MOJ
eISSN: 2576-4519


Research Article Volume 7 Issue 1
1Department of Biomedical Engineering, Universidad Tecnológica del Uruguay, Uruguay
2Department of Mechatronics Engineering, Universidad Tecnológica del Uruguay, Uruguay
Correspondence: Carlos Diaz Novo, Department of Biomedical Engineering, Universidad Tecnológica del Uruguay, Fray Bentos Rio Negro, Uruguay, Tel +59891815701
Received: July 13, 2023 | Published: July 27, 2023
Citation: Novo CD, Haller WM, Ruiz EA, et al. Development and functional validation of tarsometatarsal prosthesis. MOJ App Bio Biomech. 2023;7(1):124-131. DOI: 10.15406/mojabb.2023.07.00185
Assistive Technology (AT) plays a crucial role in providing aid products, including prostheses to persons with disabilities. Tarsometatarsal (TMT) disarticulation, a type of partial foot amputation, is associated with complex gait disorders. However, there is limited research on the functional impact of TMT prostheses on gait. This study aims to develop and functionally validate a 3D-printed TMT prosthesis using finite element analysis and human motion laboratory studies. A 65-year-old patient with TMT amputation participated. Digital models of the amputated and healthy feet were obtained through 3D scanning. The prosthesis design was created using Fusion 360 software. Finite element analysis validated the prosthesis design. The prosthesis was manufactured using thermofusion printing with a biocompatible thermoplastic elastomer material. Functional validation included walking, running, and the Timed Up and Go test using motion analysis technologies.
Finite element analysis demonstrated the structural integrity and safety of the TMT prosthesis during propulsion. The manufacturing process resulted in an adjustable and cost-effective prosthesis. Functional validation revealed improvements in gait quality, symmetry, and spatiotemporal parameters with the prosthesis. Vertical ground reaction forces during walking resembled the normal range, and running performance showed increased symmetry and propulsion velocity. The Timed Up and Go test showed that prostheses reduce time and improve efficiency. The development and functional validation of the 3D-printed TMT prosthesis offer a promising solution for individuals with TMT disarticulation. This approach addresses the need for assistive technologies in low-income countries with limited access to prostheses. Advanced technologies and a patient-centred approach contribute to improving mobility, gait patterns, and overall quality of life for individuals with partial foot amputations. Future research will focus on exploring additional parameters and developing new prostheses to further enhance gait improvements.
Assistive Technology (AT) includes systems and services through which people obtain assistive products, such as prostheses, orthoses, among others.1 Partial foot amputations are often the result of severe infections, vascular disorders, and trauma.2 The disease that causes the most lower-limb amputations is diabetes.3 In Uruguay, 60% of all amputations are due to diabetes.4 Partial foot amputations, such as TMT disarticulation, are usually associated with complex gait disorders, among which are loss of forefoot leverage, reduction in the plantar loading surface (increasing surface pressure), and loss of pronation and supination, as well as absence of the propulsive phase (push-off) of the gait cycle.5–7 Complex technologies for human movement analysis need to be applied in order to obtain objective input on the true functional impact of the true functional impact of the TMT prosthesis on the gait cycle.
Although there are very few countries with national policies and programs, there are no national services for the provision of these technologies in many Low Income Countries (LICs). According to the World Health Organization, only 5%–15% of 40 million people with amputations in LICs have access to prostheses.8 In particular, this access relies on intermittent donations or charity services, which often focus on delivering large quantities of low-quality or used products, and lack mechanisms for repair and maintenance. The above is due to a lack of state financing, nationwide service delivery systems, user-centred research and development, procurement systems, quality and safety standards, and context appropriate product design.9 Nowadays, most research is focused on upper limbs, and the lack of homogeneous data highlights the need for more scientific research to enable wider availability of knowledge about 3D-printed prostheses and their applications on partial foot amputations.10,11
This work combines Finite Element (FE) analysis tools for theoretical validation of the prosthesis design with human motion laboratory studies for functional validation of the AT.12–15 The anatomic surface data of the residual limb was obtained with a new scanning system, and 3D printing technologies were employed to manufacture the TMT prosthesis, with low-cost materials, making this prosthesis a potential solution for TMT patients from LICs.
Despite the fact, that many aspects of pathological gait have been the subject of scientific inquiry, to the knowledge of the authors, changes of gait patterns after a TMT prosthetic implementation have not been sufficiently documented.16 For this reason the purpose of this study was to develop and functionally validate a new 3D-printed prototype of TMT prosthesis. Three tests were conducted to evaluate the subject's performance under different footwear conditions: barefoot and with prosthesis. The tests involved walking, sitting up and down, and running.
Case study
The subject of this study is a 65-year-old individual who underwent a TMT amputation over 15 years ago. At the time of the study, the patient's height was measured at 1.75m and their weight at 83 kg.
Before commencing the procedures, a thorough and comprehensive explanation of the project's objectives and procedures was provided to the patient. The patient was informed about the potential risks and benefits associated with their participation, as well as their rights and responsibilities. To ensure their informed consent, the patient was given a consent form, which they read and signed to indicate their understanding and willingness to take part in the study. Throughout the study, all procedures followed international recommendations for clinical research, specifically adhering to the World Medical Association's Declaration of Helsinki. Approval from Universidad Tecnológica del Uruguay (UTEC) was obtained to ensure compliance with the institution's specific requirements. All questionable aspects of the study underwent review and received approval from an institutional review board.
