Journal of
eISSN: 2373-6410


Case Report Volume 9 Issue 2
Neurosurgery Department, “Dr. Manuel Quintela” Clinical Hospital, Republic University, Montevideo, Uruguay
Correspondence: Maria Veronica Bentancourt, Neurosurgery Department, “Dr. Manuel Quintela” Clinical Hospital, Republic University, Montevideo, Uruguay
Received: February 27, 2019 | Published: April 2, 2019
Citation: Bentancourt MV, Romero M, Martinez F. Temporal lobectomy in patients with malignant stroke and raised intracranial pressure after decompressive hemicraniectomy. J Neurol Stroke. 2019;9(2):81-84. DOI: 10.15406/jnsk.2019.09.00352
Introduction
Malignant stroke corresponds to 5% of ischemic cerebrovascular disease and it was named due to the high mortality with medical therapy. It is defined by symptoms suggesting stroke of the middle cerebral artery territory, the evolution into a progressive decrease in consciousness level of the patient and a computed tomography that show a stroke which affect at least 50% of middle cerebral artery territory or a volume greater than 145 cc in magnetic resonance.
Case report
Three patients with a middle cerebral artery territory stroke, who underwent a decompressive hemicraniectomy in the first 48 hours after the onset of symptoms and posteriorly needed a temporal lobectomy as a life-saving procedure, are reported.
Discussion
Malignant stroke has a mortality of 70 to 80% with medical therapy. Decompressive hemicraniectomy addition reduce mortality to 20 - 30% and enhance a better functional prognosis. Some authors suggest that the resection of non-viable brain tissue as the first treatment or when the decompressive hemicraniectomy is not enough diminish even more the mortality and provide a better prognosis. In the patients presented, temporal lobectomy when raised intracranial pressure appeared, even after decompressive hemicraniectomy, proven to reduce the mortality.
Conclusion
Temporal lobectomy is not a routinely procedure in patients with malignant stroke, but it can be useful in selective patients in whom the decompressive hemicraniectomy in not enough to reduce intracranial pressure.
Keywords: Malignant stroke, decompressive hemicraniectomy, strokectomy, temporal lobectomy
Cerebrovascular disease is the second cause of death in the world according to the World Health Organization.1,2 Lifestyle changes and the population aging have determined an increase in the prevalence of risk factors for cardiovascular and cerebrovascular disease. Malignant stroke corresponds to 5% of ischemic cerebrovascular disease. This term was used for the first time by Hacke in 1996 and arises as a result of the death of 78% of patients in the cited study, by uncal o transtentorial herniation around the fifth day of stroke.3
Currently we can define malignant stroke using the criteria mentioned in the trials carried out so far. According to this, we can divide them into clinical, evolutionary and imaging criteria. Clinically, it imply symptoms installation of the middle cerebral artery (MCA) territory and evolution into a progressive decrease in patient level of consciousness associated with edema. The imaging criteria imply, a suggestive ischemia images of at least 50% of the territory of the MCA or a volume greater than 145 cc in the diffusion sequence of magnetic resonance.4–11
Even with the decompressive hemicraniectomy introduction, 30% of patients will die as a consequence of uncal o transtentorial herniation.4-11 Other treatments have been mentioned in the literature with little scientific evidence. Three patients with MCA territory strokes in which the decompressive hemicraniectomy was not enough and a temporal lobectomy was performed, are presented.
Case 1
A 59 years female, with a personal history of obesity and hypertension, suddenly installed a left hemiparesis. She was admitted to hospital with 15 points in the Glasgow Coma Scale (GCS), without symptoms of raised intracranial pressure and with a left hemiplegia. Brain computed tomography (CT) scan confirmed right MCA ischemic stroke. Intravenous fibrinolytic were administered. The arteriography was performed 9 hours after the installation of symptoms so it was decided not to proceed with mechanical thrombectomy.
24 hours after the symptoms started, a patient with 12 points in the GCS was observed. The CT scan showed a configured ischemia in all MCA territory, which determined homolateral ventricular system compression. A decompressive hemicraniectomy of more than 12 cm length was performed. The patient remained in intensive care unit, intubated, reaching 11 points in the GCS (awake, obeying orders, without verbal response), with a CT scan that showed improvement in mass effect. The intracranial pressure monitoring device was taken out after 48 hours of registers under 20 mercury millimeters (mmHg).
