Journal of
eISSN: 2373-6410


Case Report Volume 9 Issue 3
1Department of Neurosurgery, Hospital Guillermo Grant Benavente, Chile
2Department of Obstetrics and Gynecology, Guillermo Grant Benavente, Chile
3Department of Neurosurgery, Instituto de Neurocirugía Asenjo, Chile
4Department of Neurology, Pontificia Universidad Católica de chile, Chile
5Department of Neurosurgery, Hospital de Puerto Montt, Chile
Correspondence: Esteban Torche, Department of Neurosurgery, Hospital Guillermo Grant Benavente, Concepción, Chile, Tel + 56999974664, Fax + 56999974664
Received: April 03, 2019 | Published: June 3, 2019
Citation: Torche E, Carrillo J, Mura J, et al. Unique presentation of giant multiple meningiomas during immediate postpartum, case report and review of literature. J Neurol Stroke. 2019;9(3):159-163 DOI: 10.15406/jnsk.2019.09.00368
We report a case with presentation and diagnosis of multiple intracranial giant meningiomas after epidural anesthesia on vaginal delivery. It’s a 20 years old woman, multiparous of 2, that after placing the epidural catheter during vaginal delivery began with severe and persistent headache, confusion, drowsiness and right hemiparesis. After vaginal delivery, studies showed a giant right olfactory groove meningioma and giant left lesser sphenoid wing meningioma. A two-stage surgery was performed. A gross total resection of both tumors and complete recovery of her symptoms was achieved after surgery.
Keywords: giant multiple meningiomas, pregnancy, postpartum, neurofibromatosis
Meningiomas are nervous system tumors, first described by Harvey Cushing 1922,1 corresponding to approximately 30% of all intracranial tumors and their incidence is 6 cases per 100,000 persons per year.2,3 There are some events, such as brain radiation therapy and some diseases such as neurofibromatosis type two (NF2) or multiple endocrine neoplasia type one (MEN1) that increases its prevalence.1
NF2 is a disease caused by mutation of the tumor suppressor gene NF2 located on chromosome 22q12.2, which determines an heritable autosomal dominant tumor predisposition syndrome that leads to the development of multiple peripheral nervous system and central intracranial tumors such as meningiomas, among others.
Meningiomas occur in 50% of patients with NF2, and are generally multiple.1
Intracranial tumors diagnosed during pregnancy were described in 1898, being gliomas the first in frequency and meningiomas in second place;4 nowadays there are guidelines to establish the management of these patients according to the stage of pregnancy, tumor type, size and location, presence of symptoms and clinical signs, presence of cerebral edema and brain herniation, comorbidities, etc. It is perfectly clear that the correct approach must be multidisciplinary, involving obstetrician, neurosurgeon, neurologist and anesthesiologist.5,6
A 20years old woman, with history of two previous deliveries and family history of father with NF2, attending her third pregnancy of 37weeks, at Guillermo Grant Benavente Hospital in Concepcion, Chile. As background, she had poor adherence to controls and obstetric monitoring of her pregnancy. During vaginal delivery, after the administration of epidural analgesia pump infusion (bupivacaine + lidocaine + fentanyl), the patient presented mild headache that increased with time, reaching its peak 5hours later and started with impairment of consciousness, drowsiness, disorientation and right hemiparesis.
A Computed Tomography (CT) scans and brain magnetic resonance imaging (MRI) was performed and showed multiple intracranial meningiomas (Figure 1).

Figure 1 (A) Post-contrast MRI axial T1-weighted sequence shows giant olfatory groove meningioma and a giant left lesser wing meningioma. The tumoral masses are separated by a thin layer of brain parenchyma (black arrow). (B) T1 Gadoline enhanced sagittal MRI shows the olfatory groove meningioma. Hyperintense to grey matter and extends anteriorly along the anterior cranial fossa floor. (C,D) T1 Gadoline enhanced coronal MRI illustrates the important mass effect on the anterior and medium skull base, secondary to giant meningiomas and the brain herniation. C: The tumor cause the collapse and superior displacement of the left temporal horn (black arrow).
A giant meningioma of the right olfactory groove measuring 7cm x 6cm x 5.2cm (Figure 1); a left giant lesser sphenoid wing meningioma measuring 7cm x 6.5cm x 4.8cm (Figure 2); both tumors producing significant edema and brain herniation (Figures 1&2). Small bilateral vestibular schwannomas, two small falx meningiomas and a cervical schwannoma from C1 to C3 (Figure 3).