Prototype design
Patient´s feet scanning procedure
In order to design TMT prosthesis, we needed to have a digital model of the patient´s amputated and healthy feet; therefore a 3D scan of both feet was performed using the Artec Leo 3D Scanner.
The patient was instructed to sit down and remove their footwear, and an alcohol solvent was used to remove any residual grease and sweat from the surface of the amputated limb. The scanner was set to its maximum spatial resolution of 0.2 mm and a temporal sampling resolution of 22 frames per second.17 With the amputated leg in the air, the entire contour of the residual limb was captured in all possible planes. A visual check was then carried out to ensure that the mesh elements of the entire scanned surface of the amputated limb were filled. Subsequently, a visual analysis of the anthropometric correspondence between the scanned digital volumes and the physical limb was conducted. A similar procedure was carried out on the healthy limb.
The scans were converted into STL format to be loaded and manipulated with Fusion 360 software, which is a cloud-based 3D modeling CAD, CAM, CAE and PCB software platform for product design and manufacturing.
3D Modeling
The STL scans were imported into Fusion 360, where various methods were applied to prepare the mesh, including reiterative element reduction. Subsequently, the design of the prosthesis was carried out.
The healthy foot was separated and scaled, and a symmetric mirror of it was made in order to have a healthy left foot. Then, the amputated foot was subtracted from it, creating a thickened shell that externally resembled a healthy foot but internally matched the shape of the amputated foot. A platform was generated for the base of the prosthesis, not only to increase the contact area with the ground, but also to enhance the rigidity of the piece. A section of material was removed, and lace grips were created to facilitate foot insertion and secure it. The design was recursively smoothed in order to reduce rough geometric forms and edges and limit the amount of sharp angles to avoid problems with mesh calculations. The result is socket prosthesis with embedded foot in it that closely resembled the advanced orthopaedic prosthetics provided by MG LATAM (Figure 1).18
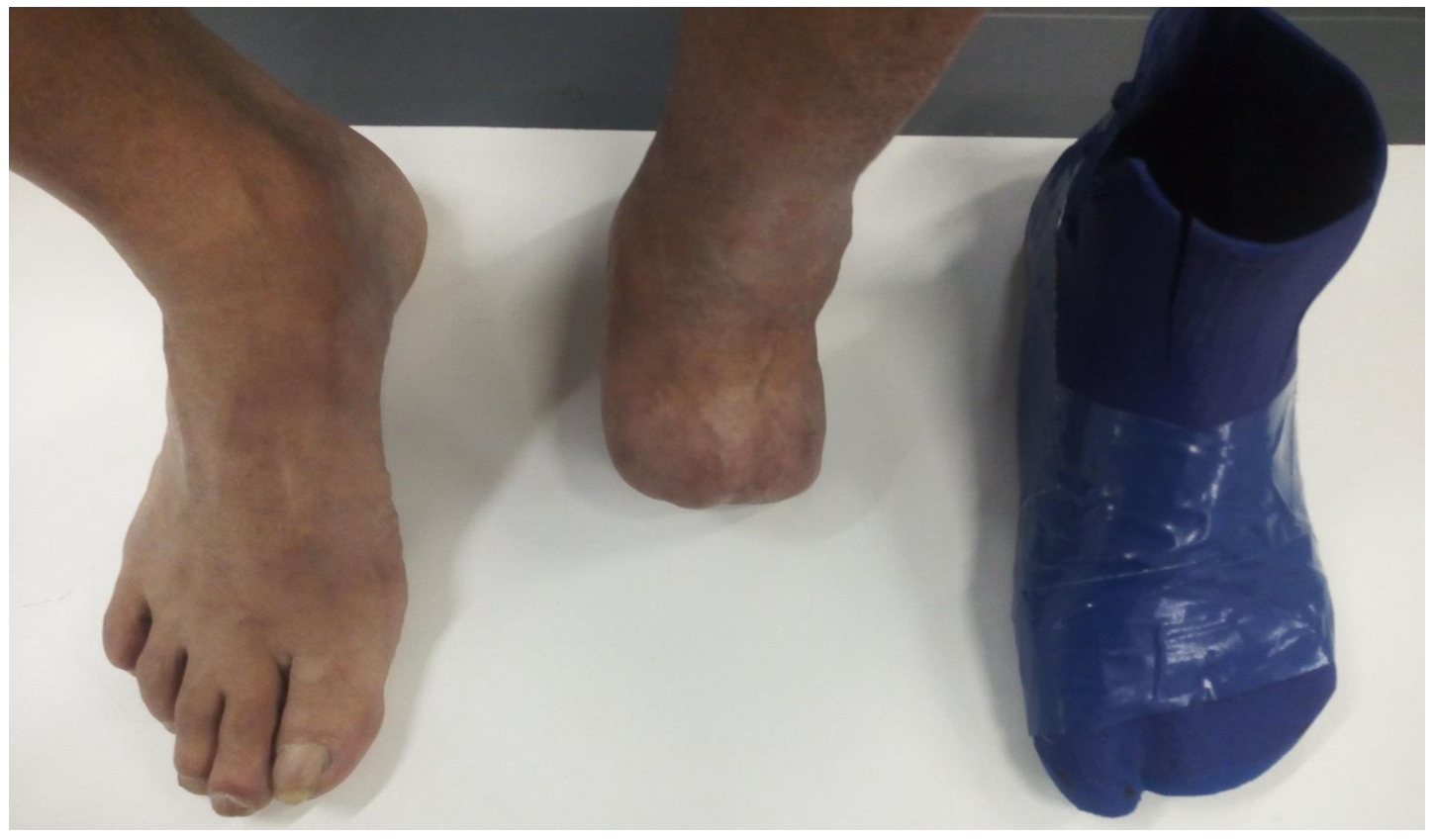
Figure 1 Photo of patient´s healthy foot, amputated foot, and final prosthesis, which is similar to MG LATAM´s.18
Finite element analysis
The program used, Fusion 360, enables us to remotely do FE analysis using their servers. The educational version was used in this case and the average time the study took was 30 minutes. For the study, the thermoplastic elastomeric (TPE) material available in the Laboratorio Abierto (LAB A) at UTEC was selected.19 The analysis was carried out with the basic geometry obtained in the design process and physical properties of the material. The geometric and material properties used in this analysis are found in Table 1.