On the fourth day after symptoms onset, the patient depressed consciousness again and installed bradycardia and arterial hypertension. Brain CT scan showed a more configured stroke that caused ventricular system compression and one centimeter midline deviation. In order to reduce undamaged brain tissue compression and diminish intracranial pressure (ICP), a right temporal lobectomy was performed. The infarcted tissue was resected up from the temporal tip to 5 centimeter behind it and in depth up to the arachnoid that separates us from the ambiens cistern. The brain control CT confirmed mass effect improvement (Figure 1). The subsequent evolution was good. One year after surgery the patient is having a plegia of the left upper limb and severe paresis of the lower limb with assistance need for daily life activities (mRS of 4).
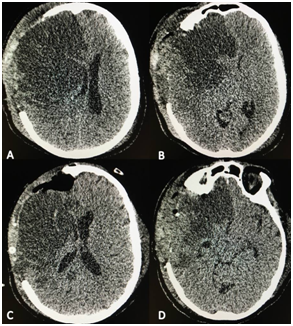
Figure 1 A & B: Computed tomography previous to de temporal lobe resection showed the area of stroke as an hypodense area which compression of the homolateral ventricular system, severe midline shift and contralateral hydrocephalus. C & D: Computed tomography after the temporal lobe resection which showed improvement in the mass effect and the absence of complications.
Case 2
A 36 years male, with no medical history, the night before admission abruptly installed a transitory aphasia and paresis in the right lower limb. The next day he suddenly developed an aphasic mutism and right hemiplegia. Brain CT scan showed a hyperdense middle cerebral artery and differentiation loss between gray and white matter. Intravenous fibrinolytic were administered, but symptoms did not improve.
48 hours after admission he started with mild consciousness depression. The brain CT scan was repeated, showing more configured MCA territory ischemia, which determined ipsilateral ventricular compression and 5 millimeter midline deviation. An emergency decompressive hemicraniectomy was performed and a subdural catheter was placed to record ICP. He was transferred to an intensive care unit where he remained intubated and the control CT showed a clear improvement in mass effect.
On the fifth day after admission, the patient installed a left mydriasis, with ICP lower than 15. The brain CT showed frank increase in the hypodense area with severe mass effect. We performed a temporal lobectomy up to 5 centimeter behind the temporal tip reaching in depth the arachnoid that separates us from the ambiens cistern. In the immediate postoperative period the mydriasis receded and ICP registers were low. One month after surgery, the patient managed to walk with help, communicating with isolated words (mRS 3).
Case 3
A 46 year-old male with a medical history of hypertension without treatment and smoking, had an abrupt right hemiparesis and aphasia. He was awake, fulfilling orders and communicated with isolated words, adding 13 points in the GCS. He presented a right hemiplegia. Brain CT confirmed a left MCA ischemic stroke. Intravenous fibrinolytic were administered and arteriography made diagnosis of carotid dissection that could not be treated. After the procedure the patient depressed consciousness, so brain CT was repeated. It showed a more configured area of ischemia which caused homolateral ventricular system compression and 6 millimeter midline deviation. A decompressive hemicraniectomy was performed and a subdural catheter was placed to register ICP. The control CT confirmed mass effect improvement and absence of postoperative complications.
On the third day, the patient started with ICP records higher than 20 mmHg that were refractory to medical treatment. Brain CT showed a frank increase of the hypodense area in the left MCA territory with mass effect increase, given by compression of the ventricular system and a 8 millimeter midline deviation. Infarcted left temporal lobe was resected with the same limits as in the previous cases. The control CT showed improvement of the mass effect (Figure 2). After two months of evolution, the patient was awake, fulfills orders and presented anomies in the naming of objects that allow him to communicate with difficulty. He continued with right hemiplegia. We managed to retired the tracheotomy and gastrostomy and remained with rehabilitation (mRS 5).
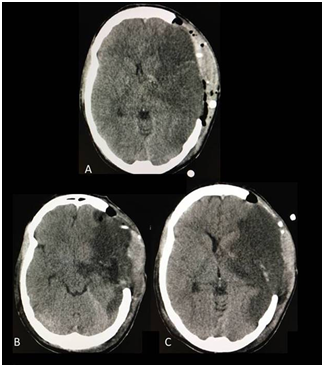
Figure 2 A) CT scan before the temporal lobectomy. The stroke is observed as a hypodense area which produced compression in the ventricular system and midline shift. B & C The CT scan after the temporal lobectomy showed absence of complications and an improvement in the mass effect with restoration of the midline.
The high mortality of patients with a malignant stroke, despite an excellent neurocritical treatment, has led to discuss the usefulness of surgical techniques with the aim of improving the vital prognosis and “saving brain function”. In stroke, intracranial pressure monitoring has not shown utility to decide the opportunity of surgery. It has been demonstrated that patients with clinical and tomographic signs of uncal herniation show no increase in ICP (higher than 20 mmHg) when it is monitored.12 Despite this, its monitoring in the postoperative period allows to predict complications related to surgery and if it is high to perform an adequate medical treatment. Despite this, its monitoring in the postoperative period allows to predict complications related to surgery and if it is high to perform an adequate medical treatment.
