Journal of
eISSN: 2373-6410


Mini Review Volume 14 Issue 5
Academy of Applied Sciences Western Serbia, Uzice Department, Serbia
Correspondence: Ivanka Djuricic, MD-PhD, Academy of Applied Sciences Western Serbia, Uzice Department, Uzice, Serbia
Received: September 23, 2024 | Published: October 4, 2024
Citation: Djuricic I. What is the role of quantum medicine in the treatment of cervical spine trauma?. J Neurol Stroke. 2024;14(5):159-160. DOI: 10.15406/jnsk.2024.14.00600
The article covers the successful treatment of cervical spine trauma using quantum therapy. It introduces a new treatment therapy that uses quantum medicine bioresonance apparatus. The case study in this article describes the case of an adult diagnosed with herniated disc who suffered the cervical spine trauma in a car accident, whose condition improved significantly after several quantum therapies.
Keywords: herniated disc, cervical spine trauma, common treatments, quantum therapy, effects of the quantum medicine treatment, recovery
The bones (vertebrae) that form the spine in the back are cushioned by discs. These discs are round, like small pillows, with a tough, outer layer (annulus) that surrounds the nucleus. Located between each of the vertebra in the spinal column, discs act as shock absorbers for the spinal bones. A herniated disc (also called bulged, slipped or ruptured) is a fragment of the disc nucleus that is pushed out of the annulus, into the spinal canal through a tear or rupture in the annulus (a nucleus pulposus is displaced from intervertebral space). Discs that become herniated usually are in an early stage of degeneration but can often be caused by a physical trauma to the spine. The spinal canal has limited space, which is inadequate for the spinal nerve and the displaced herniated disc fragment. Due to this displacement, the disc presses on spinal nerves, often producing pain, which may be severe. Herniated discs can occur in any part of the spine. Herniated discs are more common in the lower back (lumbar spine), but also occur in the neck (cervical spine). The area in which pain is experienced depends on what part of the spine is affected.1
This article covers the case of a 52-year-old male patient. The patient in case was in a car accident (drove a motor vehicle) in which he injured his cervical spine (vertebrae C3/C5). He had been diagnosed with herniated disc in the cervical spine region (vertebrae C5/C6) before his accident (Figure 1). Due to his diagnosis, he had suffered from occasional physical pain and neck stiffness. The crash only caused the physical trauma to the already existing disc herniation, significantly worsening its condition.
Immediately after the accident the patient noticed that he could not drive the vehicle, that is, he could not move his legs and arms. He was taken to a hospital, where a CT scan was performed. It showed the existence of a herniated disc, without visible bone trauma. The neurological findings suggested quadriparesis of medium degree, dominant/pronounced on the hands with hyperesthesia. Hyperesthesia is defined as an increased cutaneous sensitivity manifesting as stimulus-dependent neuropathic pain. While most neuropathic pain symptoms are contained within the dermatomal distribution of the affected nerve, hyperesthesia has been known to extend beyond the affected nerve’s distribution.2 In this case, the patient could not hold a bottle of water – he felt pain/sensitivity to touch. The patient was then referred to another health facility where he underwent an MR scan examination of the cervical spine region. The findings showed greater prolapse of the herniated disc and marked edema of the spinal cord in the C3/C5 vertebrae region (Figure 2). Considering the clinical findings and the MRI of the cervical spine, operative/surgical treatment was suggested. Anti-edematous therapy was also recommended and prescribed, which led to an improvement in the neurological status. After 2-3 days, the patient was able to sit in bed, and after 4-5 days he stood on his feet with a walker (orthopaedic aid). Operative treatment was postponed, and the continuation of therapy followed at the Clinic of Neurosurgery at the Clinical Centre of Serbia in Belgrade. (The accident occurred while the patient was on a vacation in Greece.)
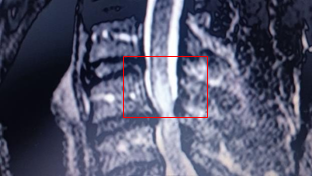
Figure 2 MRI scan after the accident showing the edema of the spinal cord in the C3/C5 vertebrae region
After returning to Uzice (patient’s hometown) from Belgrade, the treatment continues in a quantum medicine private clinic, where the BICOM bioresonance therapy was applied a number of times. After these therapies, the patient underwent rehabilitation treatment. The control MRI of the cervical spine was surprisingly better, as the edema was detected in only one point/area (Figure 3a & 3b), the clinical findings were considerably improved, the hyperesthesia reflexes were not as intense, the spasticity (i.e. the increased muscle tone) was lower than before, and the clonus, which was very pronounced, was hardly noticeable. Due to these results being significantly better than the findings of the first MRI scan, the surgical procedure was decided to be postponed until further notice.
Quantum medicine takes an important place as a complementary therapy in neurological trauma for quick and more complete recovery, as evidenced by the case in this article.
None.
The author declares that there are no conflicts of interest.

©2024 Djuricic. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.