|
Properties |
Value |
Unit |
|
Young’s modulus |
0.147 |
GPa |
|
Poisson's ratio |
0.49 |
— |
|
Shear modulus |
102 |
Mpa |
|
Density |
1140 |
kg/m3 |
|
Tensile strength (20% infill) |
32 |
MPa |
|
Element type |
Triangle |
— |
|
Elements |
19186 |
— |
|
Nodes |
32686 |
— |
|
Minimum elements size |
20 |
% average size |
|
Contact tolerance |
0.1 |
mm |
|
Maximum force |
1000 |
N |
|
Area of contact |
0.0069 |
m2 |
|
Volume |
7.094 x10-4 |
m3 |
|
Estimated mass |
0.808 |
Kg |
Boundary restrictions definition
For FE analysis, the geometry proportions and its mechanical properties are not enough. The type of study, the forces applied, and the restrictions must be selected in order to simulate normal situations to which the prosthesis would be constrained. In this case, a static study was selected. As part of the boundary conditions, an extreme load state of the prosthesis was considered. This corresponds to the patient's use of the prosthesis to ascend and descend stairs. The extreme case is linked to the patient supporting their weight on three-quarters of the prosthesis and one quarter of the prosthesis linked to the support surface, for which all displacements in the three axes were reduced to zero (0). The total forces add up to 1000 N, which is 120% of their body weight (Figure 4), representing the maximum in walking, and are distributed over an area of approximately 0.0069 m2, as shown in Figure 2(a).7 This situation is analogous to the push-off stage in the gait cycle, but with a greater moment due to the angle of the forces.
Prosthesis manufacturing
Once the prosthesis design was completed, it was transformed into a format compatible with the selected manufacturing device. The selected technology was thermoforming, and the Raise 3D Pro 2 Plus printer from UTEC's LAB A was used. This printer has an energy consumption of 600W, and a print area that is 0.305 m wide, 0.305 m long, and 0.605 m tall, allowing the prosthesis to be printed in one piece.
For the print, a TPE material was selected, which is available in LAB A. This material was chosen because it is biocompatible, washable, disinfectable, and resistant to chemicals, allowing it to be in contact with the person's foot without causing discomfort or conditions such as changes in circulatory nature or soft tissues. However, it was chosen mainly due to its mechanical characteristics. As it is an elastomer, it is flexible, which allows it to store energy as a result of functional deformation and return this energy when the deformation ceases, contributing to the propulsion efforts of the human body. Additionally, said material is cost-effective.
Before printing, the printer had to be configured according to the requirements of the print material. The person in charge of LAB A selected a 0.15 mm layer height, a 0.8 mm wall thickness, 50% infill density in a gyroid pattern, a printing speed of 25 mm/s, and a printing temperature of 225°C.
Functional evaluation of the prosthesis
Prior to the experimental data capture sessions, three sessions of 6-minute walks combined with 10 minutes of rest were conducted with the subject wearing the prosthesis. These sessions had a double objective, to promote the muscular warming of the body, and having him walk on a Pro-Form Carbon T7 treadmill in front of a mirror to allow him to adapt his gait compensatory mechanics to the prosthesis regimes of use.
After warm up sessions, 30 trials for each of the three tests were conducted along a pathway of 10 m, located in UTEC’s movement analysis laboratory, in two footwear conditions: 15 trials barefoot and the rest with prosthesis. Data capture was performed to obtain parameters related to kinematics, kinetics, and physiological features for subsequent comparison with a control group of healthy subjects, with the same gender, age, anthropometrics and socio-cultural characteristics.
A functional analysis was performed using instrumental technologies from the BTS Bioengineering digital ecosystem, which enabled an objective analysis of waking, running and timed up and go through spatio-temporal kinematics and kinetics. These technologies included a wireless inertial sensor (G-WALK®) and four force plates for dynamic gait analysis (BTS P-6000).15,22,23
Walk protocol
The walk protocol provides all the spatio-temporal gait parameters for the functional evaluation of neurological and orthopaedic patients, allowing the objective analysis of motor capability. The following parameters were evaluated:
Running protocol
The Running protocol provides spatio-temporal running parameters for the functional evaluation of neurological and orthopaedic patients, allowing the objective analysis of motor capability. The following parameters were evaluated:
Timed Up and Go protocol
This is a balance evaluation test based on the execution of an easy task allowing us to assess the subject’s functional mobility. This test enables us to determine the actual risk of falling, the ability to keep balance while executing such different movements and the walk strategy being used. The following parameters were evaluated:
Design and simulation of the tarsometatarsal prosthesis proposal
The following result provides an in-depth analysis of a prosthetic device using finite element methods. The study focuses on key parameters such as displacement, Von Mises stress, and safety factors. The findings offer valuable insights into the device's functionality under specific boundary conditions as presented in Figure 2(a).