In all three cases, intracranial pressure was not monitored in the preoperatory. Clinical and tomographic criteria where used to decide decompressive hemicraniectomy. In case 2, the previously mentioned is verified. Despite the mydriasis presented by the patient in the postoperatory, midline deviation and uncal herniation in the CT, the ICP registers are low. In case 3, however, the ICP records and CT findings are compatible.
After obtaining the results of several controlled trials conducted in recent years, the benefits of decompressive hemicraniectomy in the treatment of malignant stroke have been demonstrated.6–8,10, 11 Two meta-analyzes carried out that gather the results of the three European controlled clinical trials, showed a reduction in mortality from 70% in patients undergoing conservative treatment, to 20% in those in whom decompressive hemicraniectomy was performed.4,9 A functional improvement was also demonstrated in those patients treated surgically. It is verified that decompressive hemicraniectomy increases 30% patients with mRS 4,10% patients with mRS 2 and 3, however, there was no significant change with mRS 5. There is no doubt that these benefits are maintained even in patients with stroke in the dominant hemisphere.4,9
The best opportunity for performing decompressive hemicraniectomy is in the first 48 hours. The HAMLET study showed that in patients treated in this lapse of time with surgery, there is a difference in mortality of 50% with respect to conservative treatment, but in those operated after 48 hours, the mortality improvement was lower than 10%.4,6 There are factors that allow us to predict whether decompressive hemicraniectomy will be sufficient in patients with malignant stroke. These include the stroke volume greater than 200 cc and more than one vascular territory involvement.13–18
In the three patients mentioned, the decompressive hemicraniectomy was performed regardless of the affected cerebral hemisphere, in the first 48 hours after symptoms onset. This was done maintaining a 12 - 14 centimeter craniectomy diameter, which is the optimal diameter for an adequate brain expansion without increasing complications and with dural patch addition. None of the three patients presented elements that allow us to suspect in advance that decompressive hemicraniectomy could not be enough. We emphasize that cases 2 and 3 were young patients, with grater brain volume, so that tolerance to cerebral edema is lower.
Some authors have proposed the resection of non-viable parenchyma in patients with stroke, either as a first treatment or when decompressive hemicraniectomy is insufficient. As published by Kostov D et al.19 the functional prognosis is better in patients undergoing a strokectomy compared with an isolated decompressive hemicraniectomy.19 Kalia K et al.20 found similar results with the resection of non-viable parenchyma as a first measurement to those obtained with decompressive hemicraniectomy.20 Schwake M et al.18 states that in patients in whom decompressive hemicraniectomy is insufficient to prevent raised ICP, nonviable tissue resection reduces the mortality to 10% without changing functional prognosis.18
In the cases we have analyzed, in no patient it was opted for non-viable brain tissue resection as the first option. The three patients have in common the appearance of symptoms of raised ICP plus the visualization on the CT of a midline shift greater than 1 cm or a herniation of the brain parenchyma, between 3 and 5 days after the symptoms onset. In all three patients, it can be affirmed that the surgical treatment initially performed is insufficient and that the absence of another surgical procedure carries a high risk of death. This was assumed because of the registers of ICP higher than 20 mmHg, clinical symptoms of uncal herniation (pupillary dilatation) or TC findings in spite of the decompressive hemicraniectomy. Following these reasoning and as an exceptional measure, a temporal lobectomy was performed, resecting the non-viable brain tissue from de temporal tip to 5 cm behind it and in depth until the arachnoid that limited with the ambient cistern. It was never necessary to resect all the non-viable brain tissue of the stroke. The non-viable tissue was recognized for the hypodense area measured in the CT scan and intraoperative findings. There were no complications related to this procedure in any cases.
Mortality after temporal lobectomy was null, which is consistent with Schwakw M et al.18 proposal. Functionally, we do not consider that temporal lobectomy has aggravated the prognosis, and the existing sequels are associated with the territory of stroke.
Malignant stroke is an illness with high mortality if only medical treatment is provided. The addition of a decompressive hemicraniectomy reduces the mortality dramatically but, still 20 to 30% of the patients die as a consequence of raised ICP. We have presented three cases of patients in whom the decompressive hemicraniectomy was insufficient and the resection of non-viable temporal lobe tissue proved to be life-saving without aggravating functional outcome. We emphasize that is not a routinely procedure, but it could be useful in selective cases.
None.
Authors declare no conflicts of interest.

©2019 Bentancourt, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.