19.7%, opiates in 5.7%, cocaine in 2.7%, amphetamines in 3.4% and methamphetamine in 1.1%. Active abuse of drugs (during the month prior to the study) was registered in 17.3%, cannabis in 11.5%, opiates in 4.9%, amphetamine in 3.8%, cocaine in 1.3% and methamphetamine in 1.1%. In 41.6%, the drug abuse pre-dated symptoms of the mental disorder; in 37.1%, the duration of the mental disorders and the drug abuse was relatively similar, and in 21.3% of cases the duration of mental problems was of longer duration.16
Easy availability of substances, age, gender and having friends and relatives who use substances are the commonly mentioned factors that influence substance use.17 Though psychoactive substances use is common among patients presenting to psychiatric hospitals, few studies have assessed this phenomenon in Nigeria. The high rate of substance abuse and dependence reported elsewhere, and their effects on the course of psychiatric illness, has made identification a high priority. The objectives of this study were to assess the prevalence of psychoactive substances use, to determine the common drugs of abuse, the duration of drug use, and the common pattern of presentation among inpatients at a psychiatric hospital in Sokoto, Northern Nigeria.
Study design and population
This was a cross-sectional study of 104 patients admitted to the Federal Neuropsychiatric Hospital, Kware (FNPHK) in Sokoto, Northern Nigeria. This is a 150-bed hospital located in the outskirts of Sokoto State along the border of Niger Republic. The State is one of the oldest in Nigeria, created in 1976. The hospital serves the entire state as well as the two adjoining states (Kebbi, Zamfara). It also serves patients from neighboring countries, such as Niger Republic. The hospital offers both acute and long term care for psychiatric inpatients. The hospital also operates an outpatient’s clinic and an emergency clinic on a daily basis. The average length of stay in the hospital is approximately 4 weeks. Patients with substance use disorders can stay for as long as 3 months.
Participants were one hundred and four patients admitted to the hospital in the month of July, 2014. The inclusion criteria were;
Patients who that were judged too unstable to be interviewed were excluded from the study. During the study period, 121 patients were admitted and 104 (84.9%) met the inclusion criteria.
All the participants completed a self-report questionnaire designed by the researchers. In addition, the case notes of all the participants were retrieved and examined for additional information. After consent was obtained The questionnaire included information on demographic data, patient admission information (e.g. voluntary or compulsory admission, first or re-admission, whether violence contributed to admission), substance use history (chief complaints at presentation, types of substance abuse, duration of abuse prior to presentation, urine test for common substances of abuse). Those with little or no education were assisted in filling out the questionnaire. The interview was completed during within one month (July 2014).
Ethical approval was obtained from the Ethical Committee of the Federal Neuropsychiatric Hospital Kware, Sokoto State, Nigeria. International ethical norms and standards were strictly adhered to at all times.
The results were analyzed using the Statistical Package for Social Sciences, version 20. Sample means, standard deviations and percentages were calculated.
One hundred and twenty-one patients were admitted during the study period. The study population comprised 104 participants who met the inclusion criteria. The age range was 18-60 years; mean age of the subjects was 31.5±9.5 years. Eighty-nine (85.7%) were males, never married (54.3%), unemployed (63.8%) and students (50.4%). (Table 1)
Variables |
N (%) |
Age |
|
18-27 |
37(35.6) |
28-37 |
41(39.4) |
38-47 |
19(18.3) |
48-57 |
4(3.8) |
58-67 |
3(2.9) |
Sex |
|
Male |
89(85.6) |
Female |
15 (14.4) |
Marital Status |
|
Single |
57(54.8) |
Married |
42(40.4) |
Divorced |
5(4.8) |
Education |
|
Nil |
12(11.5) |
Quranic only |
47(45.2) |
Primary |
16(15.4) |
Secondary |
25(24.0) |
Tertiary |
4(3.8) |
Occupation |
|
Employed |
55(52.9) |
Unemployed |
49(47.1) |
Total |
104(100) |
Table 1 Socio demographic characteristics.
The lifetime prevalence of substance use was 69.2%, active abuse of drugs (during the last month) was registered in 41%, which also represents the percentage of patients primarily admitted for as cases of substance used disorder. Among those admitted primarily for substance use disorder, common substances of abuse were cannabis (90.7%), tutolin/codeine (81.4%), solvent/inhalant (69.8%), Tramal (60.5%), D5 (46.5%), and Rohypnol (44.2%), benzhexol (30%), alcohol (4.7%). We also found that 93% of active abusers used two or more substances (Table 2) & (Figure 1).
Name of Substance |
Description |
Alcohol |
Various alcohol containing drinks |
Cannabis |
Tetrahydrocannabinoid (THC) |
Diazepines |
Benzodiazepines, mainly Valium 5mg |
Benhexol |
Psychotoxic anticholinergic |
Rohypnol |
A benzodiazepine |
Shisha/Sheesha |
High nicotine flavored tobacco smoked with a hookah |
Tramal |
Opioid analgesic |
Tutolin-Codeine syrup |
Cough syrup containing codeine |
Table 2 Description of various substances of abuse as used in this study.