Displacement analysis reveals a greater degree of movement in the posterior region, particularly on the heel. This decreases as we approach the constraints. A maximum displacement of 43.28 mm is observed at the upper rear part of the socket, while the heel shows approximately 35 mm. This results in an inclination of around 8 degrees of flexion. Considering that normal foot flexion during propulsion ranges between 32 and 40 degrees, there remains a significant margin for energy absorption and release during the propulsion phase, provided the socket fit is optimal and without losses, as shown in Figure 2(b).
The Von Mises stress analysis, see Figure 2(c), identifies several areas with high values, some located in the socket where the prosthesis is thinnest. However, the highest values are found near the constraints, peaking at 12.06 MPa. This is significantly less than the material's Tensile Strength and Yield Strength.
Safety factor analysis, see Figure 2(d), shows that the majority of the prosthesis exceeds acceptable values. Only two areas, located close to the constraints, display a factor that could be considered slightly low. Yet, even these areas maintain a safety factor above 2.5, which is more than sufficient to prevent deformation or breakage.
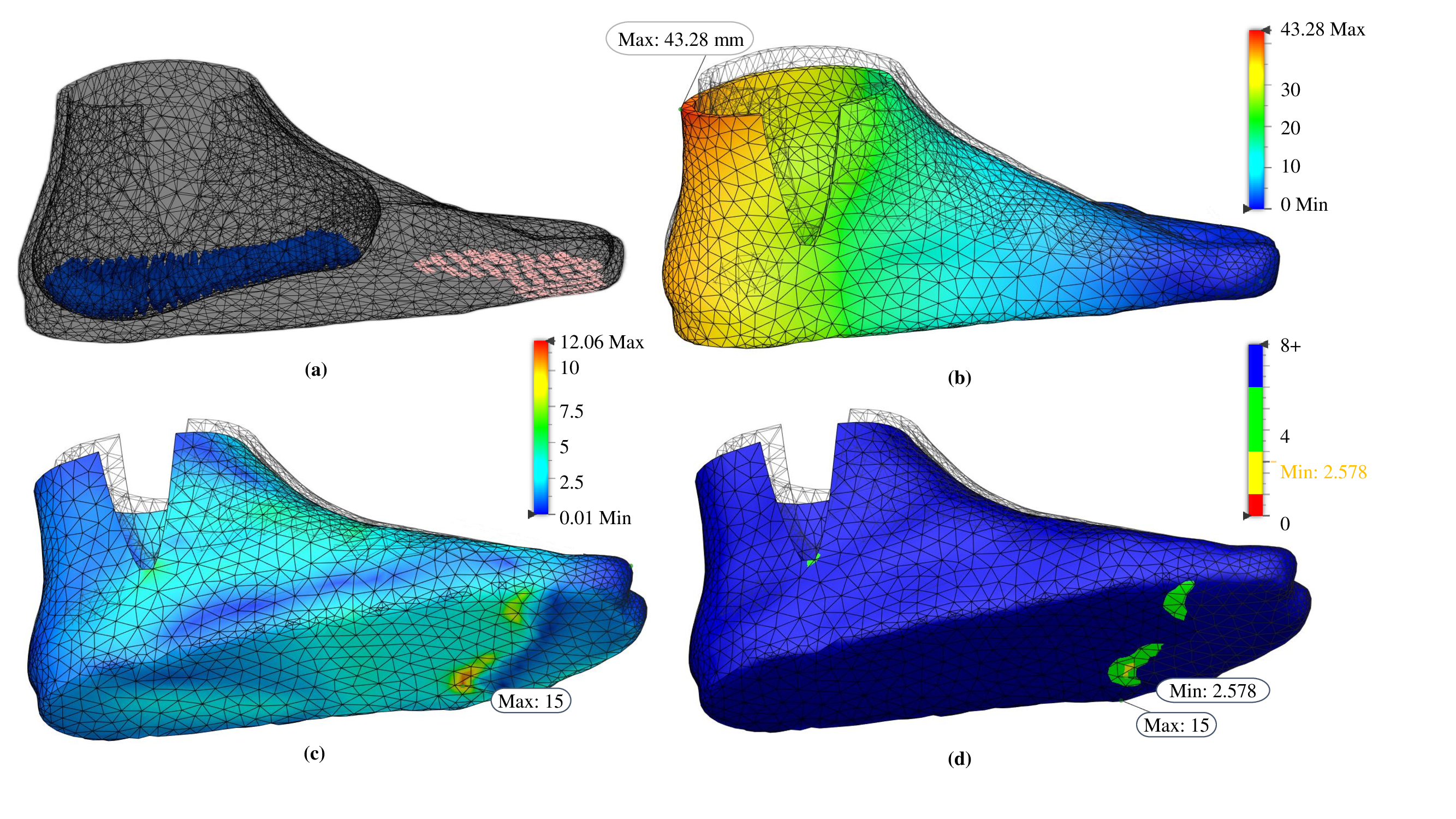
Figure 2 Finite element analysis showing the load distribution and constraints (a), displacement (b), Von Mises stress (c), and safety factor (d).