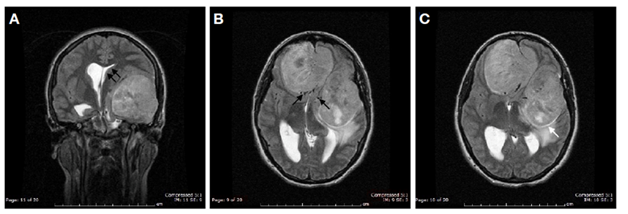
Figure 2 (A) T1 Gadoline enhanced sagittal MRI demonstrate the olfatory Groove meningioma. Hyperintense to grey matter and extends anteriorly along the anterior cranial fossa floor. (B,C) Axial T2-weighted sequence MRI demonstrates the important mass effect and ventricular compression due to the giant meningiomas. It also highlights the normal arteries involved (Black arrows).
The case was submitted to the vascular and skull base surgery team, which decided to begin removing the intracranial meningiomas first and then perform the surgical removal of the upper cervical spine lesions, due to the patient's state of consciousness and cerebral herniation. Cranial surgery was performed in two stages. First, the meningioma of the olfactory groove, operated without incidents, using a transbasal approach. 48hours after surgery, the patient was extubated and evolved without neurological deterioration. One week later, the meningioma of the left minor sphenoid wing was operated by left pterional approach, with no complications. Total resection was achieved with grade 1 of Simpson scale.7
The results of both biopsies were positive for a grade I of WHO classification: fibroblast meningioma. Postoperative CT showed satisfactory extirpation of both tumors, improvement of midline displacement, and disappearance of the cerebral hernia.
One week after the surgery, the patient evolved without neurological deficit and demanded medical discharge, knowing the risks of her decision. As a result, cervical surgery could not be performed. She didn’t attend to any outpatient postoperative neurosurgery controls.
After one year, the patient is reached and a cerebral MRI is performed, which showed a total resection of her two giant meningiomas, without recurrence (Figures 4&5). Neck lesions in situ. The patient refused cervical surgery knowing the possible risks of her decision.
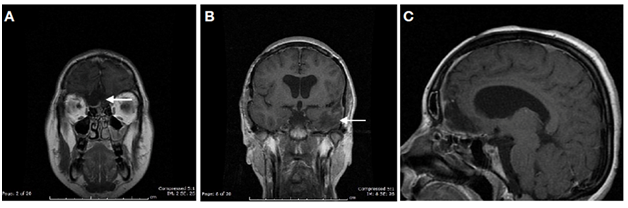
Figure 4 (A,B,C) Postoperative T1 Gadoline enhanced coronal and sagittal MRI shows complete resection of olfatory grove meningioma and left sphenoidal meningioma. White arrows show the place where the tumors were previous to surgical resection.

Figure 5 (A-D) Postoperative T1 Gadoline enhanced axial MRI shows complete resection of both large meningiomas and no ischemic sequelae.
Discussion
The reported incidence of intracranial tumors in pregnant women is approximately 7 x 125,000 pregnancies, being the glioma the first in frequency,4,8 and specifically in the case of meningiomas, the incidence is of 1-4.5 per 100,000 pregnancies.
Some authors support that the number of tumors that become symptomatic during pregnancy is lower than those of non-pregnant women of the same age.2 Other authors support that symptoms may appear and worsen during pregnancy.5,9
Meningiomas can grow during pregnancy, especially in its second half.4 The mechanisms involved are not fully understood and the present factors are, among others, fluid retention, intra- and extracellular edema, vessel congestion, increased vascularity, increased body mass index (BMI)3 and increased hormones, especially prolactin and estrogen.5,4,10
Meningiomas express receptors for different hormones, among them: androgens, progesterone, estrogen, placental growth factor and others.6 Progesterone receptors can be found in 70% of meningiomas and estrogen receptors in 30%.11 Another factor supporting the hormonal theory is that patients with oophorectomy and menopause have less risk on developing meningiomas.11 Therefore, as it has been reported in the literature, tumor size and symptoms may decline after birth.4
Kerschbaumer et al.9 Reported a 39-week pregnancy case with a 5cm sphenoidal meningioma, elective surgery was scheduled two months after birth and the tumor reduced its size by 50%. Meningiomas sensitive to hormones may shrink after delivery. Therefore, deferred surgery a few months after birth is an option, and may facilitate resection.9
Patients with positive tumor markers for progesterone show decreased rate of tumor recurrence after resection.12 Some authors have tested progesterone receptor antagonist RU-486 for the treatment of meningiomas, showing promising results in patients with high progesterone receptor density in tumor tissue13 and also in multiple meningiomas.
Our case’s presentation symptom was headache after epidural anesthesia. The headache progressively increased until reaching its peak in 5hours, with the addition of alteration of consciousness and right hemiparesis. Transient neurologic complications have been reported in 18.9 out of 10,000 births, which may be associated with epidural anesthesia.
Hari Krovvy et al. reported a case of a 33-year-old woman with a 36-week pregnancy. 24hrs after epidural anesthesia showed isolated weakness of the left leg, and after studies showed a large cystic meningioma of the parietal region and a second meningioma in front of the quadrigeminal plate. The patient started with hypertension, bradycardia and drop on Glasgow coma scale, reaching 8 points. Surgery was performed, but persisted with paralysis and developed visual impairment after it.14 To our knowledge, this is the first case reported in literature with this presentation.