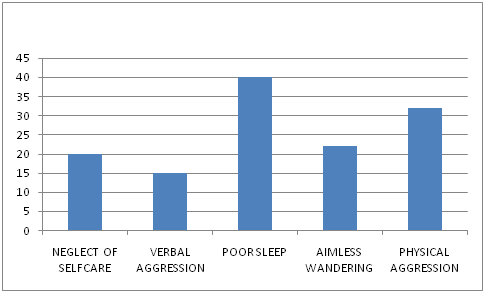
The mean duration of substance abuse prior to presentation was 7.1±4.3 years. Thirty-five participants (81.4%) had used drugs for more than 5years prior to presentation at the hospital. The common symptoms at presentation by current substance abusers were poor sleep 40(93%), physical aggression 32 (74.4%) aimless wandering 22 (51.2%), neglect of self-care 20 (46.5%) and verbal aggression 15 (34.9%) (Figure 2).
The most common disorder among the hospitalized patients were substance use disorders 43 (41.3%), followed by schizophrenia 41(39.4%), substance induced psychotic disorders 10 (9.6%) and mood disorders 10(9.6%). Among the participants, 71 (68.3%) were re-admissions and 31.7% were first admissions (Figure 3).
This study was conducted to determine the prevalence and pattern of substance abuse among hospitalized psychiatric patients in a Nigerian Psychiatric Hospital in 2014. The findings of the study showed that 69.2% of the patients on admission had used psychoactive substances at some time in their lives. A study of 124 inpatients admitted into a Psychiatric Unit of the University of Uyo Teaching Hospital reported a lifetime prevalence rate of 48.4%. This is slightly lower than found in our study. International prevalence studies have revealed that persons with severe mental illness have significantly higher rates of substance use, particularly of alcohol, cannabis and amphetamines, than the general population.18,19 Fowler et al.20 also found higher rates of alcohol, cannabis and amphetamine use among patients with schizophrenia relative to the general population in Australia.20 The prevalence reported by Sinclair et al.21 in Hamadan was higher than the rate obtained in the present study. The lower rate reported in previous studies compared to our study could be attributed to the fact that our study was conducted among inpatients of a psychiatric hospital where all the patients that presented had major psychiatric disorders. The use of substance has been reported to be higher among people with mental illness compared with the general population.22
The prevalence rate of current abuse of drugs was registered in 41%. Common substances abused were cannabis (90.7%), Tutolin/Codeine (81.4%), solvent/inhalant (69.8%), Tramal (60.5%), D5 (46.5%), and Rohypnol (44.2%), Benzhexol (30%) and Alcohol (4.7%). This pattern differs from that reported in a study in Uyo, Southern Nigeria, which showed. A prevalence rate of current use of alcohol to be highest 36.3%; cannabis 28.3%; cigarette 14.5%; cocaine 0.8%; snuff/fumes 2.4%; pain killers and kola nuts 1.6%.23 A study in Israel also investigated the extent of drug abuse in a sample of psychiatric patients hospitalized in a psychiatric hospital and in the psychiatric department of a general hospital. Alcohol consumption was highest in the two hospitals studied, which does not concur with the findings of our study.16 This difference might be due to religious and cultural differences. In the northern part of Nigeria where our study was carried out, the majority of people practice Islam. In Islam religion, which wais the religion of the majority of the participants in this study, the drinking of alcohol is prohibited and is therefore of limited access. This is probably the reason why alcohol is not prevalent among the patients in our study.
We also found that 93% of active abusers used two or more substances. This is higher than reported by.24 Katz et al. 16 in Israel reported a much lower rate of multiple substance use 28.2% of psychiatric outpatients. The higher rate in our study may reflect the sample studied. We studied psychiatric inpatients while their sample was comprised of psychiatric outpatients. Common symptoms at presentation by patients with substance use disorders in our study were poor sleep, physical aggression, aimless wandering, neglect of self-care, and verbal aggression. It is evident from the findings in this study that the reasons for presentation among the substance abuse patients were the development of mental and behavioral symptoms and not because they were using substances. The majority had used the substances for more than 5 years before presentation. No comparison studies regarding this issue were found.25
This was a cross-sectional study and data were collected from self-report measures and case notes. Future research should add diagnostic measures. This research was done in one region; a collaborative group study is suggested in order to obtain samples from other Nigerian neuropsychiatric hospitals.
This study showed that substance use disorders are prevalent among persons presenting at a Nigerian psychiatric hospital. Cannabis, codeine syrup, inhalants, Tramal, diazepam and Rohypnol were the common substances of abuse among the patients studied. Substance use was of long duration in this study population. Because of the high prevalence of substance use among psychiatric inpatients, it is recommended that a routine screening policy be put in place to identify substance use in all patients admitted to hospital for psychiatric reasons. This should become a critical component of mental health delivery. In addition, because substance abuse begins many years before a hospital admission, culturally appropriate outreach services are needed for prevention and early treatment.
None.
The author declares no conflict of interest.

©2016 Bakare, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.