These findings suggest that the prosthesis is suitable for walking and is functional during the propulsion phase.
Manufacturing of the prosthesis
Regarding the results of the prosthetic manufacturing process, the total printing time was approximately 83 hours. After printing, imperfections were removed using a manual electric lathe to avoid potential issues with the patient. The final consumption of elastomeric filament was 0.550 kg, and after the intervention, the final weight of the prosthesis was around 0.500 kg. The estimated manufacturing cost is 42.6 USD (material and printer consumables only), while the total development cost is estimated at 287 USD.
Validation of use
Different design solutions for the prosthesis were examined to ensure a high level of safety and sustainability. Key aspects such as easy handling, assembly, and the ability to don and doff the prosthesis in various anatomical postures, such as sitting or lying down were taking into the account. Solutions have been implemented to enhance the prosthesis fixation to the ankle joint and residual limb, preventing unnecessary slippage on inner surfaces. This is crucial for preventing the formation of ulcers and opportunistic injuries. Overall, a durable and reliable solution is offered, improving the user’s quality of life by promoting mobility and minimising associated risks.
Functional validation
Below are the results of the evaluation of the functional performance of the subject while using the prosthesis in daily physical activities, including walking, sitting, standing, and running.
Walking test
The results related to gait indexes with and without the prosthesis for the intact and amputated limb are presented.
For the three evaluated indexes, an improvement in the symmetry of the amputated and intact limb is evident when the prosthesis is used, which directly correlates with an increased gait quality. Both the amputated and intact limb show a higher quality index, with a slight increase when the prosthesis is employed, see Figure 3(a), which is linked to an improvement in the timing of the stance and swing phases during gait. Regarding the symmetry index in the three planes of movement, see Figure 3(b), a significant increase is observed in the anteroposterior plane (Tilt-Sagittal) when using the prosthesis, indicating a reduction in imbalance in this plane, combined with a discrete improvement in the obliquity index (Obliquity-Frontal). Finally, the overall evaluation of symmetry between both limbs reflects an improvement in gait when assisting the amputated limb with the prosthesis, as shown in Figure 3(c).
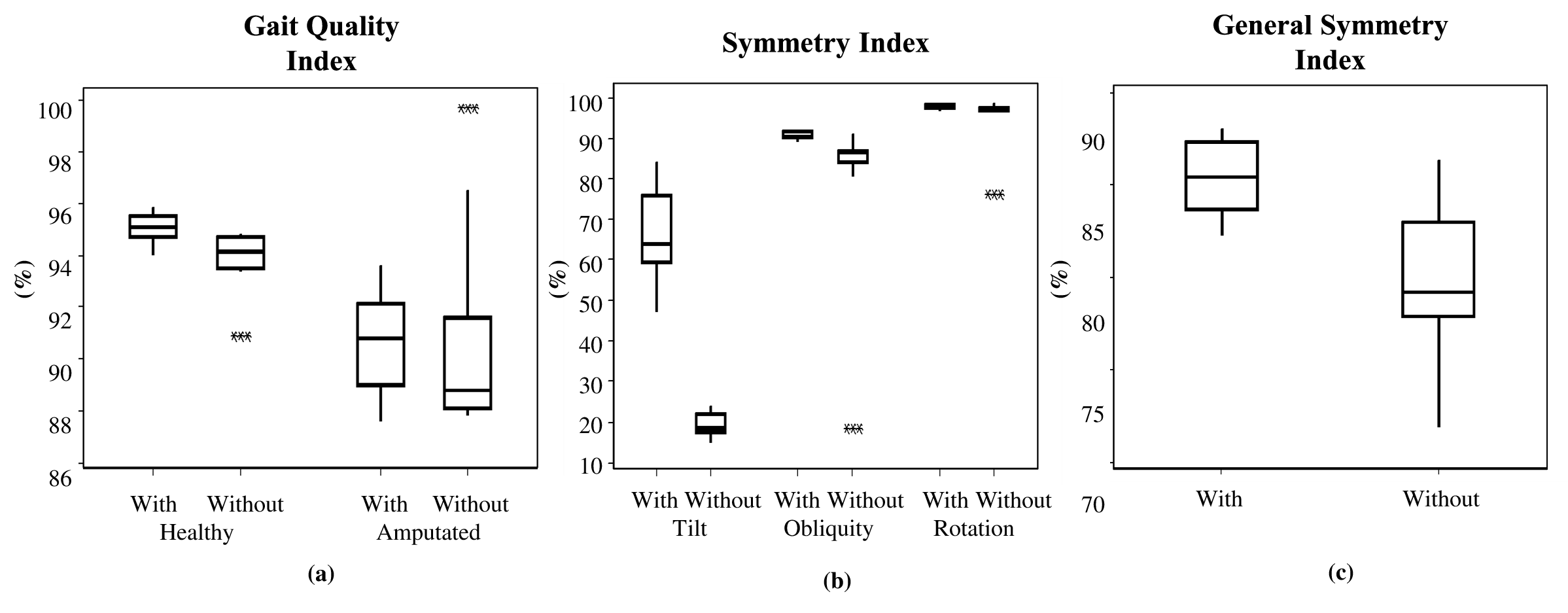
Figure 3 Boxplot of indexes related to gait (a) Gait Quality Index Left and Right, (b) Gait Symmetric Indexes (Tilt, Obliquity, Rotation), and (c) General Symmetry Index of Gait.