In this case, the patient did not regularly attend to pregnancy checks and had no prior brain studies to evidence intracranial meningiomas associated with edema, mass effect, and cerebral hernia. Without this information, an epidural anesthesia was performed. It is known that management of pregnant women with intracerebral lesions is multidisciplinary and the importance of the anesthetic decision at the time of delivery and/or cesarean.
Spinal anesthesia may cause cerebrospinal fluid (CSF) leakage and lead to severe morbidity or mortality in the context of an intracranial mass-effect lesion. Uterine contractions, secondarily increases intracranial pressure.15 Some authors claim that this would be even more noticeable in the second stage of childbirth.8
Several authors have attempted to make guidelines for management of intracranial meningiomas in pregnant women.5,6 All agreed that the most important factor for good surgical outcomes was multidisciplinary management with obstetricians, anesthesiologists, neurosurgeons and neurologists. The treatment will depend on the course and the stage of pregnancy, and should be adapted individually to each case. We agree with Al-Mefty5 that in the first trimester surgery should be avoided unless mother's life or a major function is at risk, in order to not endanger the fetus. Some authors support that surgery could be performed without increasing the risk for the fetus.6
In the second trimester, surgery is supported when there is increased intracranial pressure or significant neurological deficit. In the third trimester, one may proceed with childbirth or brain surgery depending on disease progression or fetal need.5,16 At any sign of increased intracranial pressure, vaginal delivery should be avoided. Sekhar, supports that surgery should be performed at an early stage in patients with progressive visual impairment to achieve better visual outcomes, since no improvement is achieved in patients with advanced visual impairment.5
Other factors to consider include: suspected malignant lesions, presence of hydrocephalus requiring shunt, progressive neurological involvement or signs of cerebral hernia that require urgent surgery.5,6,12 Neuroanesthesia should consider both maternal and fetal factors, and in general terms, valsalva, hypotension, hypovolemia and hypoxia should be avoided.11
Perry et al. reported 17 cases of meningioma in pregnant women, 16 were operated and one case died before surgery secondary to the mass effect. In this case, an autopsy revealed a large (6 x 3.5cm) edematous-appearing olfactory groove/tuberculum sellae meningioma with associated diffuse cerebral edema and bilateral uncal as well as tonsillar herniation. Most patients became neurologically symptomatic at the mid to late stages of pregnancy. Three patient’s (18%) presentation were in their first trimester, 5 (29%) during the second, and 7 (41%) during the third. Two patients became neurologically symptomatic post-partum, 8 days within delivery. Principle physical findings in these patients included visual impairment in 10 cases (59%) and cranial nerve palsy in 5 (29%). 4 patients developed new onset seizures, increased frequency of seizures, or massive cerebral edema requiring urgent neurosurgical attention.17 No case presented neurological symptoms during delivery, as in our case.
Kurdoglu et al. reported a case of a 41-year-old woman with a 39-week pregnancy and a large meningioma of the olfactory groove with mass effect and cerebral herniation. Due to neurological and visual problems, surgical resolution was decided. First, they performed a cesarean section and then the cranial surgery. The patient on the third postoperative day died from persistent hypotension.4 In our case a complete resection, Simpson grade 1 of both meningiomas was achieved. The patient presented complete remission of his symptoms, without neurological sequelae due to the early surgical resolution.
In our case the patient had NF2 and they were diagnosed bilateral vestibular schwannomas, cervical schwannoma (C2-C3) and multiple meningiomas. Half of patients with NF2 have medullary lesions. We agree with Aboukais18 that management of patients with NF2 and multiple tumors is very complex and surgery is the primary treatment, but there is an emerging role in drug therapies. Each decision must be evaluated for each particular case and clinical and radiological cranial and spinal follow-up should be performed to assess tumor progression and to propose any surgical treatment before neurological disorder appears.18
Due to poor patient adherence, and her demand for medical discharge, it was not possible to perform surgery on his spinal lesion. She didn`t show up to any postoperative control. One year later the patient was reached, confirming her good condition, without neurological deficit. Brain and cervical spine MRI showed complete resection of the operated meningiomas.
The authors declare that there is no conflict of interest regarding the publication of this paper.
We would like to thank the secretaries of our Department of Neurosurgery of Guillermo Grant Benavente Hospital, Concepción: María Isabel Reyera and María Raquel Sánchez for their great help and dedication to our patients. And especially Daniela Fierro, our nurse who incessantly calls our patient and family, due to she’s bad adherence to clinical controls.
All authors certify they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers' bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Informed consent was obtained from all individual participants included in the study.

©2019 Torche, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.