Vertical ground reaction force from walking test
The results presented below correspond to the vertical ground reaction forces during gait. During the analysis of vertical ground reaction force (Figure 4), significant differences were found between the healthy leg and the amputated one, both with and without prosthesis. Overall, greater similarity to the normal range was exhibited by the healthy leg in both amplitude and morphology. In contrast, the amputated leg without the prosthesis showed an atypical morphology, characterised by a plateau instead of a shape similar to the normal pattern. However, when the prosthesis was used, significant improvement in the behaviour of the vertical ground reaction force in the amputated leg was observed. Regarding the maximum vertical force during the stance phase, it was found that the healthy leg transmitted significantly more force compared to the amputated leg in both evaluated situations. Differences in the morphology of the vertical force throughout the gait cycle were also evident between the amputated and healthy legs, the latter being closer to the control group. Additionally, the transition time between the initial stance phase and the propulsion phase was shorter for the amputated leg compared to the healthy leg in both analysed conditions, the time being the shortest when the prosthesis was not used.
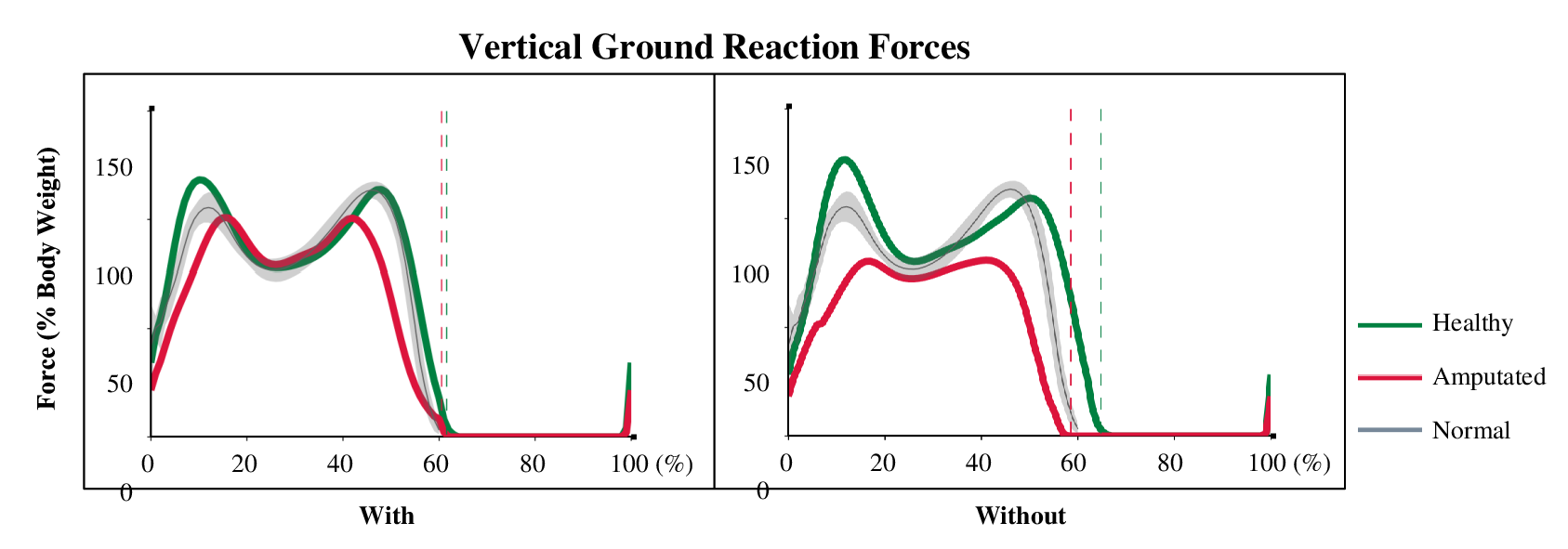
Figure 4 Representation of vertical ground reaction force as a function of the gait cycle with and without prosthesis compared with a control group of the same age range as the patient.
Running
The results related to indexes and spatiotemporal parameters of running with and without the prosthesis for the intact and amputated limb are presented below.
For the two evaluated indexes, an improvement in the symmetry of the amputated and intact limb is evident when the prosthesis is used, which directly correlates with an increased quality of running. Regarding the symmetry index in the three planes of movement, see Figure 5(a), a substantial increase is observed in the anteroposterior plane (Tilt-Sagittal) when using the prosthesis, indicating a reduction in imbalance in this plane. The evaluation of the symmetry between both limbs reflects an improvement in gait when assisting the amputated limb with the prosthesis; see Figure 5(b). The analysis of the propulsion velocity, see Figure 5(c), shows that it is lower in the amputated limb compared to the intact limb in both cases, with and without the prosthesis. When using the prosthesis there tends to be greater symmetry between both limbs. Analyzing the specific cases, when the prosthesis is not used, a slightly higher propulsion velocity is recorded in the intact limb, unlike in the amputated limb, where a higher propulsion velocity is observed when the prosthesis is employed.
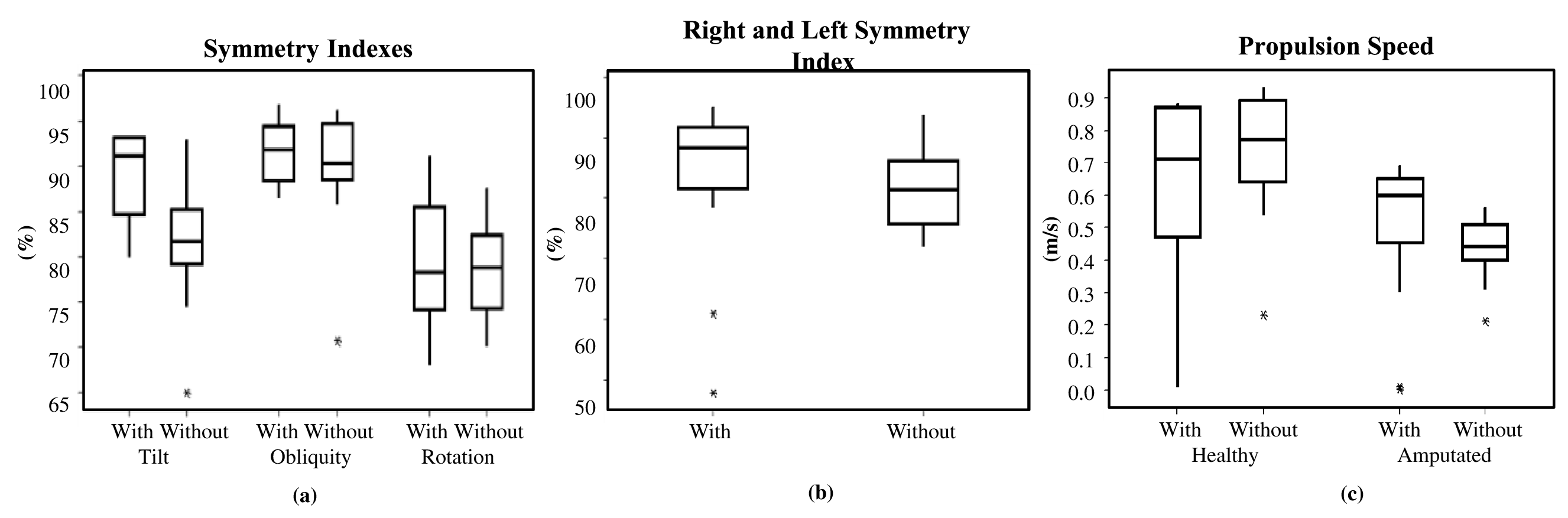
Figure 5 Boxplot of indexes and spatio-temporal parameters of Running (a) Symmetry Indexes during Running, (b) Right and Left Symmetry Index, and (c) Propulsion Speed.
Timed Up and Go
The results related to the temporal parameters of the Timed Up and Go, Sit-to-stand, and Stand-to-sit activities with and without the prosthesis are presented below. Regarding the temporal parameters of the Timed Up and Go activity, a slight decrease in time is generally observed when using the prosthesis, indicating increased efficiency in its execution. As for the Sit-to-stand and Stand-to-sit transition times, see Figure 6(a), a shorter time is recorded in the former case, and an even shorter time is recorded when using the prosthesis. However, in the Stand-to-sit case, no substantial decrease was observed when using the prosthesis. Regarding the round-trip walking times, a slight reduction in times is observed when the prosthesis is employed; see Figure 6(b). In relation to the total activity time, a slight decrease is observed when using the prosthesis, which has a beneficial effect for the user; see Figure 6(c).
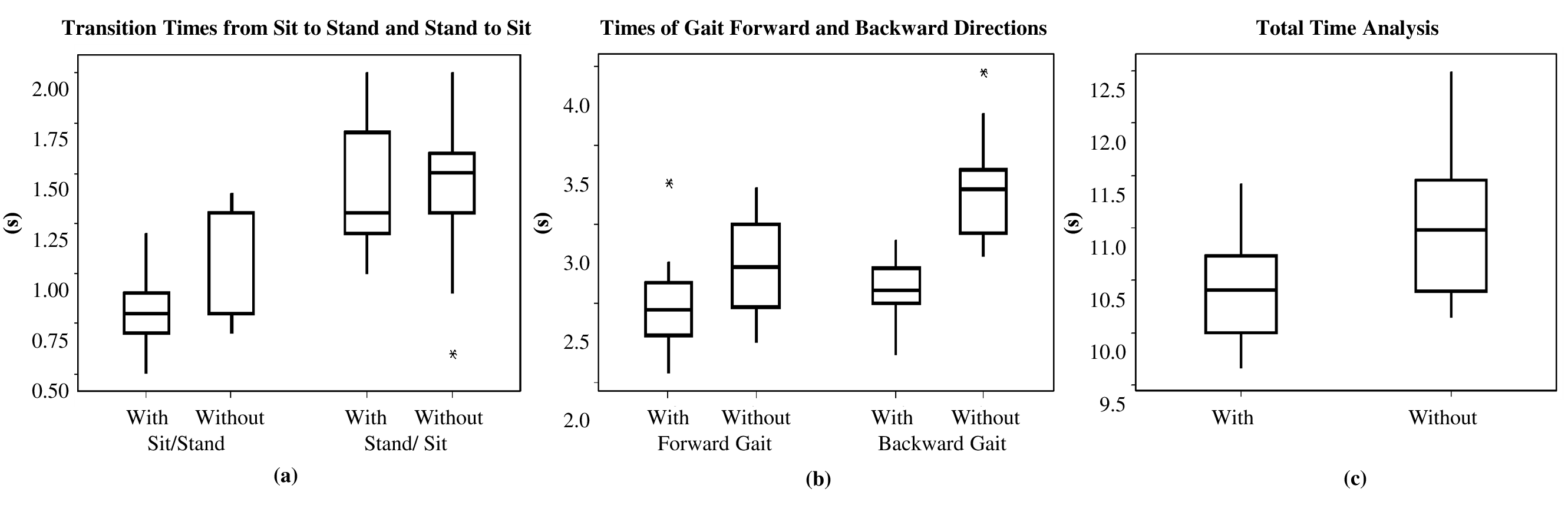
Figure 6 Boxplot on temporal parameters in Time Up and Go (a) Transition Times from Sit-to-stand and Stand-to-sit, (b) Times of Gait Forward and Backward Directions, and (c) Total Time Analysis.
The results related to the spatiotemporal parameters of the Time Up and Go, Sit-to-stand, Stand-to-sit, Mid Turning, and End Turning activities with and without the prosthesis are presented.
Regarding the spatiotemporal parameters of the Timed Up and Go activity, there is a slight reduction in acceleration in all cases when the prosthesis is used, indicating a decrease in instability in all planes, see Figure 7(a) and 7(b).
As for the angular velocity during turning, no significant changes are observed in the middle of the activity, as shown in Figure 7(c). However, at the end of the turning, a slight increase is observed when the prosthesis is employed.
The design and manufacturing of the TMT prosthesis were successfully achieved using 3D scanners and thermofusion printing, resulting in an adjustable and cost-effective product. This technology has made personalised 3D-printed prostheses accessible in developing countries, where options for lower limb assistive devices lack. While advancements have been made in the development of 3D-printed prostheses for upper limbs, the application of this technology in creating prostheses for lower limbs, specifically for TMT amputations, has been sparsely documented.
The study addresses this issue and represents a significant step towards finding effective and affordable solutions for patients with TMT amputation in resource-limited settings. The combination of 3D scanning and thermofusion printing allowed for the creation of customised prostheses that optimally fit the patients' anatomy, enhancing comfort and functionality.
The low-cost approach of this technology is particularly relevant in environments where financial resources are limited, and access to quality prostheses is scarce. The ability to manufacture prostheses on-site and adjust them to individual patient needs enables more effective and personalised care.
The results support the effectiveness and feasibility of 3D-printed TMT prostheses. The participating patients experienced significant improvements in their quality of life and their ability to perform daily activities. This demonstrates the potential of this technology to address the functional challenges associated with TMT amputation and improve patients' quality of life.
Looking ahead, there are several areas of development that can further enhance the functionality and user experience of TMT prostheses. One such area is the improvement of prosthetic materials to ensure better breathability and ventilation of the skin. By addressing these aspects, discomfort, skin irritation, and potential complications such as skin infections can be minimised or avoided.
Another important aspect to consider is the development of mechanisms to adjust the height of the prosthesis. The ability to easily customise the height based on individual preferences and needs will contribute to optimal alignment and gait dynamics. This adjustability feature will provide users with greater control and comfort, ultimately leading to improved mobility and overall quality of life.
In summary, while the study has showcased the potential of 3D scanners and thermofusion printing in creating TMT prostheses, there is still room for future advancements. By addressing aspects such as prosthetic material breathability and the inclusion of adjustable height mechanisms, we can further enhance the functionality, comfort, and overall experience of the prosthetic device. These developments will continue to drive progress in the field and promote the availability of affordable and effective assistive devices for individuals with lower limb amputations worldwide.
In conclusion, the development and functional validation of the TMT prosthesis have shown promising results in improving the mobility and gait patterns of individuals with partial foot amputations, specifically TMT disarticulation. The study addresses the need for assistive technologies in low-income countries where access to prostheses is limited. By combining finite element analysis for theoretical validation of the prosthesis design and human motion laboratory studies for functional validation, the researchers aimed to provide an objective understanding of the prosthesis's impact on the gait cycle.
Advanced technologies such as 3D scanning and printing were utilised to develop a customised TMT prosthesis for a patient with a TMT amputation. The prosthesis demonstrated structural integrity and safety during the propulsion phase, as confirmed by finite element analysis. The manufacturing process involved thermoforming and the use of a TPE material, ensuring flexibility, durability, and compatibility with the user's foot.
Functional evaluations of the prosthesis included walking, running, and timed up and go tests. The results showed improvements in gait quality, symmetry, and spatiotemporal parameters when the prosthesis was used. Vertical ground reaction forces during gait resembled the normal range when the prosthesis was employed. Running performance exhibited increased symmetry and propulsion velocity with the prosthesis. The timed up and go test demonstrated reduced time and increased efficiency when using the prosthesis.
Overall, the development and functional validation of the TMT prosthesis offer a promising solution for individuals with TMT disarticulation, particularly in low-income countries with limited access to prostheses. The use of advanced technologies and a patient-centred approach contribute to improved mobility, gait patterns, and quality of life for individuals with partial foot amputations. Future research aims to evaluate additional parameters and develop new prostheses to further enhance gait improvements.
The data can be provided by the authors upon request.
The authors would like to thank the Universidad Tecnológica del Uruguay for the financial support of this work and technical support from Laboratorio Abierto, Universidad Tecnológica del Uruguay.
None.
All authors declare that they have no conflicts of interest.

©2023 Novo, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.